Title page Type of manuscript: Case report Title of the study
advertisement

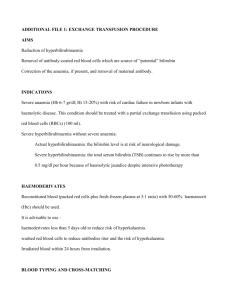
Title page Type of manuscript: Case report Title of the study: Elevated IgG causing spurious elevation in serum Total bilirubin assay Total number of authors: Four Authors: 1. Kriti Singh, MD postgraduate student, Department of Biochemistry, Kasturba Medical College, Manipal University, Manipal- 576104, Karnataka Phone: 9886815540, Email: drskriti@gmail.com 2. Pragna Rao, Professor and Head, Department of Biochemistry, Kasturba Medical College, Manipal University, Manipal- 576104, Karnataka Phone: 0820-2922326, Email: drpragnarao@gmail.com 3. Priyanka Datta, MD postgraduate student, Department of Biochemistry, Kasturba Medical College, Manipal University, Manipal- 576104, Karnataka Phone: 9742151074, Email: dattapriyanka12@gmail.com 4. Vijetha Shenoy Belle, MD postgraduate student, Department of Biochemistry, Kasturba Medical College, Manipal University, Manipal- 576104, Karnataka Phone: 9844667820, Email: vijethashy@gmail.com Declaration To, The Editor Asia Pacific Journal of Research, I hereby declare that the Case report titled ”Elevated IgG causing spurious elevation in serum Total bilirubin assay” has not been submitted or published elsewhere. Dr. Kriti Singh MD postgraduate student Department of Biochemistry Kasturba Medical College Manipal University Manipal – 576104 Karnataka India. Phone: 9886815540 Email: drskriti@gmail.com Elevated IgG causing spurious elevation in serum Total bilirubin assay Abstract Introduction: Monoclonal gammopathy is characterized by the presence of an M-protein that has homogeneous structural and functional properties. At very high concentrations it may cause significant interference in clinical chemistry assays. Incidence of interference in total bilirubin measurement is described in this study. Methodology: A 43 years old diabetic female, known case of multiple myeloma of 6 years, on chemotherapy, presented to OPD. Routine tests were inconspicuous except for elevated total bilirubin and globulins. Liver enzymes were normal. Total bilirubin estimation was done by diazonium ion method. Result: Repeat testing after dilution of sample revealed normal total bilirubin. Discussion: Paraprotein interference with the Roche automated total bilirubin assay is caused by precipitate formation which may cause clinical confusion. If false elevation of total bilirubin is suspected the laboratory should measure total bilirubin using a different method. Conclusion: The increase in serum total bilirubin of the patient was due to interference in the assay caused by high IgG levels of the patient. Every laboratory should be able to identify such incidences and have a standardized method to overcome the interferences. Sample dilution or precipitation of interfering substances can overcome the interference. Keywords: Clinical biochemistry, Interferences, Gammopathy, Hemolytic index, Multiple Myeloma, Total Bilirubin Introduction: Paraproteinemia can cause false elevations in total and direct bilirubin levels (Smogorzewska A et al 2004, Chung et al 2005). These occurrences are not just limited to bilirubin. Interference in the measurement of serum total bilirubin by Roche Cobas 6000 auto analyzer, in a patient of multiple myeloma is described in the subsequent sections. Case Description: A 43 years old diabetic female, known case of multiple myeloma of 6 years, on chemotherapy, presented to oncology OPD, with complaints of headaches and cough for a week. At the time of admission the patient was on progression phase of Bortezomib, Cyclophosphamide and Dexamethasone (VCD) protocol. She was not receiving any treatment for diabetes except dietary restrictions. The patient received a cycle of VCD chemotherapy on day 2 of admission and an episode of plasmapheresis on day 5 of admission. Laboratory investigations done on the day of admission are represented in Table 1. Table 1: Laboratory reports from day one of admission Samples Patient sample Reference ranges Day of admission - 25.7 0.2-1 0.3 0- 0.2 AST (IU/L) 35 15- 40 ALT (IU/L) 24 15- 40 ALP (U/L) 40 Total Proteins (g/dL) 12.6 6- 8 Albumin (g/dL) 3.6 3.5- 5.5 Globulin (g/dL) 9.0 2.5- 3.5 Na+ (mEq/L) 138 135- 145 K+(mEq/L) 4.0 3.5- 5.5 Urea (mg/dL) 32 20- 40 Creatinine (mg/dL) 1.0 0.6- 1.2 SPE M band in γ region - Serum Immunofixation IgG and λ bands - Serum IgA (mg/dL) <14 70-400 Immunoglobulins IgG (mg/dL) 6610 700-1600 IgM (mg/dL) 22 40-230 Complete blood Hb (g/dL) 12.2 12-15 counts RBC 4.9 x 106 4.2 – 5.4 x 106 WBC 12,800 11,000- 14,000 Tests Time of collection Total bilirubin (mg/dL) Direct bilirubin LFTs Electrolytes RFTs (mg/dL) Legend: AST- Aspartate Aminotransferase, ALT- Alanine Aminotransferase, ALP- Alkaline Phosphatase, LFTs- Liver function tests, RFTs- Renal function tests, SPE- Serum protein electrophoresis, IgA- Immunoglobulin A, IgG- Immunoglobulin G, IgM- Immunoglobulin M, Hb- Hemoglobin, RBC- Red blood cells, WBC- White blood cells Clinically, the patient was not jaundiced, and there was no supporting evidence for liver disease. From Table 1, it is evident that apart from serum total bilirubin (25.7 mg/dL) and serum globulins (9 g/dL) no other abnormality is seen in the patient sample. In vitro hemolysis as a potential interfering factor was ruled out by estimating the H index which was within acceptable range. The only interfering factor in this case was elevated serum IgG levels of 6610 mg/dL (Reference range: 700-1600). Repeat total bilirubin estimation was done after diluting the sample in a ratio of 1:50. The total bilirubin level was then found to be 0.8 mg/dL Another sample sent on day six of admission after an episode of plasmapheresis showed following findings (Table 2) Table 2: Laboratory reports from day six of admission Samples Patient sample Reference ranges Day 6 of admission - 0.5 0.2-1 0.3 0- 0.2 AST (IU/L) 18 15- 40 ALT (IU/L) 25 15- 40 ALP (U/L) 88 Total Proteins (g/dL) 9.3 6- 8 Albumin (g/dL) 2.9 3.5- 5.5 Globulin (g/dL) 6.4 2.5- 3.5 Na+ (mEq/L) 133 135- 145 K+(mEq/L) 3.9 3.5- 5.5 Urea (mg/dL) 28 20- 40 Creatinine (mg/dL) 0.9 0.6- 1.2 SPE - - Serum Immunofixation - - Serum IgA (mg/dL) - 70-400 Immunoglobulins IgG (mg/dL) 2875 700-1600 IgM (mg/dL) - 40-230 Complete blood Hb (g/dL) 12.4 12-15 counts RBC 5.0 x 106 4.2 – 5.4 x 106 WBC 12,400 11,000- 14,000/ μL Tests Time of collection Total bilirubin (mg/dL) Direct bilirubin LFTs Electrolytes RFTs (mg/dL) Legend: AST- Aspartate Aminotransferase, ALT- Alanine Aminotransferase, ALP- Alkaline Phosphatase, LFTs- Liver function tests, RFTs- Renal function tests, SPE- Serum protein electrophoresis, IgA- Immunoglobulin A, IgG- Immunoglobulin G, IgM- Immunoglobulin M, Hb- Hemoglobin, RBC- Red blood cells, WBC- White blood cells. From Table 2, after plasmapheresis, serum IgG level reduced to 2875 mg/dL along with a reduction in serum total bilirubin to 0.5 mg/dL. All chemistry parameters were estimated using standard traceable assays in Roche Cobas 6000 auto analyzer. Sample used was plain serum collected in a red capped evacuation tube. Total bilirubin estimation was done by diazonium ion method (Jendrassik L et al. 1938) Immunofixation was done using Helena Biosciences SAS MX Immunofix apparatus which includes gel electrophoresis followed by immunoprecipitation and staining. Serum protein electrophoresis was done using Helena biosciences SAS MX serum protein technique setup using Tris- barbital buffer system (pH- 8.6). Hemolytic index of both the patient samples was measured in Roche COBAS c501 subunit (cut off <60 mg/dL of free Hb i.e. visible hemolysis) (Salvagno GL et al, 2012). It was found to be within acceptable range in both the patient samples. Furthermore, the normal haemoglobin levels in both the patient samples (12.2 g/dL and 12.4 g/dL) along with normal RBC counts excluded in vivo hemolysis. Another point to be noted here is that the patient’s serum globulin levels were 9g/dL initially on day 1. After plasmapheresis, serum globulin levels reduced to 6.4 g/dL. Discussion: Interference is defined as "the effect of a substance present in the sample that alters the correct value of the result for an analyte" (Pantanowitz L et al, 2003). The paraproteinemia consistent with multiple myeloma (Saibaba KSS et al, 1998) is known to interfere with estimation of several parameters especially where the mode of measurement employs photometric or turbidimetric assays (Smogorzewska A et al. 2004, Puppalwar P. V 2012, Alexander D. D 2007). This interference is due to precipitation of these paraproteins in the reaction mixture causing turbidity and thereby increasing absorbance at every wavelength due to scattering of light. The Roche total bilirubin assay is a 1-cuvette, 2-point end point assay. The addition of R2 to the reaction mixture changes the assay environment to an acidic pH of 1–2, which precipitates paraproteins causing the interferences (Dimeski G 2008). Smogorzewska et al (2004) hypothesized that the Roche solubilising agent is in fact the cause of this artefact. The direct bilirubin assay shows no such interference. In our patient a fall in serum IgG levels coincided with fall in total bilirubin levels. This indicates that the cut-off levels of IgG that interfere with total bilirubin measurements may fall somewhere in the range of 2000-3000 mg/dL, but this is our hypothesis and warrants further analysis. A possible factor leading to an actual increase in total bilirubin could have been the long term chemotherapy, as literature states that lenalidomide and bortezomib may have adverse effects on liver functions (Coehn M.A 1970, Drug safety update 2013, Jollift CR et al 1982, Smith AF et al 2006). But the patient had no such clinical features. Hydration status of the patient is another cause for fluctuations in bilirubin levels (Cornelis T et al 2012). However, an elevation in serum total bilirubin due to dehydration would coincide with an increase in other parameters such as urea, creatinine and red cell indices. Routine clinical chemistry assays are designed keeping in mind that proteins, normal or otherwise, should not interfere with their values. However, when the monoclonal antibodies proliferate to a significant degree the “precipitation becomes relevant and influences the assay” (Canadian Paediatric Society Statement 1999). Proteins are least soluble at their isoelectric point. At this pH their net charge is zero, causing low electrostatic repulsion. Precipitation can be significantly reduced by adding surfactants to impair hydrophobic interactions, and by modifying the pH to increase electrostatic repulsion between individual M-protein molecules (Bakker AJ 2007). Because dispensing correct reports is of utmost priority for any laboratory it is imperative that every laboratory has a standardized protocol to combat interferences. While we applied dilution as a corrective technique, precipitation of interfering factors can also be performed (Canadian Paediatric Society Statement 1999, Bakker AJ 2007). It is up to the concerned laboratory to come up with suitable measures for correction. References: Alexander, DD., Mink, PJ., Adami, H., Cole, P., Mandel, J.S., Oken, M.M. et al (2007) ‘Multiple myeloma: A review of the epidemiologic literature’, Int. J. Cancer, vol 120,pp. 40–61. Bakker, AJ, Mu¨cke, M. (2007) ‘Gammopathy interference in clinical chemistry assays: mechanisms, detection and prevention’, Clin Chem Lab Med,vol. 45, pp.1240–1243. Canadian Paediatric Society Statement (2009) ‘Approach to the management of hyperbilirubinemia in term newborn infants’, Paediatr Child Health, vol.4, pp.161164. Chung, G.T.Y., Chiu, R.W.K., Chan, K.C.A., Lau, T.K., Leung, T.N., Chan, L.W. et al (2005) ‘Paraprotein Interference in an Assay of Conjugated Bilirubin’, Clinical Chemistry, pp.1076-1077. Coehn, M.A., Oberman, H.A. (1970) ’Safety and long term effects of plasmapheresis’ Transfusion, vol. 10, pp. 58-66. Cornelis, T, Beckers, E.A.M., Driessen, A.L.C., Van der Sande, F., Koek, G.H.(2012) ‘Bortezomib associated fatal liver failure in a hemodialysis patient with multiple myeloma’, Clinical toxicology, vol. 50, pp. 444- 445 Dimeski, G. (2008) ‘Interference Testing’, Clin Biochem Rev, vol. 29, pp. 43-48. Jendrassik, L., Grof, P. (1938) ‘Vereinfachte photometrische Methoden zur Bestimmung des Bilirubins’, Biochem Z,vol. 297, pp. 81-89. (Original article in German) Jollift, C.R., Cost, K.M., Stivrins, P.C., Grossman, P.P., Nolte, C.R., Franco, S.M. et al. (1982) ‘Reference Intervals for Serum lgG, IgA, 1gM, C3 and C4 as Determined by Rate Nephelometry’, Clin. Chem, vol. 28 pp.126-128. Drug safety update. (2013) ‘Lenalidomide (Revlimid): Risk of serious hepatic adverse drug reactions- routine monitoring of liver function now recommended’, vol. 6. Pantanowitz, L., Horowitz, G.L., Upalakalin, J.N., Beckwith, B.A. (2003) ‘Artifactual Hyperbilirubinemia Due to Paraprotein Interference’, Arch Pathol Lab Med, vol. 127 Puppalwar, P.V., Goswami, K., Dhok, K. (2012) ‘Review on Evolution of Methods of Bilirubin Estimation’, IOSR Journal of Dental and Medical Sciences, vol. 1, pp. 1728. Saibaba, K.S.S., Bhaskar, M.V., Srinivasa Rao, R.V.L.N., Ramana G.V., Dakshinamurty, K.V. (1998) ‘Interferences in clinical chemistry analysis’, Indian Journal of Clinical Biochemistry, vol. 13, pp. 55-62. Salvagno, G.L., Lippi, G., Gelati, M., Guidi, G.C. (2012) ‘Hemolysis, lipaemia and icterus in specimens for arterial blood gas analysis’, Clin Biochem, doi:10.1016/j. Smith, A.F., Morgan, G.J., Davies, F.E. (2006) ‘Bortezomib (Velcade™) in the treatment of multiple myeloma’, Therapeutics and Clinical Risk Management, vol. 2, pp. 271–279. Smogorzewska, A., Flood, J.G., Long, W.G., Dighe, A.S. (2004) ‘Paraprotein Interference in Automated Chemistry Analyzers’, Clinical Chemistry, vol. 50.