orders for term labor and delivery
advertisement
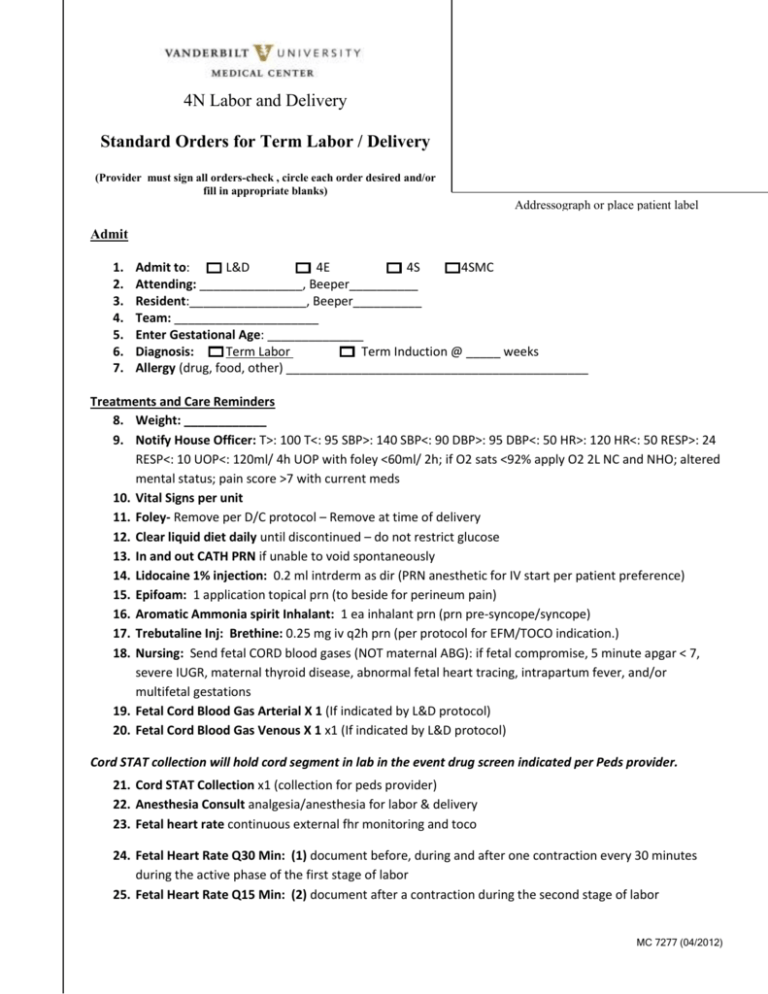
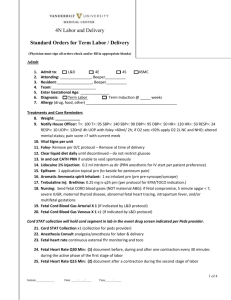
4N Labor and Delivery Standard Orders for Term Labor / Delivery (Provider must sign all orders-check , circle each order desired and/or fill in appropriate blanks) Addressograph or place patient label Admit 1. 2. 3. 4. 5. 6. 7. Admit to: L&D 4E 4S 4SMC Attending: _______________, Beeper__________ Resident:_________________, Beeper__________ Team: _____________________ Enter Gestational Age: ______________ Diagnosis: Term Labor Term Induction @ _____ weeks Allergy (drug, food, other) ____________________________________________ Treatments and Care Reminders 8. Weight: ____________ 9. Notify House Officer: T>: 100 T<: 95 SBP>: 140 SBP<: 90 DBP>: 95 DBP<: 50 HR>: 120 HR<: 50 RESP>: 24 RESP<: 10 UOP<: 120ml/ 4h UOP with foley <60ml/ 2h; if O2 sats <92% apply O2 2L NC and NHO; altered mental status; pain score >7 with current meds 10. Vital Signs per unit 11. Foley- Remove per D/C protocol – Remove at time of delivery 12. Clear liquid diet daily until discontinued – do not restrict glucose 13. In and out CATH PRN if unable to void spontaneously 14. Lidocaine 1% injection: 0.2 ml intrderm as dir (PRN anesthetic for IV start per patient preference) 15. Epifoam: 1 application topical prn (to beside for perineum pain) 16. Aromatic Ammonia spirit Inhalant: 1 ea inhalant prn (prn pre-syncope/syncope) 17. Trebutaline Inj: Brethine: 0.25 mg iv q2h prn (per protocol for EFM/TOCO indication.) 18. Nursing: Send fetal CORD blood gases (NOT maternal ABG): if fetal compromise, 5 minute apgar < 7, severe IUGR, maternal thyroid disease, abnormal fetal heart tracing, intrapartum fever, and/or multifetal gestations 19. Fetal Cord Blood Gas Arterial X 1 (If indicated by L&D protocol) 20. Fetal Cord Blood Gas Venous X 1 x1 (If indicated by L&D protocol) Cord STAT collection will hold cord segment in lab in the event drug screen indicated per Peds provider. 21. Cord STAT Collection x1 (collection for peds provider) 22. Anesthesia Consult analgesia/anesthesia for labor & delivery 23. Fetal heart rate continuous external fhr monitoring and toco 24. Fetal Heart Rate Q30 Min: (1) document before, during and after one contraction every 30 minutes during the active phase of the first stage of labor 25. Fetal Heart Rate Q15 Min: (2) document after a contraction during the second stage of labor MC 7277 (04/2012) 4N Labor and Delivery Standard Orders for Term Labor / Delivery (Physician must sign all orders-check and/or fill in appropriate blanks) Page 2 of 5 Activity 26. ambulate with fetal reassurance bedrest with bathroom privileges bedrest Labs: if no prenatal labs order HIV testing, Hepatitis, RPR, T&S Obtain rapid HIV if anticipating delivery soon and 3rd trimester HIV testing unknown: 27. Rapid HIV L&D x1 pregnancy, hiv status unknown 28. Nursing: Give Source Patient "Rapid HIV-1 Antibody Test Information Booklet" (print from e-docs) If results are NOT needed immediately: 29. HIV 1&2 AB & P24 AG BY CIA x1 / 30. Hepatitis B Surf Antigen X 1 31. RPR Qualitative blood X 1 32. Type & Screen (ABO/RH/ATBY SCN) X 1 33. Blood Band Misc Sample x1 (draw one purple top, send to blood bank to hold for workup) IV Fluids 34. LR: Lactated Ringers 125 ml/hr iv 35. Nursing: No IV or heparin flush/ lock 36. Heparin 100UNITS/ML FLUSH SOLN 3 ml flush q12h (flush each shift) 37. Heparin 100UNITS/ML FLUSH SOLN 3 ml flush prn (flush prn after each access) For Diabetic Patients 38. D5 1/2 NS: 125 ml/hr iv (via infusion pump) 39. NS: Sodium Chloride 0.9% 125 ml/hr iv 40. Blood Glucose Testing, OB Q2H 41. Blood Glucose Testing, OB Q1H if glucose is greater than 110 mg/dl or on insulin infusion 42. Regular Human Insulin INF: 1 units/hr iv now (notify Pharmacy when bag needed begin infusion for blood glucose greater than 110 mg/dl on 2 consecutive measurements) Analgesics & Antiemetics 43. Butorphanol: STADOL 1mg iv q6h prn (May repeat once in one hour if pain score remains greater than 4) 44. Nalbuphine Injection: NUBAIN 10 mg iv q8h prn (May repeat once within one hour if pain score remains greater than 4) 45. Ondansetron Injection: 4 mg iv q6h prn (for nausea/vomiting) MC 7277 (04/2012) 4N Labor and Delivery Standard Orders for Term Labor / Delivery (Physician must sign all orders-check and/or fill in appropriate blanks) Page 3 of 5 GBS Prophylaxis For Unknown GBS status order antibiotics if: EGA<37 wks, membranes ruptured>18hrs, temp>100.4, GBS UTI w/current pregnancy, hx of infant with GBS sepsis 46. Penicillin-G injection 5 million units IV now X 1, as loading dose for patient 5 mu IV X 1 now (loading dose) Penicillin-G injection: 2.5 mu IV q4h =+4hr (discontinue post –delivery) If penicillin allergic and low risk of anaphylaxis: 47. Cefazolin Inj: ANCEF 2000 mg iv x1 now (loading dose) Cefazolin Inj: ANCEF 1000 mg iv q8h =+8h (discontinue post delivery) If penicillin allergic and high or unknown risk of anaphylaxis GBS isolate testing available and sensitive to clindamycin and erythromycin: 48. Clindamycin Inj: CLEOCIN 900 mg iv q8h now (discontinue post delivery) OR … GBS isolate sensitivity unavailable/unknown OR GBS resistant to clindamycin OR patient allergic to all beta lactams and clindamycin 49. Vancomycin Injection: 1000 mg iv q12hx2 doses now (NHO if patient still laboring at last dose) Epidural Analgesia 50. NURSING: Epidural_1: Order the epidural tray, pump and tubing Epidural_2: Baseline heart rate, blood pressure and SpO2 prior to epidural placement Epidural_3: Nurse: remain with patient during epidural placement to assist with positioning and monitoring Epidural_4: Prepare 1 liter IV fluid (LR or NS) for administration in the case of an emergency LR BOLUS 1000 ml iv prn (in case of emergency during epidural analgesia) NS BOLUS 1000 ml iv prn (in case of emergency during epidural analgesia) epidural_5: insert a 3-way stopcock in IV tubing to permit administration of meds or fluids, if needed in an emergency epidural_6: monitor spo2 continuously during epidural placement; maintain sat monitor availability, but discontinue monitoring after placement epidural_7: vital signs q2 minutes immediately after epidural placement; when directed by anesthesia, q15 minutes x1hour; then, if stable, q30 minutes epidural_8: Remove BP cuff between measurements, maintain its availability epidural_9: bolus up to 500 ml of current infusing IV fluid prior to epidural placement MC 7277 (04/2012) 4N Labor and Delivery Standard Orders for Term Labor / Delivery Page 4 of 5 (Physician must sign all orders-check and/or fill in appropriate blanks) Choose level of fetal monitoring: epidural_10: Continuous fetal monitoring x1 hour after epidural placed; then, if stable, may monitor intermittently epidural_11: continuous fetal monitoring If patient chooses nitrous analgesia: 51. Nursing: Notify Anesthesia to initiate Nitrous oxide protocol (policy: Nitrous Oxide use in the Intrapartum/Immediate Postpartum Period Cervical Ripening 52. Misoprostol: CYTOTEC 25 mcg vaginal q4hx2 doses now 53. Misoprostol: CYTOTEC 25 mcg po q4hx2 doses now Induction/Augmentation-choose one dosing regimen: 54. oxytocin 15 units in ns 250 ml : pitocin 1 bag iv as dir now (start at 1 milliunit per minute and increase by 1 milliunit q 30 minutes) 55. oxytocin 15 units in ns 250 ml : pitocin 1 bag iv as dir now (start at 2 milliunit per minute and increase by 2 milliunit q 30 minutes) Third Stage of Labor: Choose Pitocin Order: 56. oxytocin 15 units in ns 250 ml : pitocin 2 bag iv as dir (rate 125ml/hr x 4 hours; start after delivery of *****baby (VUMC L&D Recommendation).) NURSING: process cord blood for T&S, send directly to blood bank. 57. oxytocin 15 units in ns 250 ml : pitocin 2 bag iv as dir (rate 125ml/hr x 4 hours; start after delivery of ***placenta.) NURSING: process cord blood for T&S, send directly to blood bank. Select one if oxytocin is NOT ordered upon transfer to floor: 58. Post-Procedure Nursing Order: No oxytocin is ordered for this patient: Patient is low risk and no oxytocin is indicated. 59. Post-Procedure Nursing Order: No oxytocin is ordered for this patient upon transfer to floor: Patient declines oxytocin. 60. Post-Procedure Nursing Order: No oxytocin is ordered for this patient upon transfer to floor: other___. For repair of lacertations: 61. Lidocaine 1% Injection: 20 ml infiltra x1 (for repair of lacerations by provider) Physician Signature: Date: ____________ Time: ______________ MC 7277 (04/2012) Page 5 of 5 MC 7277 (04/2012)