2015 department of medicine research day
advertisement
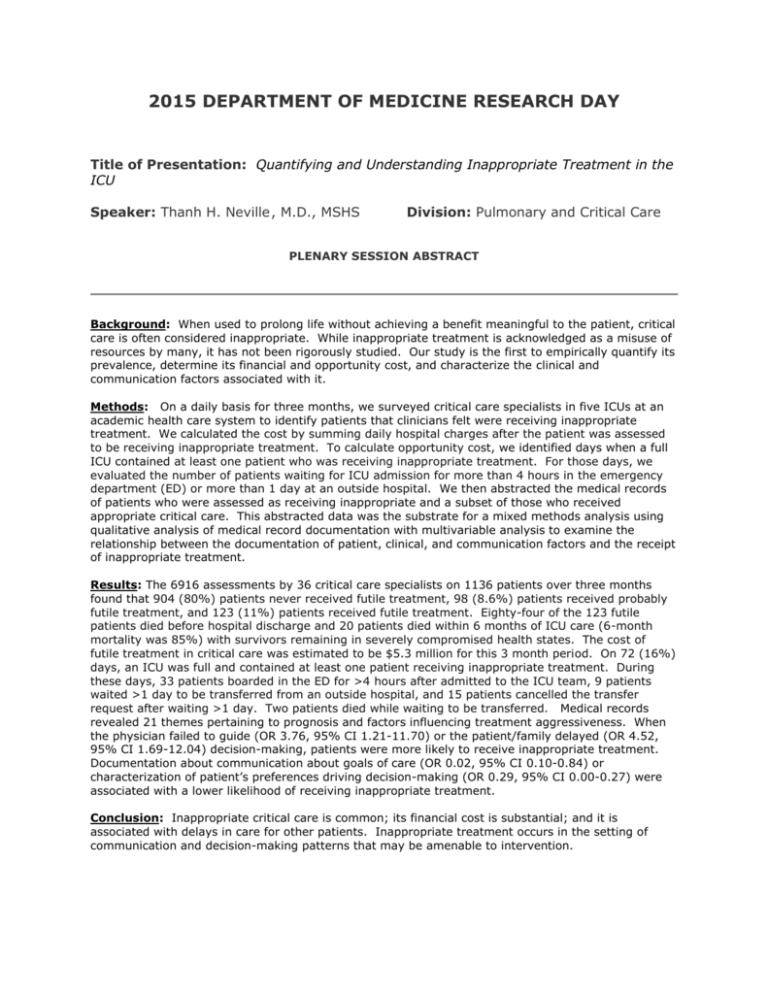
2015 DEPARTMENT OF MEDICINE RESEARCH DAY Title of Presentation: Quantifying and Understanding Inappropriate Treatment in the ICU Speaker: Thanh H. Neville , M.D., MSHS Division: Pulmonary and Critical Care PLENARY SESSION ABSTRACT Background: When used to prolong life without achieving a benefit meaningful to the patient, critical care is often considered inappropriate. While inappropriate treatment is acknowledged as a misuse of resources by many, it has not been rigorously studied. Our study is the first to empirically quantify its prevalence, determine its financial and opportunity cost, and characterize the clinical and communication factors associated with it. Methods: On a daily basis for three months, we surveyed critical care specialists in five ICUs at an academic health care system to identify patients that clinicians felt were receiving inappropriate treatment. We calculated the cost by summing daily hospital charges after the patient was assessed to be receiving inappropriate treatment. To calculate opportunity cost, we identified days when a full ICU contained at least one patient who was receiving inappropriate treatment. For those days, we evaluated the number of patients waiting for ICU admission for more than 4 hours in the emergency department (ED) or more than 1 day at an outside hospital. We then abstracted the medical records of patients who were assessed as receiving inappropriate and a subset of those who received appropriate critical care. This abstracted data was the substrate for a mixed methods analysis using qualitative analysis of medical record documentation with multivariable analysis to examine the relationship between the documentation of patient, clinical, and communication factors and the receipt of inappropriate treatment. Results: The 6916 assessments by 36 critical care specialists on 1136 patients over three months found that 904 (80%) patients never received futile treatment, 98 (8.6%) patients received probably futile treatment, and 123 (11%) patients received futile treatment. Eighty-four of the 123 futile patients died before hospital discharge and 20 patients died within 6 months of ICU care (6-month mortality was 85%) with survivors remaining in severely compromised health states. The cost of futile treatment in critical care was estimated to be $5.3 million for this 3 month period. On 72 (16%) days, an ICU was full and contained at least one patient receiving inappropriate treatment. During these days, 33 patients boarded in the ED for >4 hours after admitted to the ICU team, 9 patients waited >1 day to be transferred from an outside hospital, and 15 patients cancelled the transfer request after waiting >1 day. Two patients died while waiting to be transferred. Medical records revealed 21 themes pertaining to prognosis and factors influencing treatment aggressiveness. When the physician failed to guide (OR 3.76, 95% CI 1.21-11.70) or the patient/family delayed (OR 4.52, 95% CI 1.69-12.04) decision-making, patients were more likely to receive inappropriate treatment. Documentation about communication about goals of care (OR 0.02, 95% CI 0.10-0.84) or characterization of patient’s preferences driving decision-making (OR 0.29, 95% CI 0.00-0.27) were associated with a lower likelihood of receiving inappropriate treatment. Conclusion: Inappropriate critical care is common; its financial cost is substantial; and it is associated with delays in care for other patients. Inappropriate treatment occurs in the setting of communication and decision-making patterns that may be amenable to intervention.