Abstract - Macula and Retina Institute
advertisement

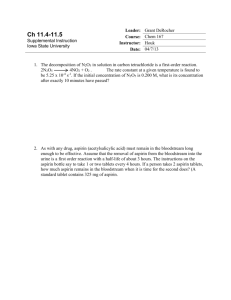
Abstract Purpose: To review current literature of the benefits that aspirin provides for patients’ cardiovascular health compared to the risk of AMD worsening. Methods: We performed a review and critically analyzed six cardiovascular and four ophthalmological trials. The cardiovascular trials consisted of over 95,000 individuals in primary and secondary prevention trials while the smaller ophthalmological trials had over 2,749 subjects. Results: The reviewed meta-analysis literature demonstrated a 32 % reduction in the risk of non-fatal stroke with regular aspirin users. The study also documented that aspirin users decreased the risk of vascular events by 15 %. Of the four ophthalmological studies, three suggested an exacerbation of AMD and one a possible benefit for AMD. Conclusion: Overall the number, size, and quality of the cardiovascular studies recommending aspirin use is much greater than the fewer, smaller and conflicting studies suggesting a possible adverse effect of aspirin use in relation to AMD. The benefits of aspirin usage include preserving the duration and quality of life by decreasing stroke and heart attack risk. These benefits seem to far outweigh the theoretical risks of possibly exacerbating wet AMD, which can be reasonably controlled with anti-VEGF therapy. Macular Degeneration and Aspirin use Many recent press releases regarding the potential adverse effects of aspirin in macular degeneration have caused some of my patients to discontinue their aspirin use.1-2 I advise my patients to continue with their doctor recommended aspirin use for many reasons. As with any treatment, it is important to weigh the risk / benefit ratio of aspirin use in this generally elderly and high-risk population. The benefits of aspirin have been well documented and highly recommended for the prevention and treatment of cardiovascular disease such as myocardial infarction, stroke, and death. The recent epidemiological studies suggesting that aspirin use may exacerbate macular degeneration are based on three studies, while the benefits of aspirin use for macular degeneration patients have been suggested in the larger Age-Related Eye Disease Study (AREDS) and the Physicians Health Study.10-13 Large cardiovascular studies: A review of numerous studies concerning regular aspirin users have been conducted in order to establish the benefits of aspirin in the prevention of cardiovascular diseases. The ATT Collaboration conducted a study on the effects of aspirin on primary and secondary prevention of vascular disease. The study performed a meta-analysis of six prevention trials (subjects had no history of occlusive disease), which consisted of 95,000 individuals of which 3554 had serious vascular events (MI, stroke, or vascular death) and secondary prevention trials (subjects with previous MI or stroke or transient cerebral ischemia) contained 17,000 participants with 3306 serious vascular events.3 The results showed that aspirin reduced vascular mortality (OR:0.91 (.82-1.00), p=0.06) which reduced total mortality by 10 % (OR: 0.90 (0.82-0.99), p=0.02)4. The findings also demonstrated that aspirin reduced major coronary events (OR: 0.80 (0.750.88) as well as ischemic stroke (OR:0.83 (0.73-0.95), p=0.005)4. Another meta-analysis study utilized five published trials (Physicians’ Health Study, British Doctors’ Trial, Thrombosis Prevention Trial, the Hypertension Optimal Treatment Study, and Primary Prevention Project) containing 55,580 randomized participants to illustrate a 32 % reduction in the risk of non-fatal stroke (OR:0.68, 95% CI, 0.59-.79) with regular aspirin users4. The study also documented that aspirin users decreased the risk of vascular events by 15 % (OR:0.85, 95 % CI, 0.79-0.93).5 Smaller AMD epidemiological studies: The three ophthalmological studies suggesting adverse effects of aspirin on ADM are the Blue Mountain Eye Study (BMES), the European Eye Study (EES), and the Beaver Dam Eye Study (BDES). There are 2 studies suggesting a benefit to AMD patients, AREDS and the Physicians Heath Study. The Blue Mountains Eye Study (BMES) database contained 2389 individuals, but only 257 were regular aspirin users (10.8%). A post hoc analysis was performed to determine if regular aspirin use interacted with age-related macular degeneration. This study was conducted over a 15-year period in which only 63 of the 2389 developed neovascular AMD. Their results suggested that regular aspirin users had a 2.5-fold increase in neovascular AMD compared with nonusers but no significant association was found between aspirin and geographic atrophy (dry AMD)6. The increase in neovascular AMD (wet AMD) went from 1.9 % in five years, 7 % in ten years, and 9.3 % in fifteen years in regular aspirin users (OR: 2.46, 95 % CI: 1.25-4.83, n=257).6 The European Eye Study pooled 4691 participants with early and late age related macular degeneration (ARMD) at 65 years of age and older, collected by random sampling. They found that early AMD was present in 36.4% of the participants and late AMD was present in 3.3% of participants. They also stated that with aspirin use, the odds ratios increased with the severity of the AMD (grade 1, 1.26 (95% confidence interval [CI], 1.08–1.46; P<0.001); grade 2, 1.42 (95% CI, 1.18–1.70), and wet late AMD, 2.22 (95% CI, 1.61–3.05).7 They reported that with early AMD only grades 1 and 2, but not grade 3 were associated with aspirin use. They found no association between aspirin use and pooled early or late AMD, nor with late AMD in those older than 85 years.7 The Beaver Dam Eye study is a longitudinal population-based study performed every five years for a 20-year period containing 4926 participants between the ages of 43 to 86 years old.8 Regular aspirin use 10 years prior to retinal examination was associated with late AMD (hazard ratio [HR], 1.63 [95% CI, 1.012.63]; P = .05) and with estimated incidence of 1.76% (95% CI, 1.17%-2.64%) in regular users and 1.03% (95% CI, 0.70%-1.51%) in nonusers. Regular aspirin use 10 years prior to retinal examination was significantly associated with neovascular AMD (HR, 2.20 [95% CI, 1.20-4.15]; P = .01) but not pure geographic atrophy (HR, 0.66 [95% CI, 0.25-1.95];P = .45). Aspirin use 5 years (HR, 0.86 [95% CI, 0.711.05]; P = .13) or 10 years (HR, 0.86 [95% CI, 0.65-1.13]; P = .28) prior to retinal examination was not associated with incident early AMD. They found that aspirin use 5 years prior to incidence was not associated with incident early or late AMD. However, they found that regular aspirin use 10 years prior was associated with a small but statistically significant increase in the risk of incident late and neovascular AMD.8 Limitations in the Epidemiological Studies The Blue Mountain Eye Study, a post hoc analysis, contained several limitations and thus the authors felt no valid conclusions could be made. There was no data obtained concerning the dose of aspirin each participant took and thus assumed that every “regular user” consumed 150 mg, when, in fact, most people take aspirin without a prescription and are subject to ingesting more than 150 mg daily (e.g. 300 mg). 6 In addition, the size of the cohort study was small and not randomized with a small number of AMD cases and only 56 % of the participants eligible for a follow-up were examined at the 15-year mark.9 Also, the study did not balance the number of subjects with possible risk factors such as age, occurrence of diabetes, heart disease, and strokes in accordance with the number of regular aspirin users. Furthermore, the number of regular aspirin users actually contained a higher percentage of participants with these conditions. Additionally, the authors note that the results do not reach statistical significance when adjusted for other risk factors (BMI, blood pressure, diabetes mellitus, blood total cholesterol level, and fish consumption).9 Additionally, the European Eye Study also a post hoc analysis contained a small sample size of aspirin users and presented results with an extremely wide confidence interval. In this study, there is also a possibility that people with AMD took aspirin after experiencing visual problems.7 There are no data regarding the amount of aspirin the participants used. Additionally, confounding by indication cannot be ruled out completely they did not eliminate the potential influence of cardiovascular deaths or angina in the analyses.7 There are also no data on other morbidities, such as arthritis, for which aspirin may be indicated. The Beaver Dam Eye Study contained numerous limitations that could have affected the conclusions. Regular aspirin users were defined as participants who took aspirin at least twice per week for >3 months, with a cumulative dose of only 24 pills which may not properly define a regular aspirin user.8 Regular aspirin users may have taken considerably larger amounts of the drug during the course of the study. Their definition fails to accurately distinguish between regular aspirin users and nonusers. Considering the inherent risk of bias in observational studies and the limitations in group definition and statistical analysis, the association between regular aspirin use and neovascular AMD may be a product of type I error.8 There are also multiple confounding factors that were not mentioned in the study. It is likely that subjects who regularly use aspirin have higher blood lipid levels than those who do not use aspirin, so blood lipid levels could be a confounding factor. Furthermore, high cholesterol is thought to contribute to the pathogenesis of AMD and thus should be reported to make the study more convincing.8 Studies contradicting AMD epidemiological results: In addition to the limitations contained in the BMES, BDES, and EES, there have been other studies suggesting a benefit of aspirin use in AMD. The Physicians’ Health Study reported that there was no increase in AMD during 7-10 years among the regular aspirin users. There were only 51 cases of age-related maculopathy (ARM) in the aspirin group and 66 in the placebo group (relative risk, 0.77; 95% confidence interval, 0.54-1.11). For ARM with vision loss, there were 25 cases in the aspirin group and 32 in the placebo group (relative risk, 0.78; 95% confidence interval, 0.46-1.32).10 The Age-Related Eye Disease Study (AREDS) reported that aspirin is actually beneficial in the protection of dry AMD patients11-13. AREDS, a larger study, shows the possible benefits of aspirin use for macular degeneration. AREDS studies 1, 3, and 19 have noted that the association between aspirin and AMD is not statistically significant.11-13 The case-controlled Age-Related Eye Disease Study (AREDS) reported that the use of anti-inflammatory medications, including aspirin, had a protective effect on dry AMD.13 Data from the BDES and the EES also suggested that aspirin has no effect on AMD risk at the 5-year mark of the study unlike the 10-year data.7,8 BDES and EES did not control for confounding variables such as other medical conditions requiring aspirin use such as arthritis. A recent review and meta-analysis demonstrated that there were no differences that exist between novel oral anticoagulants and other antithrombotic drugs for risk of substantial intraocular bleeding. In the Comparison of AMD Treatments Trials (CATT), Martin et al. attempted to seek the association between use of anticoagulant/antiplatelet and retinal hemorrhage. Among 1165 participants with active neovascular AMD, they found no significant association between the use of antiplatelet/anticoagulant with retinal hemorrhage at baseline.14 Conclusion: The BMES, BES, EES Blue Mountains Eye Study, the European Eye Study, and the Beaver Dam Eye Study received a great deal of press without the adequate context and consequences being explained to the public and to the medical community. The New York Times and CBS News have released newspaper articles discussing the results of the Blue Mountain Eye Study that resulted in patients stopping their recommended aspirin intake.1,2 However, Dr. Gregg Fonarow from UCLA stated that “individuals prescribed aspirin for high-risk primary or secondary cardiovascular prevention should not be concerned or discontinue this beneficial therapy.”1 Dr. George Diamond and Dr. Sanjay Kaul, cardiologists at Cedars-Sinai Hospital, also described how individuals should maintain the “status quo” and keep taking their recommended daily aspirin because the Blue Mountain Eye Study was observational and did not prove cause and effect.2 Dr. Rosenfeld added some context by noting how the correlation between aspirin and wet AMD is a marginal increase and thus may not represent a real-world significance.15 Patients who are taking aspirin for cardiovascular health should not fear the possible, theoretical and exaggerated risks of exacerbating their AMD. The inaccurate press releases have endangered the public by frightening many of the nation’s elderly into discontinuing their prescribed aspirin use. Overall the number, size, and quality of the studies recommending aspirin use is much greater than the few studies suggesting a possible adverse effect of aspirin use. This is reflected in the much smaller confidence intervals as shown in figure 1. The studies suggesting subjects to discontinue aspirin are post hoc analyses with small subject sizes and extremely wide confidence intervals. Substantial evidence exists to support the conclusion that the benefits of aspirin in decreasing the risk of stroke, heart attack, and death outweigh the potential minor increase in incidence of wet AMD caused by aspirin. Therefore, patients should continue taking their daily aspirin dose recommended by their primary physician. References 1. Jaslow R. Daily aspirin may increase risk for age-related blindness. CBSNews. http://www.cbsnews.com/news/daily-aspirin-may-increase-risk-for-agerelated-blindness/. Published 2013. Accessed May 15, 2015. 2. O'Connor A. Aspirin Use Tied to Rare Eye Disorder. New York Times. http://well.blogs.nytimes.com/2012/12/18/aspirin-use-tied-to-eyedisorder/?_r=1. Published 2015. Accessed May 10, 2015. 3. Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. British Medical Journal 2002;324(7329):71-86. 4. Baignet C, Blackwell L, Collins R. et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomized trials. Lancet 2009;373:1849-60. [http://www.ncbi.nlm.nih.gov/pubmed/19482214]. 5. Eidelman RS, Hebert PR, Weisman SM, Hennekens CH. An update on aspirin in the primary prevention of cardiovascular disease. Arch Intern Med 2009;163(17):2006-2010. [http://www.ncbi.nlm.nih.gov/pubmed/14504112] 6. Liew G, Mitchell P, Wong TY, Rochtchina E, Wang JJ. The association of aspirin use with age-related macular degeneration. JAMA internal medicine 2013; 173:258-64. [http://www.ncbi.nlm.nih.gov/pubmed/23337937]. 7. de Jong, P. T., Chakravarthy, U., Rahu, M., et al. Associations between aspirin use and aging macula disorder: the European Eye Study. Ophthalmology, 119(1), 112-118. 8. Klein BK, Howard KP, Gangnon RE, Dreyer JO, Lee KE, Klein R. Long-term Use of Aspirin and Age-Related Macular Degeneration. JAMA. 2012;308(23): 2469-2478. doi:10.1001/jama.2012.65406. 9. NPS MedicineWise. Aspirin and age-related macular degeneration- a link missing. NPS Direct. [http://www.nps.org.au/publications/health-professional/npsdirect/2013/march-2013/aspirin-amd]. Published March 25, 2013. Accessed August 4th, 2013. 10. Christen WG, Glynn RJ, Ajani UA, et al. Age-Related Maculopathy in a Randomized Trial of Low-Dose Aspirin Among US Physicians.Arch Ophthalmol. 2001;119(8):1143-1149. doi:10.1001/archopht.119.8.1143. 11. Chew EY, Clemons T, Sangiovanni JP, Danis R, Domalpally A, et al. (2012) The Age-Related Eye Disease Study 2 (AREDS2): study design and baseline characteristics (AREDS2 report number 1). Ophthalmology 119: 2282–2289. doi: 10.1016/j.ophtha.2012.05.027. 12. Age-Related Eye Disease Study Research Group. Risk factors associated with age-related macular degeneration: a case-control study in the age-related eye disease study: Age-Related Eye Disease Study Report Number 3. Ophthalmology 107.12 (2000): 2224-2232. 13. Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL 3rd (2005) Risk factors for the incidence of Advanced Age-Related Macular Degeneration in the Age- Related Eye Disease Study (AREDS) AREDS report no. 19. Ophthalmology 112: 533–539. doi: 10.1016/j.ophtha.2004.10.047. 14. Yang, G.S., Maguire, M.G., Daniel, E., et al. Association between Antiplatelet or Anticoagulant Drugs and Retinal Hemorrhage in the Comparison of AMD Treatment Trials (CATT). Abstract from clinical research/epidemiologic research section, ARVO 2015. 15. Rosenfeld PJ. Fact or Fiction: Does aspirin increase the risk of developing wet age-related macular degeneration (AMD)? The Newsletter of Macula Vision Research Foundation. 2013; 4-6.