Overview of Healthy Start Projects
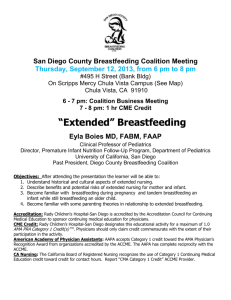
advertisement

Table of Contents Preface ................................................................................................................................................... 0 Overview of Healthy Start Projects .................................................................................................... 1 Introduction .................................................................................................................................. 1 Healthy Start Grantee Characteristics .......................................................................................... 1 Cultural Competence ................................................................................................................... 4 Healthy Start Service Components ..................................................................................................... 6 Outreach and Participant Recruitment ......................................................................................... 6 Case Management ........................................................................................................................ 8 Health Education ........................................................................................................................ 14 Interconception Care .................................................................................................................. 16 Perinatal Depression .................................................................................................................. 18 Support Services ................................................................................................................................. 20 Home Visiting ............................................................................................................................ 20 Breastfeeding Support ................................................................................................................ 22 Smoking Cessation..................................................................................................................... 24 Healthy Weight .......................................................................................................................... 25 Male Involvement ...................................................................................................................... 27 Family Involvement ................................................................................................................... 27 Domestic/Intimate Partner Violence and Child Abuse Screening ............................................. 28 Healthy Start Systems Components.................................................................................................. 33 Consortia .................................................................................................................................... 34 Local Health System Action Plan .............................................................................................. 41 Coordination and Collaboration ................................................................................................. 43 Sustainability.............................................................................................................................. 47 Perceived Outcomes ........................................................................................................................... 48 Intermediate and Long- Term Program Outcomes ................................................................... 48 Selected Community Outcomes ................................................................................................. 50 Appendix ............................................................................................................................................. 54 Appendix 1: Logic Model for the National Healthy Start Evaluation ....................................... 55 A Profile of Healthy Start ▌pg. ii Preface The U. S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB) has conducted several independent evaluations of the Federal Healthy Start Program since the program began in 1991. The Bureau awarded a multiyear contract in 2009 to Abt Associates Inc. to conduct the current evaluation. The first national evaluation of the Federal Healthy Start Program, conducted by Mathematica Policy Research in 1997 – 1999, examined the implementation of the 15 demonstration projects during fiscal years 1992 and 1996, and whether these projects achieved the goals of Healthy Start in reducing infant mortality and improving maternal and infant health. Findings suggested that Healthy Start was associated with improvements in measurements of prenatal care utilization, preterm birth rate, low and very-low birth weight rates, and the infant mortality rate. Specifically, several sites had significantly better outcomes than comparison sites. The second national evaluation was comprised of two phases. A key objective of the first phase of this evaluation (conducted from 2002 to 2004) was to provide information about the funded grantees and the implementation of the program components of the National Healthy Start program. Findings from this first phase were published in a similar report in 2006.1 The second phase consisted of eight case studies, including a survey of Healthy Start participants.2,3 The current evaluation, which builds on the previous evaluations, and uses a logic model (shown in Appendix 1.1) to illustrate how implementation of the nine program components may lead to a progression of the achievement of some short-term outcomes, which in turn, may translate into intermediate outcomes and then to longer-term outcomes. This evaluation is consistent with the needs of the MCHB to meet the requirements of the Government Performance and Results Act (GPRA). This report provides the descriptive findings from the Grantee Project Director Survey of 2011 and documents the accomplishments of the Federal Healthy Start Program. 1 Health Resources and Services Administration. (2006). A profile of Healthy Start: Finding from Phase 1 of the Evaluation 2006. Rockville, MD: Health Resources and Services Administration, U.S. Department of Health and Human Services. 2 Brand, A., Walker, D.K., Hargreaves, M., & Rosenbach, M. (September 2010). Intermediate Outcomes, Strategies, and Challenges of Eight Healthy Start Projects. Maternal Child Health Journal, 14(5), 654-65. 3 Rosenbach, M., Cook, B., O’Neil, S., Trebino, L., & Walker, D.K. (2010). Characters, access, utilization, satisfaction and outcomes of Healthy Start participants in eight sites. Maternal and Child Health Journal, 14(5), 666-679. A Profile of Healthy Start ▌pg. 0 Overview of Healthy Start Projects Introduction The National Healthy Start Program, funded through Health Resources and Services Administration’s (HRSA) Maternal and Child Health Bureau (MCHB), was developed in 1991 with the goal of reducing infant mortality disparities in high-risk populations through community-based interventions. The program originally began as a 5-year demonstration project within 15 communities that had infant mortality rates 1.5 to 2.5 times above the national average. By 2010, the National Healthy Start Program had expanded in size and mission to include 96 grantees implementing 104 projects in 38 states, the District of Columbia and Puerto Rico. The objective of the National Healthy Start Program is to implement evidence-based practices and innovative community-driven interventions to promote and improve the quality of health care for women and infants. To do this, Healthy Start works collaboratively with stakeholders and consumers in the community to leverage existing assets at both the service and system levels to ensure continuity of care from pregnancy through 2 years following delivery (prenatal to interconception). As specified by the HRSA 2001 Guidance, the core program goals, or intermediate outcomes of Healthy Start, include: Reduced racial and ethnic disparities in access to and utilization of health services, Improved local health care systems, Increased consumer or community voice in health care decisions. To meet those goals, HRSA identified nine core components that grantees are required to implement. These five service components are outreach and participant recruitment, health education, case management, maternal depression screening and interconception care services; the four systemsbuilding components are implementation of a consortium, development of local health system action plans, development of sustainability measures, and collaboration and coordination with Title V. The Grantee Project Director 2011 Survey was designed to collect information related to the implementation of the nine core program components and their features as well as additional, support services offered by all Healthy Start projects. Information on the accomplishments of each Healthy Start project for the subset of the service and system activities that were identified as most important in previous evaluations was collected as well; many survey questions were drawn from the 2004 survey of Healthy Start project directors. The 2011 Survey was administered as a web-based survey between July and September 2011. All projects completed the survey resulting in an 100 percent response rate. Healthy Start Grantee Characteristics Healthy Start begins with outreach to high risk pregnant and interconceptional women, high risk infants, and other women and male partners. Once enrolled, Healthy Start offers risk assessment and case management, care coordination, and referrals as a way to ensure that participants receive the services they need. Healthy Start allows each program flexibility to implement processes and services based on the the needs of the community and those being served by Healthy Start. Therefore, A Profile of Healthy Start ▌pg. 1 it is not surprising that Healthy Start grantees varied on a number of characteristics. For instance, community-based non-governmental agencies (43%) and government agencies including State and Local health departments (41%) were most often cited as the types of Healthy Start grantee organizations; less often reported agencies included non-profits (9%), universities (5%), tribal groups (2%), or Federally Qualified Health Centers (1%) (Figure 1). The scope of Healthy Start projects was predominantly local (77%); other projects reported having a multi-community scope (21%), far fewer reported regional or state-wide (2%) scope (Figure 2). Healthy Start projects served eligible participants in both urban and rural areas; however many more projects served participants in urban/central city (62%) and/or metropolitan (23%) areas compared with rural areas (27%). Few projects (5% or less) served participants in suburban areas and along the (US-Mexico) border (Figure 3). At the time of the survey, 104 Healthy Start projects were funded by HRSA; 17 percent of these projects were initially funded in the first phase when the program began in 1991 but most (61%) were funded during the second phase beginning in 1997 (Figure 4). A Profile of Healthy Start ▌pg. 2 A Profile of Healthy Start ▌pg. 3 Cultural Competence Because the populations served by Healthy Start projects are culturally diverse, the projects implement strategies to ensure that their staff is culturally competent. In 2010, 94 percent of all Healthy Start projects hired staff that represented the target population and 39 percent required contractors to do the same; 80 percent provided cultural competence training. Fifty three percent employed two of these three strategies; and 32 percent employed all three strategies. Other strategies used to promote cultural competence included hiring staff who were former participants, offering Spanish language instruction, and hiring staff who spoke the primary languages of the target population. Only three percent of all projects reported that they did not implement any of the abovementioned strategies for promoting cultural competence (Figure 5). Sixty-six percent of HS projects (69) indicated that their target population included individuals whose first language was not English. Of those 69 projects, 94 percent reported serving Spanish speaking participants. Additional languages spoken by populations served included French (19%), Arabic (10%), Hmong (7%) and Creole (7%) (data not shown). To facilitate communication with participants who did not speak English, 90 percent of HS projects assigned these participants to staff who spoke the same language; 43 percent allowed friends or family of the participant to translate; and 39 percent contracted with outside agencies for translation/interpretation services. Three percent reported that staff was unable to communicate with participants who were non-English speakers. Additionally, Healthy Start projects reported a variety of ways in which screening tools were adapted for each participant’s cultural background. For instance, approximately 80 percent (79.8%) of projects reported using staff who spoke the participant’s language to administer screening tools (79.8%), and 58 percent (57.7%) of the projects reported adapting tools to meet the cultural needs of their participants. Fewer projects reported using translators, or using an advising group to review the tools (data not shown). A Profile of Healthy Start ▌pg. 4 A Profile of Healthy Start ▌pg. 5 Healthy Start Service Components As described above, the Healthy Start Program consists of five core service components: outreach, case management, health education, perinatal depression and interconception care. All 104 Healthy Start projects were implementing all five core service components. Outreach and Participant Recruitment Outreach and client recruitment are the point of entry for Healthy Start project participants. A project’s ability to reach out to women and families in the community, and recruit their participation, is a key first step in impacting access to needed services. For the most part, Healthy Start projects employed their own project staff to perform outreach and recruitment; however, staff from other agencies under subcontract or organizations in collaboration with Healthy Start staff (41%) also conducted outreach and recruitment in addition to a combination of Healthy Start and contracted staff. Fewer projects (approximately 3%) reported using other staff, including Title V employees and other grant-funded employees (Figure 6). Outreach was targeted to the eligible cultural and ethnic groups within the communities using specific strategies that included utilizing staff reflective of the community being served (86%); connecting with community initiatives that reflect the participants’ cultural group (74%); translation of written materials (74%); and applying knowledge of customs and cultures during participant interactions (68%) (Figure 7). Major client outreach and recruitment strategies included both community-based strategies and mass media approaches. Community events (98%), brochures (94%) and networking with health care providers, schools, or other agencies (93%) were common community-based strategies. Fewer Healthy Start projects utilized mass media; 51 percent implemented newspaper or advertising campaigns as a way to reach participants. Many projects also used classes or presentations as a way to reach potential participants (83%), as well as neighborhood canvassing (82%). Other strategies included informal networking such as word of mouth through current or former participants, or advertising on websites of other local organizations (Figure 8). A Profile of Healthy Start ▌pg. 6 A Profile of Healthy Start ▌pg. 7 Case Management Case management is a required core service of the Healthy Start Program and an important mechanism for understanding the often complex needs of Healthy Start participants. It is essential for linking women with needed referrals to care. The majority of Healthy Start projects engage participants in their home (92%), which allows staff to engage their clients in surroundings that are comfortable to the participant, and also allow staff to better understand the varying facets of each participant’s life. Many projects also report (71%) providing case management at the project site, while others do so in clinics (51%), or in other community- based settings (41%). A few (25%) projects reported delivering case management in other settings such as schools, WIC offices, or other places convenient for the participant (Figure 9). Case management services were mainly provided by Healthy Start project staff (76%); staff from other agencies and organizations (34%) and a combination of Healthy Start and subcontracted staff (11%) also provided case management services (Figure 10). Case management staff was mostly social workers (67%) or nurses (63%); over half were staff indigenous to the community (59%). Less than one-third of case managers had backgrounds in health education (32%) behavioral/mental health (29%), public health (28%) or something else (Figure 11). Case management provides a prime opportunity for Healthy Start staff to assess the needs of the participant, and then to provide referrals as needed. As such, case management services occurred in a variety of settings, for prenatal/pregnant women, and women during the interconception period. The majority of projects reported providing case management services prenatally or during pregnancy through home visiting (93%), at the Healthy Start project site (79%), or over the phone (88%). Similar case management services were offered to women during the interconceptional period. The vast majority of Healthy Start projects offered some referrals through case management (Figure 12). The type of referrals varied, although most projects reported that case managers made referrals A Profile of Healthy Start ▌pg. 8 for many critical social services such as domestic violence/shelters (97%), WIC/food assistance (97%), substance abuse treatment and counseling (96%), housing/heating (96%), mental/behavioral health (96%), clinical services (92%) and transportation services (89%). Other reported referrals included childbirth, childcare, breastfeeding classes, GED and employment services, family planning services, and Medicaid enrollment assistance. In addition, most projects (89.4%) reported developing written service plans as a part of their case management activities (data not shown). Several barriers to accessing care through primary care providers were identified by respondents (Figure 13). The most predominantly reported barrier was lack of transportation to and from appointments (79%); lack of health insurance (78%) and participant perceptions or misperceptions of primary care (68%) of respondents. Less frequently, Healthy Start projects reported lack of available providers (41%) and language barriers between the participant and provider (35%). Other barriers reported included lack of child care, and competing priorities. Similarly, barriers to accessing referrals made through case management were reported (Figure 14). The most predominantly reported barrier was unstable housing (91%), followed by lack of transportation (85%); lack of child care (78%) and depression or other mental health conditions (76%). Other barriers again included competing priorities. A Profile of Healthy Start ▌pg. 9 A Profile of Healthy Start ▌pg. 10 A Profile of Healthy Start ▌pg. 11 A Profile of Healthy Start ▌pg. 12 A Profile of Healthy Start ▌pg. 13 Health Education All 104 Healthy Start projects provided health education to participants. Health education was most often conducted at a participant’s home (90%), the Healthy Start project site (85%), or other community-based setting (84%). Fewer projects reported conducting health education at clinics (59%) (Figure 15). Eighty four percent of Healthy Start projects used project staff to perform health education activities. Less than half reported using staff from another agency or organization (37%) or a mix of Healthy Start and subcontracted staff (23%) (Figure 16). A large proportion of health education staff were indigenous to the community (76%). Projects also utilized staff with health education (64%) or nursing backgrounds (57%) (Figure 17). Projects reported a wide array of educational offerings. Some key educational topics reported by 103 of the 104 projects included: immunization, breastfeeding, sudden unidentified infant deaths/sudden infant death syndrome (SUID/SIDS), child safety and injury prevention, perinatal depression, substance abuse, nutrition, and tobacco use cessation (data not shown). A Profile of Healthy Start ▌pg. 14 A Profile of Healthy Start ▌pg. 15 Interconception Care Beginning in 2001, the Division of Healthy Start and Perinatal Services (DHSPS) formally introduced interconception care as a core component of Healthy Start in recognition of the important role of interconception care in eliminating disparities and improving maternal and infant outcomes. Since 2005, all grantees have been required to incorporate an interconception care component into the services offered by their Healthy Start projects. All Healthy Start projects reported offering interconception care services to participants. The majority (94%) of Healthy Start projects provide interconception care (ICC) services in the participant’s home, while many participants receive these services at the project site (75%). More than half of the projects provided ICC services at clinical (56%) and other community-based settings (53%) (Figure 18). Interconception care services were provided predominantly by Healthy Start project staff (76%) (Figure 19). Staff backgrounds of those providing interconception care services included social work (65%) and nursing (61%) (Figure 20). Referrals are a key component of Healthy Start interconception care services. For example, more than 80percent of projects offered the following through the interconception care component of their projects: clinical or mental health services, food assistance, housing and heating assistance, substance abuse treatment and counseling services for women experiencing domestic violence, and transportation referrals (data not shown). A Profile of Healthy Start ▌pg. 16 A Profile of Healthy Start ▌pg. 17 Perinatal Depression Evidence has shown links to depression and adverse pregnancy outcomes, as well as risk of depression for women following the birth of their babies. Furthermore, low-income mothers of young children experience particularly high levels of depression, often in combination with other risk factors. Perinatal depression screening became a required component in the third funding cycle of Healthy Start, beginning in 2001. All projects currently provide perinatal depression screening. The majority (91%) of Healthy Start projects provide perinatal depression screening services in the participant’s home, while some offer services at the project site (67%). Close to half perform perinatal depression screening services at clinics (47%) and in other community based settings (47%) (Figure 21). Perinatal depression screening services are provided mainly by Healthy Start project staff (73%) (Figure 22), and staff with social work (64%) and nursing (55%) backgrounds or staff indigenous to the community (56%). Less than 50 percent (44%) of all staff providing perinatal depression screening services have a mental health background (Figure 23). Although information on the screening tools most often used to screen for perinatal depression was not collected through the 2011 Survey, many of the Healthy Start projects that participated in the Interconception Care Learning Collaborative (ICC LC) from 2009-2011 indicated that they used the Edinburgh or the PHQ-9 scale to assess depression (data not available). A Profile of Healthy Start ▌pg. 18 A Profile of Healthy Start ▌pg. 19 Support Services A total of 68 Healthy Start projects (35%) reported offering all of the following support services: home visiting, breastfeeding support and education, smoking and other tobacco use cessation, healthy weight services, male and family involvement, domestic/intimate partner violence screening and child abuse screening or services. Home Visiting Evidence-based home visiting programs have been shown to reduce adverse birth outcomes such as low birth weight, decrease the incidence of child abuse and neglect, and positively impact child development, including literary skills and test scores. The Patient Protection and Affordable Care Act of 2010 authorized the creation of a Maternal, Infant and Early Childhood Home Visiting Program, which is providing funding to states to establish home visiting program models for at-risk pregnant women and children from birth to age 5. The new funding has heightened the attention to and need for home visiting program models that target families with pregnant women and young children and rigorous evaluation to assess the effectiveness of these home visiting models. Home visiting is a core mechanism through which Healthy Start programs deliver preventive services that address disparities in perinatal health and infant mortality. Approximately half (51%) of all Healthy Start projects conduct home visits based on a model. Many projects use State or local models or a combination of models. A few projects use existing evidence-based models or promising practices such as Parents as Teachers (23%), Healthy Families America (19%), and Nurse Family Partnerships (19%). Several projects also reported the use of curricula such as Florida State University’s Partners for a Healthy Baby (Figure 24). Of the 82 Healthy Start projects that offered home visiting through required components, the majority of projects conducted home visiting for case management (93%) and interconception care services (82%). Many also offer home visiting through health education (60%) and some offer home visiting via outreach services (39%) (Figure 25). The 103 Healthy Start projects that reported conducting home visits all provided home visiting to their participants and 42 percent provided these services to partners of participants and 16 percent to non-partner family members. The majority of Healthy Start projects provide home visiting services to high risk women in either the interconception period (94%), or prenatally and during pregnancy (93%). Furthermore, the majority of projects also offer services to high risk infants and toddlers through 23 months (92%). Approximately 90 percent of projects also report serving women and infants at moderate risk through home visits (Figure 26). A Profile of Healthy Start ▌pg. 20 A Profile of Healthy Start ▌pg. 21 Breastfeeding Support Evidence shows that breastfeeding plays a central role in the development and maturation of immune systemof infants. Breast-fed infants were less likely to develop gastrointestinal illness compared with infants in the control group. The health and bonding benefits to baby and mother, as well as potential cost savings make breastfeeding an important option for new mothers. Yet, the rates of breastfeeding are particularly low among African American women, making breastfeeding support an important part of the support services offered by Healthy Start projects. All Healthy Start projects reported addressing breastfeeding either during pregnancy or during the prenatal period; most (92%) also discuss breastfeeding during the interconception period. Additionally, 85% also offer individual breastfeeding support to postpartum participants (Figure 27). Of the projects that offer individual support, most have peer counselors available for individual breastfeeding support (67%), and some have certified lactation consultants (49%) or doulas (18%) onsite for consultation (Figure 28). Breastfeeding is encouraged through offering private space for participants (65%) as well as Healthy Start staff (61%) (Figure 29). Additional breastfeeding support is offered through loaning or donating breastfeeding equipment to participants at some Healthy Start projects, with 44 percent offering breast pumps, 23 percent offering breast shells or shields, and 10 percent offering nursing supplementers to participants (Figure 30). A Profile of Healthy Start ▌pg. 22 A Profile of Healthy Start ▌pg. 23 Figure 30: Breastfeeding Equipment Available to Loan or donate to Healthy Start Participants, 2010 Breast Pumps 44% Breast Shells/Shields Nursing Supplementers 23% 10% Smoking Cessation The association between maternal smoking and low birthweight is well established. The importance of smoking and tobacco use cessation among women of childbearing age is reflected in the fact that Healthy Start projects address this topic during many interactions with participants including home visits (98%), face to face meetings (82%), and group health education classes (85%) (data not shown) In fact, the majority of (99%) of the Healthy Start projects offer participants a number of opportunities for smoking/tobacco use cessation. The opportunities are primarily through access to community, state-run or other quit lines (86%), referrals (84%) and one-on-one counseling (63%). A few projects offer group counseling (30%) and even fewer offer medication options (18%) (Figure 31). A Profile of Healthy Start ▌pg. 24 Healthy Weight Obesity has reached epidemic proportions in the United States. Among women the correlates of obesity are increasing age, low education and/or low economic status. Additionally, there is an increasing prevalence of overweight and obesity among women of childbearning age, and currently 1out of 5 women are obese at the beginning of their pregnancy and obesity has been linked to a number of adverse reproductive outcomes. Given the risk factors for and prevalence of obesity, as well as the known links between obesity and adverse outcomes in women and children, addressing Healthy Weight is a priority for Healthy Start projects.The majority (97%) of Healthy Start projects discussed healthy weight with participants and most (80%) encouraged or promoted weight-related activities with staff . Among the 101 Healthy Start projects addressing healthy weight with participants, the majority addressed nutrition (100%), physical activity (97%) and weight management (94%) during home visits (89%), group education classes (73%), face to face meetings (68%), other routine care-related contacts (56%), and outreach activities (49%). Additionally, these projects report offering literature on weight and nutrition (93%), nutrition-related education (91%), and education about weight and pregnancy (87%) (data not shown). Of the 83 projects that addressed healthy weight with staff, 99 percent discussed physical activity, as well as nutrition (94%), and weight management (93%) (Figures 32 & 33 & 34). A Profile of Healthy Start ▌pg. 25 A Profile of Healthy Start ▌pg. 26 Male Involvement Healthy Start enables men to play a positive role in the lives of Healthy Start women participants and their children. The majority of Healthy Start projects (69%) offer services to men either as part of a male-only program or through services offered to female participants (data not shown). These services primarily include health education (96%), but case management (65%), court advocacy (43%), mental health services (42%) and clinical services (25%) are also offered to men by some Healthy Start projects (Figure 35). Family Involvement Healthy Start projects encourage family involvement in services and activities, and all projects indicated that family involvement is an important part of the activities offered to participants. Specifically, 80 percent of Healthy Start projects reported that at least some (30 % or more) participants had family involved in their Healthy Start activities. For example, 88 percent invite family members to attend any health education opportunities, 86 percent offer the opportunity to attend consortium meetings, and 84 percent encourage family members to attend outreach activities. Many projects encourage family involvement through health education (80%) or outreach (75%) designed specifically for family involvement. Fifty three percent of projects reported that family members are invited to be present in the development of a written service plan for participants. A Profile of Healthy Start ▌pg. 27 Projects also reported encouraging family participation in other ways, including designing brochures and PSAs, participating in focus groups, or serving on consortia (Figure 36). Domestic/Intimate Partner Violence and Child Abuse Screening Domestic violence/intimate partner violence (IPV) during pregnancy not only has serious consquences for the health of the mother, but can also negatively impact pregnancy and the subsequent health of the infant, with outcomes such as premature labor and low birthweight associated with IPV during pregnancy. Healthy Start projects overwhelmingly offer training about domestic IPV and child abuse to their staff, and most report offering referrals to their participants. Eighty four percent of Healthy Start A Profile of Healthy Start ▌pg. 28 projects offered staff training on child abuse, and 95 percent offered training on Domestic/Intimate Partner Violence(DV/IPV); similarly 47 percent of projects provided referrals for child abuse, and 95 percent provided referrals for DV/IPV. Training on a variety of topics related to child abuse and DV/IPV were offered. Most projects offered staff training on what constitutes child abuse (98%), reporting requirements for suspected child abuse or neglect (97%), and how to make referrals to community or legal services (93%), among other topics. Other training topics included in-house protocols on child abuse reporting (Figure 37). Training on domestic/intimate partner violence included: what constitutes domestic/intimate partner violence (98%), resources in the community or through the legal system (94%), and how to make referrals (91%) (Figure 38). Referrals most often provided for suspected child abuse included referrals to protective services (96%), referrals to shelters or safe havens (96%), and referrals to mental health services (96%) (Figure 39). Of those Healthy Start projects making referrals for DV/IPV (99), all referred to shelters and safe havens for participants experiencing domestic/intimate partner violence. Other referrals included referrals to mental health services (97%), and medical referrals for domestic violence related injuries (84%), among others (Figure 40). A Profile of Healthy Start ▌pg. 29 A Profile of Healthy Start ▌pg. 30 A Profile of Healthy Start ▌pg. 31 A Profile of Healthy Start ▌pg. 32 Healthy Start Systems Components Community wellness and transformation requires significant collaborative efforts among various public and private partners for addressing environmental changes in combination/unison with individually focused behavior changes. Healthy Start systems components underscore the importance of local and State collaboration, stakeholder engagement, and sustainability planning for effecting systems-level change. Consortium and collaboration with Title V were the two original systems components required by Healthy Start; local health systems action plan (LHSAP) and sustainability planning were added during the third funding cycle (2001-2005) on the recommendation of Secretary’s Advisory Committee on Infant Mortality. These four required systems components – consortium, local health systems action plan, collaboration with Title V, and sustainability plan – were being implemented to varying degree by all Healthy Start projects (from 99% to 66%). Overall, however, all Healthy Start projects were more likely to implement service components than systems components (Figure 41). A Profile of Healthy Start ▌pg. 33 Consortia All projects have at least one consortium through which community stakeholders are engaged; the majority (77%) had one, with 11 percent reporting two consortia. Fewer Healthy Start projects reported 3 (6%), 4 (2%), or 5 or more (4%) consortia (Figure 42). Most Healthy Start projects reported that the purpose of a consortium was to share information with the community and raise awareness of maternal and child health issues (95%), bring together potential partners and enhance collaboration (91%), and to fulfill the requirements of the grant guidance (89%) (Figure 43). Systems activities conducted through the consortium included developing priorities to direct Healthy Start activities (88%), coordinating existing services and resources, such as building referral networks (87%), and enhancing community participation in identifying community needs, setting priorities, and implementing changes (82%) (Figure 44). Several accomplishments of the consortia were reported. The most often cited accomplishment was an increased awareness of infant mortality in the community (87%). Other accomplishments included an enhanced ability of Healthy Start projects to address disparities in access to and utilization of health services (65%), creating sustainable partnerships among member agencies (61%), and increasing Healthy Start participant involvement in the project's decision-making activities (57%). Approximately half of the projects reported increased integration of service systems (52%) and increased service capacity in the community (47%), as well as increasing the amount of, or access to, data available to partner organizations on the health status of the target population (46%). Fewer projects reported influencing policy affecting access to care for the Healthy Start target population (30%), using funds in an innovative manner (29%), or obtaining new grants or funding (19%) as accomplishments of the consortium (Figure 45). Additional accomplishments reported included increased provider or member knowledge, needs assessment development, and joint funding applications. Only 2 percent reported no accomplishments associated with the consortium in 2010. Fifty-six percent of Healthy Start projects reported irregular attendance at meetings as a barrier to consortia accomplishments; other reported barriers included lack of resources to support the consortium (39%), insufficient staff time to assist with the efforts of the consortium (38%), and lack of participant engagement (36%). Among those projects reporting other barriers, budget cuts were among the most often-offered response. Forty two percent of projects reported that their consortium did not have any challenges in 2012 (Figure 46). Consumer involvement is key to the success of a consortium, yet lack of Healthy Start participant involvement in consortia remains a barrier to consortia accomplishments, as reported by Healthy Start projects. In an effort to encourage Healthy Start participant involvement in consortia, several strategies were employed including providing supports such as child care or transportation to participants (77%), designing the consortia meetings to be both welcoming and interesting to participants (75%), choosing convenient meeting and event times (74%) as well as convenient locations (73%) and actively recruiting Healthy Start participants to be a part of the consortia (72%). Other strategies reported included incentivizing participants, and involving case managers in recruiting participants for consortia participation (Figure 47). A variety of methods were also used to promote leadership among Healthy Start participants involved in consortia. Most commonly reported methods for promoting leadership included inviting A Profile of Healthy Start ▌pg. 34 participants to serve on subcommittees (65%), sending participants to conferences (65%), conducting leadership training sessions (45%) and inviting participants to facilitate meetings (42%) (Figure 48). A Profile of Healthy Start ▌pg. 35 A Profile of Healthy Start ▌pg. 36 A Profile of Healthy Start ▌pg. 37 A Profile of Healthy Start ▌pg. 38 A Profile of Healthy Start ▌pg. 39 A Profile of Healthy Start ▌pg. 40 Local Health System Action Plan The development of a Local Health System Action Plan (LHSAP) became a required component during the third funding cycle, beginning in 2001. A total of 95 Healthy Start projects (91%) currently have a Local Health System Action Plan, with 68 percent reporting that their LHSAP is specific to Healthy Start (Figure 49). The majority of those projects with a LHSAP report that Healthy Start staff (89%), key community partners (79%), Healthy Start consortium members or a consortium subcommittee (77%), and the local health department (73%) are involved in the development of the LHSAP. Fewer projects reported involving Healthy Start participants (56%), the state Title V agency (44%) and local Title V grantees (42%), as well as local government agencies (36%) (Figure 50). Strategies used to facilitate consumer involvement in consortia with and without LHSAP were examined. Among those projects with a LHSAP, 40 percent reported communication improvements between community agencies and institutions as a result of Healthy Start efforts, 39 percent reported that Healthy Start had created solutions to address health care access problems, and 36 percent reported that Healthy Start was able to document a positive effect on local maternal and child health issues. Twenty five percent of the projects with a LHSAP reported that Healthy Start contributed to the community’s capacity for assessing maternal and child health issues (data not shown). In terms of developing a basis for change, of those projects with a LHSAP, 53 percent reported that Healthy Start is connected to the community’s power structure, and 16 percent reported that Healthy Start is an integral part of the delivery system in the community (data not shown). A Profile of Healthy Start ▌pg. 41 A Profile of Healthy Start ▌pg. 42 Coordination and Collaboration Healthy Start projects have established relationships with many entities in their communities and are engaged in a wide range of collaborative activities. Almost all Healthy Start projects reported collaboration with health-related organizations such as local health departments (94%), mental health agencies (94%), WIC programs (92%), hospitals (91%) substance abuse programs (90%), and Federally Qualified Health Centers (88%). In addition, most projects also reported collaborating with State Title V (87%), private physicians (86%), and Medicaid (84%) (Figure 51). Projects reported collaborating with several community-based organizations such as faith-based groups (98%), civic groups (92%), professional associations (82%), advocacy groups (81%), diseasebased organizations (80%), and ethnic organizations (76%) (Figure 52). Healthy Start projects collaborated with service-related organizations including schools (88%), child protective services (87%), Head Start/Early Head start (83%), welfare agencies (79%), and courts (64%) (Figure 52). Of projects that coordinate with State Title V, the most common reported benefit was access to data and other information provided by State Title V for needs assessment (74%). The majority of projects also reported that State Title V agencies help with efforts to advocate for Healthy Start target populations (66%) and provides resource materials for health education (63%). Approximately half of those projects that responded to the survey questions about State Title V reported State Title V’s assistance with increasing Healthy Start’s visibility in policy arenas (51%) as well as providing training for staff (51%) (Figure 53). Only five percent of Healthy Start projects reported no perceived benefits to this collaboration. Healthy Start projects also reported on their involvement in community-wide collaborative efforts related to a variety of important topics. Eighty three percent collaborated with the community on breastfeeding initiatives and 61 percent reported collaboration around the topics of smoking and other tobacco use cessation and healthy weight. Other areas of collaboration included infant mortality and prematurity, family planning, and access to care (Figure 54). A Profile of Healthy Start ▌pg. 43 A Profile of Healthy Start ▌pg. 44 A Profile of Healthy Start ▌pg. 45 A Profile of Healthy Start ▌pg. 46 Sustainability The requirement that all projects develop a plan to sustain Healthy Start services at the end of the grant began in the third funding cycle; sixty nine Healthy Start projects (66%) had a sustainability plan (Figure 55) in 2010. Among the 69 Healthy Start projects with a sustainability plan , sustainability strategies included seeking state or local funding (84%), collaborating with other organizations (83%) and seeking other federal funding (83%). More than half of the projects reported seeking additional Healthy Start funding (84%) and collaborating with State or local Title V (72%) as strategies used for sustainability. Fewer projects reported packaging services for Medicaid or health plan reimbursement (54%). A Profile of Healthy Start ▌pg. 47 Perceived Outcomes Intermediate and Long- Term Program Outcomes Healthy Start projects reported on several intermediate and long- term outcomes in a number of areas including increased awareness, improved systems of care, participant involvement, and participant service outcomes. With respect to outcomes around increasing awareness, many projects reported increasing awareness of the importance of interconception care (77%) and increasing awareness of disparities in birth outcomes as a priority in the community (73%). Furthermore, 71 percent of Healthy Start projects increased positive health behaviors among participants, 68 percent increased access to services available for participants, and 67 percent increased the number of participants with a medical home (Figure 56). Less than half of all projects reported achievement of outcomes related to improving systems of care; 49 percent increased screening for perinatal depression among providers in the community, 45 percent increased integration of prenatal, primary care and mental health services, and 41 percent increased the cultural competence of providers in the community. In terms of participant involvement, fewer projects reported increased participant involvement in Healthy Start decision making (48%), and participant involvement in other community activities addressing systems change (38%), and only 21 percent of Healthy Start projects increased participant involvement in decision making among partner agencies (Figure 56). Healthy Start projects further reported findings in support of intermediate outcomes. The majority of projects reported that evidence of project outcomes could be found in the MCHB performance measures (63%), local evaluation findings (60%), and in the Healthy Start Impact Reports (58%). Other evidence included new and continuing applications (49%), case study findings (13%), among others (data not shown). Finally, 88 percent of all projects reported achieving some long- term outcomes. Improved birth outcomes was the most often reported long -term outcome with 68 percent of projects reporting this achievement in 2010. Fewer projects reported improved maternal or child health, birth spacing, or sustained community capacity to reduce disparities in health status in the community (data not shown). A Profile of Healthy Start ▌pg. 48 A Profile of Healthy Start ▌pg. 49 Selected Community Outcomes Healthy Start projects engage with the community through a myriad of mechanisms including community outreach and recruitment, hiring staff indigenous to the community, encouraging community members to participate in consortia, and partnering with other community organizations to foster sustainability and to ensure that participants have access to needed care. Healthy Start projects were asked to report on a select set of community outcomes such as reduction in MCH disparities. Projects most often cited case management (87%) as a service activity that contributed to a reduction of disparities in maternal and infant health outcomes. Other services cited for playing a role in these efforts included interconception care (70%), perinatal depression screening (67%), enabling services (63%) and outreach and client recruitment (62%) (Figure 57). Collaboration with consumers (58%) was reported by many projects as a system activity that contributed to reducing disparities in maternal and infant health outcomes. Collaboration with community–based organizations (CBOs) (51%), provider education (47%), and collaboration with public (47%) and private (44%) agencies, consortium (43%), LHSAP (41%), as well as collaboration with State (30%) and local (33%) Title V were less often reported as contributing to reducing disparities (Figure 58). Additional outcomes were reported as a result of Healthy Start’s community relationships. For instance, 43 percent of the Healthy Start projects reported that changes or solutions have been implemented in the community as a result of Healthy Start recommendations. Forty one percent of projects reported improved communication between community agencies and institutions as a result of Healthy Start (Figure 59). Fifty four percent of projects reported that MCH agencies and providers take ownership of Healthy Start goals; 41 percent reported an institutional and fiscal base of support sustains Healthy Start. With regard to identifying issues, 38 percent of Healthy Start projects reported identification of strategies for addressing disparities, and 38 percent identified access problems in the health care system. Fifty one percent of projects also reported that Healthy Start was connected to the community’s power structure and that Healthy Start processes maintain a good balance between medical, public health, and community viewpoints (48%), as well as the fact that residents of the community are aware of Healthy Start (48%) (Figure 60). A Profile of Healthy Start ▌pg. 50 A Profile of Healthy Start ▌pg. 51 A Profile of Healthy Start ▌pg. 52 A Profile of Healthy Start ▌pg. 53 Appendix A Profile of Healthy Start ▌pg. 54 Appendix 1: Logic Model for the National Healthy Start Evaluation A Profile of Healthy Start ▌pg. 55