Prostate surgery and erectile dysfunction
advertisement
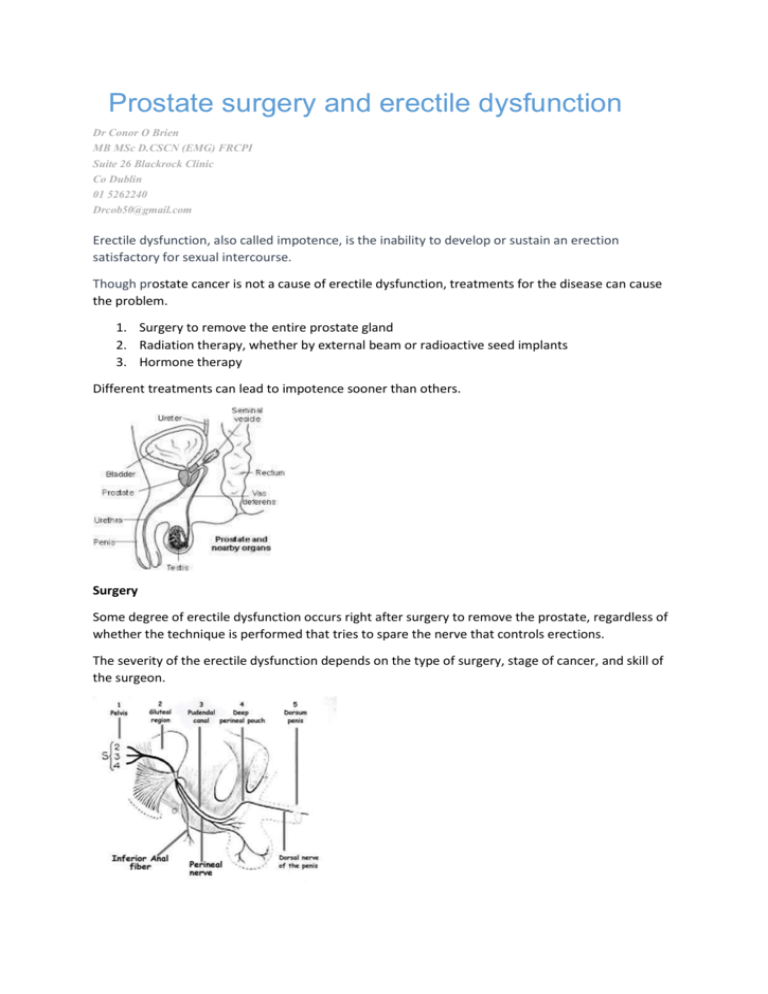
Prostate surgery and erectile dysfunction Dr Conor O Brien MB MSc D.CSCN (EMG) FRCPI Suite 26 Blackrock Clinic Co Dublin 01 5262240 Drcob50@gmail.com Erectile dysfunction, also called impotence, is the inability to develop or sustain an erection satisfactory for sexual intercourse. Though prostate cancer is not a cause of erectile dysfunction, treatments for the disease can cause the problem. 1. Surgery to remove the entire prostate gland 2. Radiation therapy, whether by external beam or radioactive seed implants 3. Hormone therapy Different treatments can lead to impotence sooner than others. Surgery Some degree of erectile dysfunction occurs right after surgery to remove the prostate, regardless of whether the technique is performed that tries to spare the nerve that controls erections. The severity of the erectile dysfunction depends on the type of surgery, stage of cancer, and skill of the surgeon. If the nerve-sparing technique is used, recovery from erectile dysfunction may occur within the first year following the procedure. Recovery of erectile function after a non-nerve-sparing surgery is unlikely, but possible. One study shows erectile dysfunction rates of 66% for nerve-sparing prostatectomy versus 75% for non-nerve sparing surgery at one year after the surgery. The use of vacuum devices or erectile dysfunction drugs after the body has healed from surgery may improve the quality of erections and speed the return of normal sexual function . If an erection can be achieved after surgery, one does not lose the ability to have an orgasm. However, they may be "dry" orgasms in which little (if any) ejaculate is produced. This results in infertility for most men, although most men are older when they are diagnosed for prostate cancer and may not be concerned. If desired, you could talk to your doctor about "banking" sperm before the procedure. Radiation therapy. The onset of erectile dysfunction following radiation therapy is gradual and usually begins about six months following the treatment. Erectile dysfunction is the most common long-term complication of radiation therapy. However, its occurrence decreases when more sophisticated treatments are used, such as radioactive seed implants (brachytherapy), intensity-modulated radiotherapy (IMRT), or 3-D conformal radiotherapy. Hormone therapy. When hormone therapy is used, erectile dysfunction and decreased sexual desire may result approximately two to four weeks after the start of therapy. This is due to the testosterone-reducing action of the drugs. Treatment Current treatment options for erectile dysfunction for men who have received treatment for prostate cancer include: Oral medications, such as Cialis, Levitra, Staxyn, Stendra, or Viagra Injections of medicine into the penis before intercourse (called intracavernous injection therapy) Use of a vacuum constriction device to draw blood into the penis to cause an erection Drugs taken as a suppository placed in the penis prior to intercourse Penile implants Following surgery, as many as 60% to 70% of men who have had nerves spared on both sides of the prostate will regain erections. Results are less favorable for men who have had a single nerve spared or no nerves spared. Following radiation therapy, overall, 50% to 60% of men regain erections with medication. However, current data are rather limited, especially for patients treated with radioactive seed implants. Hormone therapy. Men treated with hormone therapy do not respond well to any erectile dysfunction treatments, but data are limited. If oral erectile dysfunction drugs fail, injections into the penis can be an effective form of treatment for men who have undergone surgery or who have received radiation therapy (whether by external beam or seed implants) for prostate cancer. Overall, 60% to 80% of men will regain erections with the use of injection treatments. Side effects include occasional pain due to one of the drugs used for injection therapy, and the development of scar tissue. If Viagra and injections fail (or if you are unwilling or unable to use either therapy), other treatments may be appropriate. Vacuum constriction device. A cylinder is placed over the penis. The air is pumped out of the cylinder, which draws blood into the penis and causes an erection. The erection is maintained by slipping a band off the base of the cylinder and onto the base of the penis. The band can stay in place for up to 30 minutes. Although these devices can be effective, they generally have been less desirable for patients who have been treated with surgery. Many patients dislike having to use the band at the base of the penis and find it uncomfortable. Penile suppositories. For this treatment, the patient places a suppository into the urinary tube (urethra) using a plastic applicator. The suppository contains the drug alprostadil, which travels to the erection chambers. Alprostadil relaxes the muscle in the erection chamber, allowing blood to flow into the penis. This treatment works in only about 30% of men. Penile implants. This option may be considered if the patient has had erectile dysfunction for about one year following cancer treatment and nonsurgical therapy has either failed or is unacceptable. An implant, or prosthesis, is an effective form of therapy in many men, but it does require an operation to place the implant into the penis. Surgery can cause problems, such as mechanical failure or infection, which may require removal of the prosthesis and re-operation. However, most men and their partners are very satisfied with these devices. The success rate is as high as 95%. Direct Treatment of pelvic floor pain and erectile dysfunction by targeting the pudendal nerve Pelvic floor pain and dysfunction Pelvic floor pain can come in a variety of forms, from burning and itching to a constant dull ache. Frequently patients will describe an uncomfortable feeling, which they associate with passing urine or a bowel motion. The pain can also be accompanied by episodes of minor incontinence Most pelvic floor pain is generated through the pudendal nerve. This nerve is formed by 3 sacral nerve roots and then enters the pelvis before travelling through a tunnel before it splits into 3 branches. These 3 braches supply pain and sensation, as well as the sphincter muscles essential for urination and defecation The nerve can be injured anywhere along its course. Local back or pelvic trauma can damage the nerve. Up to 30% of all women can experience some transitory symptoms following vaginal birth. Of these women a further 1/3 can develop chronic problems. Pelvic floor pain can be treated in a number of ways 1. Oral Medication 2. Neuromodulation 3. Injection therapy. Oral Medication The oral medication used to treat pelvic floor pain are similar to those used to treat “neuropathic pain syndrome”, and include, Simple analgesics, non-steroidal anti-inflammatory, Pregablin and sildenafil like medication. The first 2 options work by interrupting the inflammatory cascade that is associated with injury and pain The pregablin medication alters the nerves response to the painful stimuli, by blocking the calcium channels on the nerves, thus altering the nerves response, and reducing the symptoms of pain. The 4th oral option is medication which selectively increases the pelvic blood flow to the injured nerve All oral medication have side effects, these will by described by your medical practitioner. Neuromodulation Electrical stimulation to reduce pain has been used for over 60 years. Neuromodulation has been recently shown to reduce the symptoms of pelvic floor pain. The treatment involves a nerve in your foot [ the posterior tibial nerve] being stimulated by an electrical impulse. This sends a message up the nerve to the spine where the message “bounces off” the spinal cord and is sent down the affected nerve. In this case the pudendal nerve. The treatment involves 12 sessions lasting 10-15 minutes. This treatment has proven to be successful in over 70% of cases of pelvic floor pain and dysfunction involving the urinary system Injection therapy In cases of severe pain the pudendal nerve can be injected in an effort to block the pain emanating from the injured nerve. In these cases the nerve is identified by ultrasound and the doctor injects a solution containing local anaesthetic and a steroid around the nerve, and by blocking the nerve in this way reduces the pelvic floor pain Recently PRP [Platelet Enriched Plasma] has also been used with good effect in these cases blood is drawn from the patient, and the platelets are concentrated by spinning them in a centrifuge, before they are injected back into the patient around the affected nerve. There is also research ongoing using a similar system to inject stem cells from bone marrow and adipose tissue , in an effort to promote healing in the injured nerve