File
advertisement

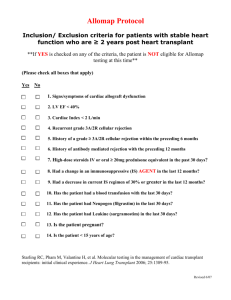
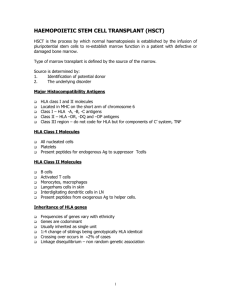
CHAPTER 15 – TRANSPLANTATION OF TISSUES AND ORGANS Transplant rejection and graft-versus-host rejection are immune responses caused by genetic differences between transplant donors and recipients o The most important genetic difference are the antigenic differences in the highly polymorphic HLA class I and class II molecules – aka transplantation antigens or major histocompatibility antigens Antigens such as these, which vary between members of the same species are known as alloantigens; the immune responses they provoke are known as alloreactions o In clinical transplantation, two distinct types of alloreaction can occur: Transplant rejection – after transplantation of solid organs, such as kidney and heart, alloreactions developed by the recipient’s immune system are directed at the cells of the graft and can kill them Graft vs Host reaction – alloreaction arises from mature T cell in grafted bone marrow that attack and reject the recipients healthy tissue – causes graft-versus-host disease, which affects almost all patients who have a bone marrow transplant, to varying degrees o Types of grafts: Autograft – graft of tissue taken from one anatomical site and transplanted to another in the same individual Isograft (syngeneic transplant)- tissue or organ graft from one genetically identical individual to another Allograft (allogeneic transplant) – tissue graft made between genetically non-identical members of the same species Blood transfusion is the most widespread kind of transplantation in clinical medicine o Today, donated blood is commonly separated into erythrocytes, platelets, and plasma and transfusions are only made of those components that a patient needs Plasma replaces fluid and prevents bleeding; erythrocytes improve respiration and metabolism; platelets facilitate clotting to prevent bleeding o Human erythrocytes lack HLA class I and II molecules, which are therefore of little consequence in blood transfusion; however patients still need to be screened for ABO and rhesus alloantigens Problems occur when the transfused patient has preformed antibodies that bind to alloantigens on the transfused erythrocyte and cause their lysis; prior to transfusion of any unit of blood, a cross-match test determines whether the patient has antibodies that react with the donor’s red cells TRANSPLANTATION OF SOLID ORGANS Antibodies against ABO or HLA antigens cause hyperacute rejection of transplanted organs o Hyperacute rejection – rejection of an allogeneic tissue graft as a result of pre-formed antibodies that react against ABO blood group antigens or HLA class I antigens on the graft; the antibodies bind to endothelium and trigger the blood clotting cascades, leading to ischemia and death of the transplanted organ or tissue Anti-HLA antibodies can arise from pregnancy, blood transfusion, or previous transplants o In almost all pregnancies, the fetus expresses paternal HLA isoforms that are not part of the mother’s HLA type and have the potential to cause an alloreactive immune response. During the trauma associated with birth, cells and material of fetal origin enter maternal circulation and stimulate an immune response With successive pregnancies, increasing levels of anti-HLA antibodies can develop and multiparous women are the main source of the anti-HLA sera used in serological HLA typing Has no detrimental effect on subsequent pregnancies, but will complicate any future search for a compatible organ transplant should it be needed o Blood transfusions can also lead to production of anti-HLA antibodies In routine blood transfusion, HLA type is not assessed and so although the donor and recipient are matched for ABO type they are not matched for HLA type; infusion of HLA-incompatible leukocytes and platelets in a blood transfusion can generate antibodies specific for the donor HLA allotypes E to which a patient seeking a transplant has been sensitized to potential donors is assessed by testing their sera against a representative panel of individuals from the population and expressing the number of positive reactions as a percentage of panel reactive antibody – the higher the PRA, the more difficult it is to find a suitable donor o As with blood transfusions, the greater number of transplants that a patient has had leads to a higher PRA number Acute rejection is caused by effector T cells responding to HLA differences between donor and recipient o Most organ transplants are performed across some HLA class I and/or class II difference CD8 T cells respond to the HLA class I differences, and CD4 T cells respond to the class II differences; the alloreactive T cell response produces effector CD4 and CD8 T cells, both of which can attack the organ graft and destroy it – acute rejection (days to develop) To prevent acute rejection, all transplant patients are conditioned with immunosuppressive drugs before transplantation and are maintained on them after transplantation The effector mechanisms underlying acute rejection are just like those caused by type IV hypersensitivity reactions o Direct pathway of allorecognition - type of alloreactive response in which T cells of the recipient of a transplant are stimulated by direct interaction of their receptors with the allogeneic HLA molecules expressed by dendritic cells from the donor, present in the transplant Produces effector T cells that migrate to the transplanted tissue, where TH1 cells activate the resident macrophages to inflame the tissue further an CD8 T cells systematically kill the cells of the transplanted tissues HLA differences between transplant donor and recipient activate numerous alloreactive T cells o Mixed lymphocyte reaction (MLR) assesses the extent to which a patient’s T cells will respond to transplanted tissue Peripheral blood cells from the recipient are mized in tissue culture with lethally irradiated cells from a potential transplant donor; both the proliferation of T cells and the effector function of donor-specific cytotoxic T cells can be measured Chronic rejection of organ transplants is due to the indirect pathway of allorecognition o Chronic rejection – occurs months or years after transplantation and is characterized by reactions in the vasculature of the graft that cause thickening of the vessel walls and a narrowing of their lumina. The blood supply to the graft gradually becomes inadequate, causing ischemia, loss of function, and eventually death of the graft Chronic rejection is correlated with antibodies specific for the HLA class I molecules of the graft o CD4 helper T cells that initiate the response leading to chronic rejection recognize their specific antigens by the indirect pathway of allorecognition In this pathway, some of the donor derived dendritic cells that migrate to the draining lymphoid tissue die there by apoptosis. Membrane fragments containing HLA molecules from these apoptotic cells are taken up by dendritic cells of the transplant recipient and processed so the peptides derived from the donor are presented to the recipients HLA allotypes This pathway is ‘indirect’ because alloreactive T cells do not directly recognize the transplanted cells, but recognize subcellular material that has been processed and presented by the recipients own cells o After transplantation, stimulation of helper CD4 T cells through the indirect pathway can initiate an antibody response against the allogeneic HLA allotypes which then activate naïve B cells that are specific for the HLA allotypes of the graft and provoke a B cell response. This can lead to expansion and epitope spreading of the allogeneic B and T cell response and the gradual impairment of the function of the transplanted organ through the same mechanism that operate in autoimmune disease Allogeneic transplantation is made possible by the use of three types of immunosuppressive drug o Corticosteroids –steroids with anti-inflammatory properties like those of the natural glucocorticosteroid hormones made in the adrenal cortex o Cytotoxic drugs - that interfere with DNA replication and kill proliferating lymphocytes activated by graft alloantigens o Inhibitors of T cell activation signaling pathways o All immunosuppressive drugs are also toxic to other tissues in varying degrees. Because these ‘side-effects’ vary for different drugs, immunosuppressive drugs are commonly used in combination so their immunosuppressive effects are additive, but their toxic effects are not. Corticosteroids change patterns of gene expression o The steroid commonly given to transplant patients is prednisone – a synthetic derivative or hydrocortisone that is 4 times more potent in reducing inflammation; it has no biological activity until it is enzymatically converted in vivo to prednisolone Example of a pro-drug – a drug that is given to patients in the inactive form and becomes chemically or enzymatically converted to the active form within the body By itself, prednisone is insufficient – typically used in combination with a cytotoxic drug o Steroids act at intracellular receptors Corticosteroids are lipid-soluble compounds that diffuse across the plasma membrane and bind to their receptors in the cytosol. The binding to the receptor displaces a dimer of a heat-shock protein (Hsp90), exposing the DNA-binding region of the receptor, which then enters the nucleus and binds to specific DNA sequences in the promoter regions of steroid-responsive genes o Effects of corticosteroids on the immune system Reduce the production of inflammatory mediators, including some cytokines, prostaglandins, and nitric oxide; also indirectly decrease IL-2 synthesis by activated lymphocytes by their effects on other cytokines. Inhibit inflammatory cell migration to sites of inflammation by inhibiting the expression of adhesion molecules Promote the death by apoptosis of leukocytes and lymphocytes o Commonly used as an acute immunosuppressive agent during episodes of rejection, but their continued use is avoided whenever possible - due to side effects such as fluid retention, diabetes, loss of bone mineral, etc. Cytotoxic drugs kill proliferating cells o Azathioprine - a pro-drug used in solid organ transplantation that is converted to 6-mercptopurine and then to 6-thioinosinic acid, which inhibits the production of inosinic acid, an intermediate in the synthesis of adenine and guanine Principal effect is inhibition of DNA replication; drug has no effect on cells until they try to replicate their DNA, whereupon they die o Cytotoxic drugs, although helpful in inhibiting the proliferation of alloantigen-activated lymphocytes, damage all tissues that are normally active in cell division Principally effected are bone marrow, intestinal epithelium, and hair follicles, leading to anemia, leukopenia, thrombocytopenia, intestinal damage and loss of hair o Mycophenolate mofetil is a more recently developed drug with similar effects to azathioprine – it is metabolized in the liver to mycophenolic acid, which prevents cell division by inhibiting inosine monophosphate dehydrogenase, an enzyme necessary for guanine synthesis o Other examples of cytotoxic drugs include: Cyclophosphamide and Methotrexate Cyclosporin A, tacrolimus, and rapamycin selectively inhibit T-cell activation o Cyclosporine A is a cyclic decapeptide derived from a soil fungus, Tolypocladium inflatum, that inhibits the activation of T cells by antigen disrupting the transduction of signals from the T cell receptor Signals typically lead to an elevation of cytosolic calcium concentration which activates the cytoplasmic serine/threonine phosphatase calcineurin, which in turn activates the transcription factor NFAT. Cyclosporin interferes with calcineurin activity It diffuses across the membrane into the cytosol, where it binds peptidyl-prolyl isomerase enzymes (cyclophilins). The complex of cyclosporin A and cyclophilin binds to calcineurin, inhibiting its phosphatase activity and preventing activation of NFAT o Tacrolimus, also called FK506, is a macrolide that suppressed T cell activation by the inhibition of calcineurin through a similar mechanism to that of cyclosporin A The peptidly-prolyl isomerases to which tacrolimus binds are distinct from cyclophilins, and are known as FK binding proteins FK binding proteins and cyclophilins are collectively known as immunophilins o Although the principal effect of cyclosporin A and tacrolimus is to inhibit T cell activation, the activation of B cells is also suppressed Main benefit: drugs do not target proliferating cells, so the reduced hematopoiesis and intestinal damage seen in cytotoxic drugs does not occur Major side effect – nephrotoxicity o Rapamycin (aka sirolimus) is an immunosuppressive macrolide that binds to FK-binding proteins, but does not interfere with calcineurin. Instead, it blocks T cell activation at a later stage by preventing signal transduction from the IL-2 receptor. it is more toxic that either cyclosporin A or tacrolimus, but has become a useful component in combination therapy Antibodies specific for T cells are used to prevent and control acute rejection o Early symptoms of rejection are treated with 5 to 15 day courses of T cell specific antibody injection, as well as increased dosages of immunosuppressant drugs o Polyclonal anti-T cell antibodies are made in sheep and goats that have been immunized with human thymocytes or lymphocytes. Antibody containing fractions called anti-thymocyte globulin (ATG) or anti-lymphocyte globulin (ALG) are prepared ALG and ATG cause destruction of lymphocytes to which they bind, through complement fixation and phagocytosis o Monoclonal anti-CD3 interferes with T cell function by reducing the number of CD3:T cell receptor complexes on T cells o Both anti-T cell antibodies and anti-CD3 are xenogeneic, that is, they come from a non-human species, and stimulate an immune response against them –therefore they are only effective one time This is because the patient’s antibodies form immune complexes with the immunosuppressive antibodies, clearning them from circulation before they can bind to T cells