Reference Range
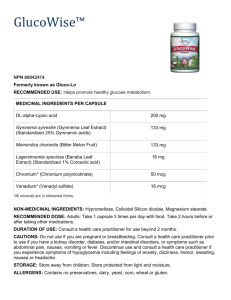
advertisement

Therapeutic Drug Monitoring TDM is a branch of clinical chemistry and clinical pharmacology that specializes in the measurement of medication concentrations in blood. Its main focus is on drugs with a narrow therapeutic range, i.e. drugs that can easily be under- or overdosed. Indications for therapeutic drug monitoring include: There is an experimentally determined relationship between plasma drug concentration and the pharmacological effect. Knowledge of the drug level influences management. There is narrow therapeutic window. There are potential patient compliance problems. The drug dose cannot be optimized by clinical observation alone. Examples of drugs analyzed by therapeutic drug monitoring: Antibiotics.(aminoglycosides , glycopeptides ). Antiepileptics (such as carbamazepine, phenytoin and valproic acid). Mood stabilizers, especially lithium citrate. Antipsychotics (such as pimozide and clozapine). Cardiac agents( antiarrythimcs , glycosides ). Immunosuppressant . Bronchodilators . Antineoplastic.. Analgesics . Addictions therapeutics . Anticoagulants . Clinical usefulness of TDM : TDM data provides the clinician with greater insight into the factors determining the patients response to drug therapy. For example when a patient fails to respond to a usual measurement of plasma level can help to distinguish a noncompliant ,therapeutic dose patient and a patient who is a true non-responder. TDM also provides useful information regarding individual variations in drug utilization patterns and alteration in drug TDM is a .utilization as a consequence of altered physiological state or disease process useful adjunct in treating many patients provided the potential pit falls and problems are .considered Antibiotics 1-Aminoglycosides :(Amikacin) Therapeutic levels: Peak: Life-threatening infections: 25-40 mcg/mL Serious infections: 20-25 mcg/mL Urinary tract infections: 15-20 mcg/mL Trough: <8 mcg/mL The American Thoracic Society (ATS) recommends trough levels of <4-5 mcg/mL for patients with hospital-acquired pneumonia. Toxic concentration: Peak: >40 mcg/mL; Trough: >10 mcg/mL Optimum sampling time: Draw peak 30 minutes after completion of 30-minute infusion or at 1 hour following initiation of infusion or I.M. injection. Draw trough within 30 minutes prior to next dose. Time to steady state: Route of elimination: Half life : 10-15 h with normal renal function. > 90 % excreted renally. Adults: Normal renal function: 1.4-2.3 hours; Anuria/end-stage renal disease: 28-86 hours. 2-Aminoglcosides (Gentamicin ): Therapeutic range : Peak: Serious infections: 6-8 mcg/mL (12-17 micromole/L) Life-threatening infections: 8-10 mcg/mL (17-21 micromole/L) Urinary tract infections: 4-6 mcg/mL Synergy against gram-positive organisms: 3-5 mcg/mL Trough: Serious infections: 0.5-1 mcg/mL Life-threatening infections: 1-2 mcg/mL The American Thoracic Society (ATS) recommends trough levels of <1 mcg/mL for patients with hospital-acquired pneumonia. Obtain drug levels after the third dose unless renal dysfunction/toxicity suspected Optimum sampling time: Time to steady state : Route of elimination: Half life : Timing of serum samples: Draw peak 30 minutes after 30-minute infusion has been completed or 1 hour after I.M. injection; draw trough immediately before next dose. 10-15 h with normal renal function. >90% renally execrated . Adults: 1.5-3 hours; End-stage renal disease: 36-70 hours 3-Aminogylcosides (Tobramycin ): Therapeutic levels: Peak: Serious infections: 6-8 mcg/mL (SI: 12-17 micromole/L) Life-threatening infections: 8-10 mcg/mL (SI: 17-21 micromole/L) Urinary tract infections: 4-6 mcg/mL (SI: 7-12 micromole/L) Synergy against gram-positive organisms: 3-5 mcg/mL Trough: Serious infections: 0.5-1 mcg/mL Life-threatening infections: 1-2 mcg/mL The American Thoracic Society (ATS) recommends trough levels of <1 mcg/mL for patients with hospital-acquired pneumonia. Monitor serum creatinine and urine output; obtain drug levels after the third dose unless otherwise directed Inhalation: Serum levels are ~1 mcg/mL one hour following a 300 mg dose in patients with normal renal function. Optimum sampling time: Draw peak 30 minutes after 30-minute infusion has been completed or 1 hour following I.M. injection or beginning of infusion. draw trough immediately before next dose. Time to steady state : Route of elimination: Half life : 10-15 h with normal renal function. >90% renally execrated . Adults: I.V.: 2-3 hours; directly dependent upon glomerular filtration rate; Inhalation: ~4 hours Adults with impaired renal function: 5-70 hours. 4- Glycopeptides :Vancomycin: Therapeutic levels: Trough: ≥10 mcg/mL. For pathogens with an MIC ≤1 mcg/mL, the minimum trough concentration should be 15 mcg/mL to meet target AUC/MIC of ≥400 (see "Note" below). For complicated infections (eg, bacteremia, endocarditis, osteomyelitis, meningitis, and hospital-acquired pneumonia caused by S. aureus), trough concentrations of 15-20 mcg/mL are recommended to improve penetration and improve clinical outcomes (Liu, 2011; Rybak, 2009). The American Thoracic Society (ATS) guidelines for hospital-acquired pneumonia and the Infectious Disease Society of America (IDSA) meningitis guidelines also recommend trough concentrations of 15-20 mcg/mL. Note: Although AUC/MIC is the preferred pharmacokineticpharmacodynamic parameter used to determine clinical effectiveness, trough serum concentrations may be used as a surrogate marker for AUC and are recommended as the most accurate and practical method of vancomycin monitoring (Liu, 2011; Rybak, 2009). Toxic: >80 mcg/mL (SI: >54 micromole/L) Optimum sampling time: Time to steady state : Route of elimination: Half life : Draw trough just before the administration of a dose at steady-state conditions. Steady state conditions generally occur approximately after the fourth dose. Drawing peak concentrations is no longer recommended. 10-15 h with normal renal function. 80% renally execrated . Adults: 5-11 hours; significantly prolonged with renal impairment End-stage renal disease: 200-250 hours. Antiepileptic 1-Phenytoin: Therapeutic levels: Total phenytoin: 10-20 mcg/mL (SI: 40-79 micromole/L) (children and adults), 8-15 mcg/mL (SI: 32-59 micromole/L) (neonates) Concentrations of 5-10 mcg/mL (SI: 20-40 micromole/L) may be therapeutic for some patients but concentrations <5 mcg/mL (SI: <20 micromole/L) are not likely to be effective 50% of patients show decreased frequency of concentrations >10 mcg/mL (SI: >40 micromole/L) seizures at 86% of patients show decreased frequency of concentrations >15 mcg/mL (SI: >59 micromole/L) seizures at Add another anticonvulsant if satisfactory therapeutic response is not achieved with a phenytoin concentration of 20 mcg/mL (SI: 79 micromole/L) Free phenytoin: 1-2.5 mcg/mL (SI: 4-10 micromole/L) Total phenytoin: Toxic: >30 mcg/mL (SI: >119 micromole/L) Lethal: >100 mcg/mL (SI: >396 micromole/L) Optimum sampling time: Because it is slowly absorbed, peak blood levels may occur 4-8 hours after ingestion of an oral dose. The serum half-life varies with the dosage and the drug follows Michaelis-Menten kinetics. Children and Adults: Toxicity is measured clinically, and some patients require levels outside the suggested therapeutic range Time to steady state : Route of elimination: Half life : 2-Valproic acid: 5-10 days. 80% renally execrated . 24 hours. Therapeutic levels: Therapeutic: Epilepsy: 50-100 mcg/mL (SI: 350-700 micromole/L); although seizure control may improve at levels >100 mcg/mL (SI: 700 micromole/L), toxicity may occur at levels of 100-150 mcg/mL (SI: 700-1040 micromole/L) Mania: 50-125 mcg/mL (SI: 350-875 micromole/L) Toxic: Some laboratories may report >200 mcg/mL (SI: >1390 micromole/L) as a toxic threshold, although clinical toxicity can occur at lower concentrations. Probability of thrombocytopenia increases with total valproate levels ≥110 mcg/mL in females or ≥135 mcg/mL in males. Epilepsy: Although seizure control may improve at levels >100 mcg/mL (SI: 700 micromole/L), toxicity may occur at levels of 100-150 mcg/mL (SI: 700-1050 micromole/L) Mania: Clinical response seen with trough levels between 50-125 mcg/mL (SI: 350-875 micromole/L); risk of toxicity increases at levels >125 mcg/mL (SI: 875 micromole/L). Optimum sampling time: Time to steady state : Route of elimination: Half life : 3-Carbamazipene: Therapeutic levels: In general, trough concentrations should be used to assess adequacy of therapy; peak concentrations may also be drawn if clinically necessary (eg, concentration-related toxicity). Within 2-4 days of initiation or dose adjustment, trough concentrations should be drawn just before the next dose (extended-release preparations) or before the morning dose (for immediaterelease preparations). Patients with epilepsy should not delay taking their dose for >2-3 hours. Additional patient-specific factors must be taken into consideration when interpreting drug levels, including indication, age, clinical response, pregnancy status, adherence, comorbidities, adverse effects, and concomitant medications (Patsalos, 2008; Reed, 2006). Renally. 9-19 hours. Epilepsy: Therapeutic levels: 4-12 mcg/mL (SI: 17-51 micromole/L) Toxic concentration: >15 mcg/mL; patients who require higher levels of 8-12 mcg/mL (SI: 34-51 micromole/L) should be watched closely. Side effects including CNS effects occur commonly at higher dosage levels. If other anticonvulsants are given therapeutic range is 4-8 mcg/mL Optimum sampling time: Time to steady state : Route of elimination: Half life : Absorption is slow, peak levels occur 8-65 hours after ingestion of the first dose; the half-life ranges from 8-60 hours, therefore, steady-state is achieved in 2-5 days. 2-5 days . Renally. 8-60 hrs . 4- Lamotrigen: A therapeutic serum concentration range has not been established for lamotrigine. Dosing should be based on therapeutic response. Lamotrigine plasma concentrations of 0.25-29.1 mcg/mL have been reported in the literature 5-Ethsuximide : Reference Range: Therapeutic: 40-100 mcg/mL 6-Primidone: Serum primidone and phenobarbital concentration, neurological status. Due to CNS effects, monitor closely when initiating drug in elderly. Monitor CBC and sequential multiple analysis-12 (SMA-12) at 6-month intervals to compare with baseline obtained at start of therapy. Monitor for suicidality (eg, suicidal thoughts, depression, behavioral changes). Since elderly metabolize phenobarbital at a slower rate than younger adults, it is suggested to measure both primidone and phenobarbital levels together. Reference Range: Therapeutic: Children <5 years: 7-10 mcg/mL (SI: 32-46 micromole/L); Adults: 5-12 mcg/mL (SI: 23-55 micromole/L); toxic effects rarely present with levels <10 mcg/mL (SI: 46 micromole/L) if phenobarbital concentrations are low. Dosage of primidone is adjusted with reference mostly to the phenobarbital level; Toxic: >15 mcg/mL (SI: >69 micromole/L) 7-Phenobarbital: Reference Range: Therapeutic: Infants and Children: 15 to 40 mcg/mL (SI: 65 to 129 micromole/L) Adults: 20 to40 mcg/mL (SI: 86 to 172 micromole/L) Toxic: >40 mcg/mL (SI: >172 micromole/L) Toxic concentration: Slowness, ataxia, nystagmus: 35 to 80 mcg/mL (SI: 150 to 344 micromole/L) Coma with reflexes: 65 to 117 mcg/mL (SI: 279 to 502 micromole/L) Coma without reflexes: >100 mcg/mL (SI: >430 micromole/L) 8-Fosphenytoin: Reference Range Therapeutic: 10-20 mcg/mL (SI: 40-79 micromole/L); toxicity is measured clinically, and some patients require levels outside the suggested therapeutic range Toxic: >30 mcg/mL (SI: 120 micromole/L) Lethal: >100 mcg/mL (SI: >400 micromole/L) Manifestations of toxicity: Nystagmus: 20 mcg/mL (SI: 79 micromole/L) Ataxia: 30 mcg/mL (SI: 118.9 micromole/L) Decreased mental status: 40 mcg/mL (SI: 159 micromole/L) Coma: 50 mcg/mL (SI: 200 micromole/L) Peak serum phenytoin level after a 375 mg I.M. fosphenytoin dose in healthy males: 5.7 mcg/mL Peak serum fosphenytoin levels and phenytoin levels after a 1.2 g infusion (I.V.) in healthy subjects over 30 minutes were 129 mcg/mL and 17.2 mcg/mL, respectively. Cardiac glycosides : Digoxin: Therapeutic levels: Digoxin therapeutic serum concentrations: Heart failure: 0.5 to 0.9 ng/mL (ACCF/AHA [Yancy, 2013]) Adults: <0.5 ng/mL; probably indicates underdigitalization unless there are special circumstances Toxic: >2 ng/mL Digoxin-like immunoreactive substance (DLIS) may cross-react with digoxin immunoassay. DLIS has been found in patients with renal and liver disease, heart failure, neonates, and pregnant women (3rd trimester). Optimum sampling time: When to draw serum digoxin concentrations: Digoxin serum concentrations are monitored because digoxin possesses a narrow therapeutic serum range; the therapeutic endpoint is difficult to quantify and digoxin toxicity may be life-threatening. Digoxin serum concentrations should be drawn at least 6 to 8 hours after last dose, regardless of route of administration (optimally 12 to 24 hours after a dose). Note: Serum digoxin concentrations may decrease in response to exercise due to increased skeletal muscle uptake; a period of rest (eg, ~2 hours) after exercise may be necessary prior to drawing serum digoxin concentrations. Initiation of therapy: If a loading dose is given: Digoxin serum concentration may be drawn within 12 to 24 hours after the initial loading dose administration. Concentrations drawn this early may confirm the relationship of digoxin plasma concentrations and response but are of little value in determining maintenance doses. If a loading dose is not given: Digoxin serum concentration should be obtained after 3 to 5 days of therapy. Maintenance therapy: Trough concentrations should be followed just prior to the next dose or at a minimum of 6 to 8 hours after last dose. Digoxin serum concentrations should be obtained within 5 to 7 days (approximate time to steady-state) after any dosage changes. Continue to obtain digoxin serum concentrations 7 to 14 days after any change in maintenance dose. Note: In patients with end-stage renal disease, it may take 15 to 20 days to reach steady-state. Patients who are receiving electrolyte-depleting medications such as diuretics, serum potassium, magnesium, and calcium should be monitored closely. Digoxin serum concentrations should be obtained whenever any of the following conditions occur: Questionable patient compliance or to evaluate deterioration following an initial good response clinical Changing renal function Suspected digoxin toxicity Initiation or discontinuation of therapy with drugs (eg, amiodarone, quinidine, verapamil) which potentially interact with digoxin. Any disease changes (eg, thyroid disease) Time to steady state : Route of elimination: 2-5 days . Renally. Half life : Adults: 36 to 48 hours Adults, anephric: 3.5 to 5 days . 2- Procinamide: Reference Range: Timing of serum samples: Draw 6 to 12 hours after I.V. infusion has started; half-life is 2.5 to 5 hours Therapeutic concentrations: Procainamide: 4 to 10 mcg/mL; NAPA 15 to 25 mcg/mL; Combined: 10 to 30 mcg/mL Toxic concentration: Procainamide: >10 to 12 mcg/mL 3-Flecinide : Reference Range Therapeutic: 0.2-1 mcg/mL; pediatric patients may respond at the lower end of the recommended therapeutic range Analgesics : Aspirin . Serum Salicylate: Clinical Correlations serum Salicylate Concentration Desired Effects Adverse Effects / Intoxication (mcg/mL) Antiplatelet ~100 Antipyresis GI intolerance and bleeding, hypersensitivity, hemostatic defects Analgesia 150-300 Anti-inflammatory Mild salicylism 250-400 Treatment of rheumatic fever Nausea/vomiting, hyperventilation, salicylism, flushing, sweating, thirst, headache, diarrhea, and tachycardia serum Salicylate Concentration Desired Effects Adverse Effects / Intoxication (mcg/mL) Respiratory alkalosis, hemorrhage, excitement, confusion, asterixis, pulmonary edema, convulsions, tetany, metabolic acidosis, fever, coma, cardiovascular collapse, renal and respiratory failure >400-500 Methadone : Reference Range Prevention of opioid withdrawal: Therapeutic: 100 to 400 ng/mL (SI: 0.32 to 1.29 micromole/L); Toxic: >2 mcg/mL (SI: >6.46 micromole/L) Immunosuppressants 1-Tacrolimus: (refrence range) Heart transplant: Typical whole blood trough concentrations: Months 1-3: 10-20 ng/mL Months ≥4: 5-15 ng/mL Kidney transplant: Whole blood trough concentrations: Immediate release: In combination with azathioprine: Months 1-3: 7-20 ng/mL Months 4-12: 5-15 ng/mL In combination with mycophenolate mofetil/IL-2 receptor antagonist (eg, daclizumab): Months 1-12: 4-11 ng/mL Extended release: With basiliximab induction: Days 1-60: 5-17 ng/mL Month 3-12: 4-12 ng/mL Without induction: Days 1-60: 6-20 ng/mL Month 3-12: 6-14 ng/mL Liver transplant: Whole blood trough concentrations: Months 1-12: 5-20 ng/mL Recommended therapeutic ranges when administered in combination with everolimus for liver transplant (Zortress product labeling, 2013): By 3 weeks after first everolimus dose and through month 12 post-transplant: 3-5 ng/mL Prevention of graft-versus-host disease (unlabeled use): 10-20 ng/mL (Uberti, 1999) although some institutions use a lower limit of 5 ng/mL and an upper limit of 15 ng/mL (Przepiorka, 1999; Yanik, 2000).. 2-Sirolimus: Reference Range: Note: Sirolimus concentrations are dependent on the assay method (eg, chromatographic and immunoassay) used; assay methods are not interchangeable. Determine the assay method used to assure consistency (or accommodations if changes occur) and for monitoring purposes, be aware of alterations to assay method or reference range. Serum trough concentration goals for renal transplantation (based on HPLC methods): Concomitant cyclosporine: 4-12 ng/mL Low-to-moderate immunologic risk (after cyclosporine withdrawal): 16-24 ng/mL for the first year after transplant; after 1 year: 12-20 ng/mL High immunologic risk (with cyclosporine): 10-15 ng/mL Note: Trough concentrations vary based on clinical context and use of additional immunosuppressants. The following represents typical ranges. When combined with tacrolimus and mycophenolate mofetil (MMF) without steroids: 6-8 ng/mL As a substitute for tacrolimus (starting 4-8 weeks post-transplant), in combination with MMF and steroids: 8-12 ng/mL Following conversion from tacrolimus to sirolimus >6 months post-transplant due to chronic allograft nephropathy: 4-6 ng/mL Serum trough concentrations for heart transplantation (unlabeled use): With calcineurin inhibitor (eg, cyclosporine): 4-12 ng/mL (Costanzo, 2010) Without calcineurin inhibitor: 10-15 ng/mL (Raichlin, 2007a; Raichlin, 2007b) Following conversion from cyclosporine or tacrolimus to sirolimus: Initial (maintained until completion of conversion [~2 weeks]): 8-14 ng/mL (Topilsky, 2012) or 9-15 ng/mL (Zuckermann, 2012); Maintenance: 10-15 ng/mL (Kushwaha, 2005) or 7-15 ng/mL (Zuckermann, 2012) Serum trough concentrations for GVHD prophylaxis in allogeneic stem cell transplant (unlabeled use): 3-12 ng/mL (Armand, 2008; Cutler, 2007) Serum trough concentrations for advanced chordoma (unlabeled use): 15-20 ng/mL (Stacchiotti, 2009) Serum trough concentrations for renal angiomyolipoma or lymphangioleiomyomatosis (unlabeled use): 3-6 ng/mL; may increase to 6-10 ng/mL if <10% reduction in lesion diameters at 2 months (Davies, 2011) or 5-15 ng/mL (McCormack, 2011) 3-Cyclosporine : Reference Range Reference ranges are method dependent and specimen dependent; use the same analytical method consistently Method-dependent and specimen-dependent: Trough levels should be obtained: Oral: 12-18 hours after dose (chronic usage) I.V.: 12 hours after dose or immediately prior to next dose Therapeutic range: Not absolutely defined, dependent on organ transplanted, time after transplant, organ function and CsA toxicity: General range of 100-400 ng/mL Toxic level: Not well defined, nephrotoxicity may occur at any level Recommended cyclosporine therapeutic ranges when administered in combination with everolimus for renal transplant (Zortress product labeling, 2013): Month 1 post-transplant: 100-200 ng/mL Months 2 and 3 post-transplant: 75-150 ng/mL Months 4 and 5 post-transplant: 50-100 ng/mL Months 6-12 post-transplant: 25-50 ng/mL Monitor blood pressure and serum creatinine after any cyclosporine dosage changes or addition, modification, or deletion of other medications. Monitor plasma concentrations periodically. Nephrotic syndrome (Canadian labeling): Baseline blood pressure (2 readings within 2 weeks), fasting serum creatinine (at least 3 levels within 2 weeks), creatinine clearance, urinalysis, CBC, liver function, serum uric acid, serum potassium, and malignancy screening (eg, skin, mouth, lymph nodes). Biweekly monitoring of blood pressure for initial 3 months and then monthly thereafter, frequent monitoring of renal function and periodic cyclosporine trough levels are recommended during therapy. Consider renal biopsy in patients with steroiddependent minimal change neuropathy who have been maintained on therapy >1 year. Transplant patients: Cyclosporine trough levels, serum electrolytes, renal function, hepatic function, blood pressure, lipid profile Psoriasis therapy: Baseline blood pressure, serum creatinine (2 levels each), BUN, CBC, serum magnesium, potassium, uric acid, lipid profile. Biweekly monitoring of blood pressure, complete blood count, serum creatinine, and levels of BUN, uric acid, potassium, lipids, and magnesium during the first 3 months of treatment for psoriasis. Monthly monitoring is recommended after this initial period. (Note: The Canadian labeling recommends bimonthly monitoring of serum creatinine after the initial period if serum creatinine remains stable and cyclosporine dose is ≤2.5 mg/kg daily, and monthly monitoring for higher doses). Also evaluate any atypical skin lesions prior to therapy. Increase the frequency of blood pressure monitoring after each alteration in dosage of cyclosporine. Rheumatoid arthritis: Baseline blood pressure, and serum creatinine (2 levels each); serum creatinine every 2 weeks for first 3 months, then monthly if patient is stable. Increase the frequency of blood pressure monitoring after each alteration in dosage of cyclosporine. Additional Canadian labeling recommendations include CBC, hepatic function, urinalysis, serum potassium and uric acid (baseline and periodic thereafter). Psychoactive agents : 1-Amytriptyline: Reference Range; Therapeutic: Amitriptyline plus nortriptyline 80-250 ng/mL (SI: 288-900 nmol/L); amitriptyline plus nortriptyline levels >300 ng/mL are associated with increased side effects; plasma levels do not always correlate with clinical effectiveness (Am J Psychiatry, 1985; Boyer, 1984; Orsulak, 1979) 2-Clozapine : Reference Range; Clozapine levels >350 ng/mL may be associated with an increased likelihood of clinical response. However, increases of serum concentrations above this have not been shown to confer greater improvements and may increase the risk of adverse events (Remington 2013). 3-Haloperidol: Reference Range: Therapeutic: 5-20 ng/mL (SI: 10-40 nmol/L) (psychotic disorders - less for Tourette's and mania) Toxic: >42 ng/mL (SI: >84 nmol/L) 4-Fluoxetine : Reference Range: Therapeutic levels have not been well established Therapeutic: Fluoxetine: 100-800 ng/mL (SI: 289-2314 nmol/L); Norfluoxetine: 100-600 ng/mL (SI: 289-1735 nmol/L) Toxic: Fluoxetine plus norfluoxetine: >2000 ng/mL 5-Lithium : Serum lithium every 4-5 days during initial therapy; draw lithium serum concentrations 8-12 hours postdose; renal, thyroid, and cardiovascular function; fluid status; serum electrolytes; CBC with differential, urinalysis; monitor for signs of toxicity; beta-hCG pregnancy test for all females not known to be sterile. Canadian labeling (additional monitoring recommendations): Serum calcium prior to initiation of therapy, at 6 months, and annually thereafter during prolonged therapy. Reference Range: Levels should be obtained twice weekly until both patient's clinical status and levels are stable then levels may be obtained every 1-3 months Timing of serum samples: Draw trough just before next dose (8-12 hours after previous dose) Therapeutic levels: Acute mania: 0.6-1.2 mEq/L (SI: 0.6-1.2 mmol/L) Protection against future episodes in most patients with bipolar disorder: 0.8-1 mEq/L (SI: 0.8-1.0 mmol/L); a higher rate of relapse is described in subjects who are maintained at <0.4 mEq/L (SI: 0.4 mmol/L) Elderly patients can usually be maintained at lower end of therapeutic range (0.6-0.8 mEq/L) Toxic concentration: >1.5 mEq/L (SI: >1.5 mmol/L) Adverse effect levels: GI complaints/tremor: 1.5-2 mEq/L Confusion/somnolence: 2-2.5 mEq/L Seizures/death: >2.5 mEq/L Anticoagulants : 1-Heparin (UFH): Reference Range: Venous thromboembolism: Heparin: 0.3-0.7 unit/mL (children: 0.35-0.7 unit/mL) anti-Xa activity (by chromogenic assay) or 0.2-0.4 unit/mL (by protamine titration); aPTT: 1.5-2.5 times control (usually reflects an aPTT of 60-85 seconds) (Garcia, 2012; Monagle, 2012) When used with thrombolytic therapy in patients with acute MI, a lower therapeutic range corresponding to an aPTT of 1.5-2 times control (or approximately an aPTT of 50-70 seconds) is recommended (Antman, 2004) For intermittent I.V. injections, aPTT is measured 3.5-4 hours after I.V. injection. Note: Continuous I.V. infusion is preferred over I.V. intermittent injections. For full-dose heparin (ie, nonlow-dose), the dose should be titrated according to aPTT results. For anticoagulation, an aPTT 1.5-2.5 times normal is usually desired. Because of variation among hospitals in the control aPTT values, nomograms should be established at each institution, designed to achieve aPTT values in the target range (eg, for a control aPTT of 30 seconds, the target range [1.5-2.5 times control] would be 45-75 seconds). Measurements should be made prior to heparin therapy, 6 hours (pediatric: 4 hours) after initiation, and 6 hours (pediatric: 4 hours) after any dosage change, and should be used to adjust the heparin infusion until the aPTT exhibits a therapeutic level. When two consecutive aPTT values are therapeutic, subsequent measurements may be made every 24 hours, and if necessary, dose adjustment carried out. In addition, a significant change in the patient's clinical condition (eg, recurrent ischemia, bleeding, hypotension) should prompt an immediate aPTT determination, followed by dose adjustment if necessary. In general, may increase or decrease infusion by 2-4 units/kg/hour dependent upon aPTT. 2-Enoxaparin: Monitoring Parameters Platelets, occult blood, anti-Xa levels, serum creatinine; monitoring of PT and/or aPTT is not necessary. Routine monitoring of anti-Xa levels is not required, but has been utilized in patients with obesity and/or renal insufficiency. Monitoring anti-Xa levels is recommended in pregnant women receiving therapeutic doses of enoxaparin or when receiving enoxaparin for the prevention of thromboembolism with mechanical heart valves (Guyatt, 2012). For patients >190 kg, if anti-Xa monitoring is available, adjusting dose based on anti-Xa levels is recommended; if anti-Xa monitoring is unavailable, reduce dose if bleeding occurs (Nutescu, 2009). Monitor obese patients closely for signs/symptoms of thromboembolism. Reference Range: The following therapeutic ranges for anti-Xa levels have been suggested, but have not been validated in a controlled trial. Anti-Xa level measured 4 hours postdose. Treatment of venous thromboembolism: Anti-Xa concentration target (Garcia, 2012): Once-daily dosing: >1 anti-Xa units/mL; the manufacturer recommends a range of 1-2 antiXa units/mL Twice-daily dosing: 0.6-1 anti-Xa units/mL Recurrent VTE prophylaxis in pregnant women: Peak anti-Xa concentrations: 0.2-0.6 units/mL (Bates, 2012) 3-Tinzaparin: Monitoring Parameters: CBC (at baseline then twice weekly throughout therapy); renal function (use Cockcroft-Gault formula); hepatic function; potassium (baseline in patients at risk for hyperkalemia, monitor regularly if duration >7 days); stool for occult blood. Routine monitoring of anti-Xa levels is generally not recommended; however, anti-Xa levels may be beneficial in certain patients (eg, children, obese patients, patients with severe renal insufficiency receiving therapeutic doses, and possibly pregnant women receiving therapeutic doses) (Guyatt, 2012). Peak anti-Xa levels are measured 4-6 hours after administration. Monitoring of PT and/or aPTT is not of clinical benefit. Reference Range: Anti-Xa level (measured 4 hours after administration): Fixed-dose (3500 units): 0.15 anti-Xa units/mL; weight-based (75-175 units/kg): 0.34-0.70 anti-Xa units/mL; in treatment of venous thromboembolism, a target of 0.85 anti-Xa units/mL has been recommended (Garcia, 2012) Children: Target anti-Xa level: 0.5-1 anti-Xa units/mL 4-6 hours after administration or 0.5-0.8 anti-Xa units/mL 2-6 hours after administration (Monagle, 2012 4-Fondaparinux: Reference Range Note: Routine monitoring is not recommended; the following fondaparinux-specific anti-Xa concentrations have been reported (Garcia, 2012): Thromboprophylaxis dose: Anti-Xa activity at 3 hours post dose: ~ 0.39-0.5 mg/L Therapeutic dosing (eg, 7.5 mg once daily): Anti-Xa activity at 3 hours post dose: 1.2-1.26 mg/L 5-Dalteparin: Monitoring Parameters: Periodic CBC including platelet count; stool occult blood tests; monitoring of PT and PTT is not necessary. Once patient has received 3-4 doses, anti-Xa levels, drawn 4-6 hours after dalteparin administration, may be used to monitor effect in patients with severe renal dysfunction or if abnormal coagulation parameters or bleeding should occur. For patients >190 kg, if anti-Xa monitoring is available, adjusting dose based on anti-Xa levels is recommended; if anti-Xa monitoring is unavailable, reduce dose if bleeding occurs (Nutescu, 2009). Reference Range: Recurrent VTE prophylaxis in pregnant women: Peak anti-Xa concentrations: 0.2-0.6 units/mL (Bates, 2012) Treatment of venous thromboembolism: Peak anti-Xa concentration target (measured 4 hours after administration): Once-daily dosing: 1.05 anti-Xa units/mL (Garcia, 2012); per the manufacturer, target anti-Xa range is 0.5-1.5 units/mL (measured 4-6 hours after administration and after patient received 3-4 doses) 6-Wafrarin: Adult Target INR Ranges Based Upon Indication: Targeted INR Targeted INR Range Anterior myocardial infarction with LV thrombus or high risk for LV thrombus (EF<40%, anteroapical wall motion abnormality)1,2 2.5 2-3 Atrial fibrillation (nonvalvular)3 or atrial flutter 2.5 2-3 LV systolic dysfunction (without established CAD) with an LV thrombus (eg, Takotsubo cardiomyopathy) 2.5 2-3 2.5 2-3 Indication Cardiac Valvular Carbomedics or St. Jude Medical bileaflet or Medtronic Hall tilting disk mechanical aortic valve in normal sinus rhythm and normal LA size4 Adult Target INR Ranges Based Upon Indication: Targeted INR Targeted INR Range Bileaflet or tilting disk mechanical mitral valve4 3 2.5-3.5 Caged ball or caged disk mechanical valve4 3 2.5-3.5 2.5 2-3 3 2.5-3.5 Bioprosthetic mitral valve6 2.5 2-3 Rheumatic mitral valve disease (particularly mitral stenosis) and normal sinus rhythm (LA diameter >5.5 cm), AF, previous systemic embolism, or LA thrombus 2.5 2-3 2.5 2-3 Idiopathic pulmonary artery hypertension (IPAH)8 2 1.5-2.5 Antiphospholipid syndrome (no other risk factors) 2.5 2-3 Antiphospholipid syndrome and recurrent thromboembolism 2.5 2-3 Total hip or knee replacement or hip fracture surgery9 2.5 2-3 Ischemic stroke due to AF10 2.5 2-3 Cryptogenic stroke (recurrent) and either patent foramen ovale (PFO) or atrial septal aneurysm 2.5 2-3 Indication Mechanical aortic valve5 Mechanical mitral valve or mechanical valves in both the aortic and mitral positions5 Thromboembolism Treatment Venous thromboembolism 7 Thromboprophylaxis Other Indications