this Outline - Alcohol Medical Scholars Program
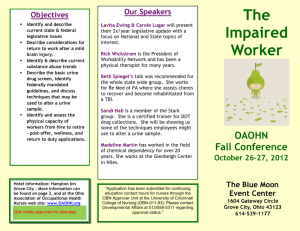
advertisement

1 Monitoring Abstinence By Martin H. Plawecki, M.D. Ph.D. Prepared for the Alcohol Medical Scholars Program (Slide 1) I. Introduction (Slide 2) A. Many diseases are chronic relapsing, and remitting conditions1 – controlled, not cured 1. Type I Diabetes: 30-50% Relapse Rate 2. High blood pressure: 50-70% Relapse Rate 3. Substance use disorders (SUDs): 40-60% Relapse Rate B. Goals of SUD treatment vary (Slide 3) 1. Harm reduction a. Definition: reduce (not eliminate) substance use and consequences b. Example: methadone maintenance (to be discussed more later) 2. Abstinence (ex. Alcoholics Anonymous (AA) and 12-step programs) C. Abstinence monitoring has a role in both types (e.g., regarding heroin for methadone treatment) D. Physicians need to know: 1. Methods for monitoring abstinence 2. Reasons to monitor E. To address these issues, this lecture will cover: (Slide 4) 1. Definition and natural history (i.e., course) of Substance Use Disorders (SUDs) 2 2. Goals of monitoring abstinence and detection 3. Abstinence monitoring substance examples 4. Efficacy of monitored abstinence II. Definitions & Course of Substance Use Disorders (SUDs) (Slide 5) A. Definitions and course specifiers 1. DSM-5 SUD definition: in the same yr, ≥2 2 (Slide 6) a. Tolerance (needing more to get same effects as past lower doses) b. Withdrawal (symptoms that begin when stop or cut down) c. Use longer/more than intended d. Unable to ↓ use e. Significant time spent obtaining, using, recovering f. ↓Activities in order to use g. Use despite medical or psychological problems (liver failure, depression) h. Craving or strong urge/desire to use i. Failed roles because of use (parenting/home, work, school) j. Hazardous use (e.g., while driving) k. Social/interpersonal problems from substances (divorce, loss of friends) B. SUDs are relapsing/remitting conditions that fluctuate between (Slide 7) 1. Abstinence3 3 a. Abstinent: 7% w/ alcohol use disorder recovery had symptom recurrence in 3 yrs b. Not abstinent: >26% recur in 3 yrs 2. Temporary controlled use – e.g. <4 drinks/d; no problems4 3. Problems/crises – recurrence of SUD Sx, even if not full diagnostic criteria III. Goals of monitoring abstinence and detection (Slide 8) A. Goals of monitoring abstinence (Slide 9) 1. Improve treatment outcomes by a. Improving treatment compliance 1’. Verifying prescription usage 2’. Detect problems b. Safety 2. Objective is not punitive B. Basics of detection 1. Detection is primarily based upon pharmacokinetics (what body does to the drug) (Slide 10) a. Absorption – how and how much drug enters the body b. Distribution – where drug goes in body (blood, urine, hair, etc.) c. Metabolism – what body does to drug to deactivate it d. Elimination – how drug/metabolite is eliminated 2. Strategies (Slide 11) 4 a. Detect chemical itself (direct) b. Detect metabolites (breakdown products) c. Detect secondary effects (alteration of body tissue/structure by drug) 3. Locations (Slide 11) a. Blood b. Breath c. Sweat d. Hair e. Urine IV. Abstinence monitoring substance examples A. Monitoring using breath (e.g. alcohol, tobacco) (Slide 13) 1. Advantages a. Easy to use; non-invasive (no blood draw) b. Cost predominantly device ($500-2,500) and reusable 2. Disadvantages a. Must be done properly b. Cheating (ex. non-deep breath for breath alcohol measurement) c. Possibly non-specific (ex. carbon monoxide produced from other burned substances) 3. Breath example 1: alcohol (Slide 14) 5 a. Alcohol is water soluble -> appears in the breath5; 6 b. Electrochemical detection (burns alcohol) c. Deep breath = proportional to blood level in deep lungs (alveoli) d. Detects [alcohol] as low as 1 drink last hour 4. Breath example 2: nicotine (Slide 15) a. Measures carbon monoxide (CO) from burning tobacco7; 8 b. Electrochemical detection (burns CO) - [CO] threshold w/ 90% sensitivity c. [CO] detected up to 2 days9, but sensitivity for “smokers” <10 hours10-12 B. Monitoring using urine (e.g., drugs) 1. Advantages (Slide 16) a. Easy to obtain/non-invasive – detection via specific antibodies (immunochemistry) b. Common: >120 million screens/yr13 c. Inexpensive: $4-8/test 2. Disadvantages (Slide 16) a. Positive test → expensive replication (~ $100+ 14, chromatograph13; 15) b. Replication takes weeks to get results c. Specific drugs detected for different time lengths d. Cheating 3. Urine example: urine drug screen (e.g. employment job screen) (Slide 17) 6 a. Specific antibody (Immunoassay) screening for substances or their byproducts b. Many substances can be detected in a single test 1’. Opioids 2’. Amphetamines 3’. Cocaine 4’. Cannabinoids 5’. PCP 6’. Alcohol 7’. Benzodiazepines 4. Specific drugs detected for different time lengths16 (Slide 18) a. Most opioids (heroin, morphine, methadone, etc.) 1-3 days b. Cannabinoids 1’. Single use – 3d 2’. Daily – 10-15d 3’. Long-term heavy - >30d c. Amphetamines – 2d d. Cocaine – 2-4d e. PCP – 8d f. Alcohol – 1/4 – 1/2 d (7-12h) 7 f. Sedatives (e.g. benzodiazepines) 1’. Short-acting – 3d 2’. Long-acting – 30d 5. Many ways to cheat; 2007 Review - 12 million “tampering” web sites and 40 methods13 (Slide 19) a. Adulterants 1’. Substances added to urine sample (OTC eye drops, ammonia) 2’. Suspect w/ abnormal urine chemistry (↓/↑ acidity, ↑ [nitrate]) b. Dilution 1’. Intentional fluid over-ingestion→ ↓[urine drug] 2’. Suspect w/ dilute urine (↓ [creatinine], ↓specific gravity) 3’. Acute water intoxication can be life threatening17 c. Substitution 1’. Use of another’s, old, or synthetic urine 2’. Suspect w/ abnormal urine properties (temperature, chemistry) d. False attribution – claimed use of one chemical to hide another16 1’. Amphetamines – phenylephrine (OTC decongestant) 2’. Opioids – poppy seeds, quinolones (antibiotic) 3’. Benzodiazepines – sertraline (anti-depressant) 4’. PCP – dextromethorphan (cough suppressant) 8 5’. Cannabinoids – proton pump inhibitors (OTC heartburn Rx) C. Monitoring using blood (Slide 20) 1. Advantages a. Highly specific confirm other tests b. Difficult to cheat, low false positives c. Direct and indirect measurements possible 2. Disadvantages a. Invasive – requires a blood draw b. Expensive – includes testing and procedural fees 3. Blood example 1: alcohol (Slide 21) a. Blood alcohol concentration18 1’. Direct detection of alcohol 2’. Timing: Recent consumption only b. Carbohydrate deficient transferrin (CDT)19; 20 1’. Indirect marker of alcohol use - ↑ alcohol > 2 wks ↑ CDT 2’. Timing: abstinence ↓ CDT in 2-5 weeks 4. Blood example 2: cannabis (Slide 22) a. Direct detection of cannabinoids b. Timing 9 1’. Acute use21;22 a’. ↑ [THC] to peak within minutes b’. ↓ [THC] < 1 hour, can be non-zero for 1 day 2’. Chronic use23 - Low [THC] up to 30 days D. Monitoring using sweat (Slide 23) 1. Advantages a. Non-invasive b. Tamper resistant c. Amenable to electronic and chemical detection techniques d. Many substances can be detected 2. Disadvantages a. Positive test → expensive replication b. Limited quantification (largely present or absent) c. Unclear effects of exercise (increased sweat production) 3. Chemical monitoring of sweat24 (Slide 24) a. Swab collection 1’. Used to verify intoxication 2’. Detects recent usage only (point in time, <24 hours) b. Patch collection 10 1’. Collect drug over longer periods of time (~1 week) 2’. Possible to provide cumulative measure 3’. Drugs may be reabsorbed 4. Electronic monitoring (Slide 25) a. Advantages 1’. Continuous monitoring 2’. Data can be monitored remotely b. Disadvantages 1’. Intrusive and highly visible - Use commonly limited to forensic setting 2’. Expensive – costs include unit plus monitoring or lease 3’. Optimized for forensics25; 26 a’’. High threshold for positive events (low/slow drinking can be missed) b’’. Limited ability to predict how many drinks c’’. Sensitive to external alcohol sources (ex. spills) 5. Sweat monitoring example: ScramX electronic alcohol monitoring27 (Slide 26) a. Similar to breath; Alcohol is water soluble → sweat5; 6 b. Samples every 30 minutes and data analyzed by company c. Automatic alerts d. Tamper resistant (detects temperature, requires special tool to remove) 11 d. Cost: $6-8/day lease; $1,400-1,800 + $5/day purchase E. Monitoring abstinence with other sources (Slide 27) 1. Hair28 a. Advantages 1’. Chemical detection 2’. Detects patterns of long-term usage 3’. Non-invasive 4’. Difficult to cheat b. Disadvantages 1’. Limited substances can be detected 2’. Cannot determine if a patient is acutely intoxicated (may be up to one month) 3’. Significant time lag until results 4’. Positive test → expensive replication 2. Saliva29; 30 a. Advantages 1’. Chemical detection 2’. Can be used to detect acute intoxication 3’. Non-invasive 4’. Difficult to cheat 12 5’. Highly sensitive b. Disadvantages 1’. Short window of detection 2’. Positive test → expensive replication 3. Hair monitoring details28 (Slide 28) a. Drug becomes deposited in follicles which results in presence in hair b. Hairs cut and sent for testing c. Several drugs can be detected 1’. Cocaine 2’. Amphetamines 3’. Opiates 4’. PCP 5’. THC/Cannabis 6’. Ecstacy 4. Saliva monitoring details30 (Slide 28) a. Drug travels in blood or was ingested via mouth → drug in saliva b. Saliva absorbed into a pad for testing c. Several drugs can be detected 1’. Cocaine 13 2’. Amphetamines 3’. Opiates 4’. PCP 5’. THC 6’. Sedatives V. Efficacy of monitored abstinence A. Methadone maintenance31-33 (Slide 30) 1. Goal and approach a. Goal: ↓ crime; ↑ able to work and ↑family time b. Methadone vs heroin 1’. Lasts >24hours → 1x/day dosing 2’. Allows work; avoids withdrawal and prevent “high” 3’. Cheaper & supplied by clinic → ↓need commit crimes c. Approach: highly structured, use methadone to substitute for riskier opiate (heroin) 1’. Administer methadone daily, usually at clinic 2’. Methadone ↓ withdrawal33 3’. Prevents euphoria/”high” from other opioids31 4‘. Monitor for abstinence from heroin/morphine and other drugs33 5’. Rx programs are federally regulated and include counselling32; 33 14 6’. Success → continue program 7’. Failure → lose privileges or access to methadone 2. Methadone clinic efficacy31 (Slide 31) a. 3x ↑remain in Rx vs no opiate replacement b. 2/3x ↓ positive opioid hair/urine samples w/ replacement c. 2.5x ↓ involved in crime B. Chronic pain management 1. Goal and approach (Slide 32) a. Goal: provide adequate pain control and minimize illicit opioid use34 b. Approach: adherence monitoring and risk minimization35 1’. Risk minimization a'. Explicit agreements regarding supply and behavior b’. Stratify risk for opioid misuse 1’’. Patient questionnaire – e.x. opioid risk tool36 2’’. Physician checklists evaluating patient behaviors37 a’’. Over-usage/early refills b’’. Multiple prescribers c’’. Over-focus on opioids d’’. Extra visits/phone calls 15 e’’. “Lost” or “stolen” medications c’. Preferentially prescribe abuse resistant medications 2’. Adherence monitoring a'. Verify opioid supply (prescription drug monitoring programs)35 b’. Routine urine drug testing (rapid point-of-care and verification)34; 35 3’. Success → continued access to prescription opioids 4’. Failure → lose access to prescription opioids & termination of treatment 2. Efficacy (Slide 33) a. Urine drug tests → ↓ illicit drug usage38; 39 b. ↑ urine drug tests → ↑prescription medication plan adherence40 1’. 2-6 urine drug tests → ↑prescription medication plan adherence 3.8 – 10.5% 2’. 12 urine drug tests →↑ prescription medication plan adherence 18.4% c. ↑ urine drug tests → non-prescribed medications (or ↑ abstinence)40 1’. 2-6 urine drug tests → ↑ abstinence non-prescribed medications 1.5 - 4.4% 2’. 12 urine drug tests →↑ abstinence non-prescribed medications 8.7% C. Court mandated Rx: drug courts offer SUD Rx vs jail 1. Goal and approach (Slide 34) a. Goal: stop substance abuse and related crime41 1’. Many federal/state crimes are SUD and drug related42 16 a’. ~50% federal/state prisoners w/ SUD b’. >25% intoxicated at time of offense 2’. SUD Rx → ↓ drug use → ↓ crime b. Approach: highly structured management41 1’. Receive authority from legal integration a’. Residential and outpatient Rx b’. Random urine drug screens c’. Routine judicial interaction and progress monitoring c. Success → avoid jail d. Failure → 1’. ↑monitoring frequency/intensity 2’. ↑punishment up to jail 2. Efficacy (Slide 35) a. Crime: 12% ↓ criminal relapse43 b. Substance use: no clear effect on SUD Rx outcomes44 1’. Difficult to quantify 2’. Highly heterogeneous population 3’. Different Rx approaches/referral networks D. Physician health programs (PHP) 17 1. Goal and approach (Slide 36) a. Goal: avoid patient harm through early detection and Rx b. Most common substances of abuse45 1’. Alcohol 2’. Opioids c. Approach: highly structured care management46; 47 1’. Receive authority from state medical licensing boards, laws, or job a’. Residential and outpatient Rx b’. Random urine drug screens c’. +/- random office visit d’. ≥5 yr follow-up 2’. Success → practice medicine, keep job 3’. Failure → a’. Return to Rx b’. ↑monitoring frequency/intensity c’. Referral to medical licensing board d. Soberlink Blue Device System48 (Slide 37) 2. Efficacy44; 42; 43 (Slide 38) a. Only ~20% w/ positive UDS at any time during 5 yrs 18 b. 70-80% physicians still licensed and employed at 5 yr follow-up VI. Summary (Slide 39) A. Like many other conditions, SUDs are chronic relapsing/remitting B. Abstinence monitoring is therapeutic C. Monitoring can be chemically and electronically D. Monitored abstinence improves Rx outcomes VIII. Graphic during Questions (Slide 40) 19 References 1. McLellan, A. T., Lewis, D. C., O'Brien, C. P., & Kleber, H. D. (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA, 284(13), 16891695. 2. American Psychiatric Association., & American Psychiatric Association. DSM-5 Task Force. (2013). Diagnostic and statistical manual of mental disorders : DSM-5 (5th ed., pp. p.490-497). Arlington, Va.: American Psychiatric Association. 3. Dawson, D. A., Goldstein, R. B., & Grant, B. F. (2007). Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcohol Clin Exp Res, 31(12), 2036-2045. doi: 10.1111/j.1530-0277.2007.00536.x 4. . Helping Patients Who Drink Too Much - A Clinician's Guide. (2007). (NIH Publication No. 07–3769). National Institute on Alcohol Abuse and Alcoholism. 5. Jones, A. W., Hahn, R. G., & Stalberg, H. P. (1992). Pharmacokinetics of ethanol in plasma and whole blood: estimation of total body water by the dilution principle. Eur J Clin Pharmacol, 42(4), 445448. 6. Norberg, A., Sandhagen, B., Bratteby, L. E., Gabrielsson, J., Jones, A. W., Fan, H., & Hahn, R. G. (2001). Do ethanol and deuterium oxide distribute into the same water space in healthy volunteers? Alcohol Clin Exp Res, 25(10), 1423-1430. 7. Deveci, S. E., Deveci, F., Acik, Y., & Ozan, A. T. (2004). The measurement of exhaled carbon monoxide in healthy smokers and non-smokers. Respir Med, 98(6), 551-556. 8. Jarvis, M. J., Tunstall-Pedoe, H., Feyerabend, C., Vesey, C., & Saloojee, Y. (1987). Comparison of tests used to distinguish smokers from nonsmokers. Am J Public Health, 77(11), 1435-1438. 9. www.bedfont.com.). piCO Smokerlyzer Operating Manual. Retrieved 1/18/2015, from http://www.bedfont.com/downloads/pico+/LAB220_piCO+_Manual_English_iss13.pdf 10. Maclaren, D. J., Conigrave, K. M., Robertson, J. A., Ivers, R. G., Eades, S., & Clough, A. R. (2010). Using breath carbon monoxide to validate self-reported tobacco smoking in remote Australian Indigenous communities. Popul Health Metr, 8(1), 2. doi: 10.1186/1478-7954-8-2 11. Sandberg, A., Skold, C. M., Grunewald, J., Eklund, A., & Wheelock, A. M. (2011). Assessing recent smoking status by measuring exhaled carbon monoxide levels. PLoS One, 6(12), e28864. doi: 10.1371/journal.pone.0028864 12. Cunnington, A. J., & Hormbrey, P. (2002). Breath analysis to detect recent exposure to carbon monoxide. Postgrad Med J, 78(918), 233-237. 13. Jaffee, W. B., Trucco, E., Levy, S., & Weiss, R. D. (2007). Is this urine really negative? A systematic review of tampering methods in urine drug screening and testing. J Subst Abuse Treat, 33(1), 3342. doi: 10.1016/j.jsat.2006.11.008 14. CostHelper, Inc.). Drug or Alcohol Testing Cost - How Much Does Drug or Alcohol Testing Cost? . Retrieved 1/18/2015, from http://health.costhelper.com/drug-alcohol-test.html 15. Standridge, J. B., Adams, S. M., & Zotos, A. P. (2010). Urine drug screening: a valuable office procedure. Am Fam Physician, 81(5), 635-640. 16. Moeller, K. E., Lee, K. C., & Kissack, J. C. (2008). Urine drug screening: practical guide for clinicians. Mayo Clin Proc, 83(1), 66-76. doi: 10.4065/83.1.66 17. Tilley, M. A., & Cotant, C. L. (2011). Acute water intoxication during military urine drug screening. Mil Med, 176(4), 451-453. 18. Martin, E., Moll, W., Schmid, P., & Dettli, L. (1984). The pharmacokinetics of alcohol in human breath, venous and arterial blood after oral ingestion. Eur J Clin Pharmacol, 26(5), 619-626. 19. Allen, J.P.; Sillanaukee, P.; Strid, N.; Litten, R.Z. (2003). Biomarkers of Heavy Drinking. In J. P. W. Allen, V.B. (Ed.), Assessing Alcohol Problems - A Guide for Clinicians and Researchers (Second 20 ed., Vol. NIH Publication No. 03–3745). Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism. 20. Ingall, G. B. (2012). Alcohol biomarkers. Clin Lab Med, 32(3), 391-406. doi: 10.1016/j.cll.2012.06.003 21. Schwope, D. M., Bosker, W. M., Ramaekers, J. G., Gorelick, D. A., & Huestis, M. A. (2012). Psychomotor performance, subjective and physiological effects and whole blood Delta(9)tetrahydrocannabinol concentrations in heavy, chronic cannabis smokers following acute smoked cannabis. J Anal Toxicol, 36(6), 405-412. doi: 10.1093/jat/bks044 22. Skopp, G., & Potsch, L. (2008). Cannabinoid concentrations in spot serum samples 24-48 hours after discontinuation of cannabis smoking. J Anal Toxicol, 32(2), 160-164. 23. Bergamaschi, M. M., Karschner, E. L., Goodwin, R. S., Scheidweiler, K. B., Hirvonen, J., Queiroz, R. H., & Huestis, M. A. (2013). Impact of prolonged cannabinoid excretion in chronic daily cannabis smokers' blood on per se drugged driving laws. Clin Chem, 59(3), 519-526. doi: 10.1373/clinchem.2012.195503 24. De Giovanni, N., & Fucci, N. (2013). The current status of sweat testing for drugs of abuse: a review. Curr Med Chem, 20(4), 545-561. 25. Hill-Kapturczak, N., Lake, S. L., Roache, J. D., Cates, S. E., Liang, Y., & Dougherty, D. M. (2014). Do variable rates of alcohol drinking alter the ability to use transdermal alcohol monitors to estimate peak breath alcohol and total number of drinks? Alcohol Clin Exp Res, 38(10), 25172522. doi: 10.1111/acer.12528 26. Hill-Kapturczak, N., Roache, J. D., Liang, Y., Karns, T. E., Cates, S. E., & Dougherty, D. M. (2014). Accounting for sex-related differences in the estimation of breath alcohol concentrations using transdermal alcohol monitoring. Psychopharmacology (Berl). doi: 10.1007/s00213-014-3644-9 27. SCRAM Continuous Alcohol Monitoring. (2014). Retrieved 12/2/14, 2014, from http://www.scramsystems.com/index/scram/continuous-alcohol-monitoring 28. Baciu, T., Borrull, F., Aguilar, C., & Calull, M. (2015). Recent trends in analytical methods and separation techniques for drugs of abuse in hair. Anal Chim Acta, 856, 1-26. doi: 10.1016/j.aca.2014.06.051 29. Gallardo, E., Barroso, M., & Queiroz, J. A. (2009). Current technologies and considerations for drug bioanalysis in oral fluid. Bioanalysis, 1(3), 637-667. doi: 10.4155/bio.09.23 30. Pil, K., & Verstraete, A. (2008). Current developments in drug testing in oral fluid. Ther Drug Monit, 30(2), 196-202. doi: 10.1097/FTD.0b013e318167d563 31. Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev(3), CD002209. doi: 10.1002/14651858.CD002209.pub2 32. Methadone Treatment Services. (2014). Retrieved 12/2/14, 2014, from http://www.methadone.us/blog/methadone-treatment-services/ 33. Strain, E. (2014). Treatment of opioid use disorder. Retrieved 12/2/14, 2014, from http://www.uptodate.com/contents/treatment-of-opioid-use-disorder 34. Christo, P. J., Manchikanti, L., Ruan, X., Bottros, M., Hansen, H., Solanki, D. R., . . . Colson, J. (2011). Urine drug testing in chronic pain. Pain Physician, 14(2), 123-143. 35. Solanki, D. R., Koyyalagunta, D., Shah, R. V., Silverman, S. M., & Manchikanti, L. (2011). Monitoring opioid adherence in chronic pain patients: assessment of risk of substance misuse. Pain Physician, 14(2), E119-131. 36. Webster, L. R., & Webster, R. M. (2005). Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med, 6(6), 432-442. doi: 10.1111/j.15264637.2005.00072.x 37. Chabal, C., Erjavec, M. K., Jacobson, L., Mariano, A., & Chaney, E. (1997). Prescription opiate abuse in chronic pain patients: clinical criteria, incidence, and predictors. Clin J Pain, 13(2), 150-155. 21 38. Manchikanti, L., Manchukonda, R., Pampati, V., Damron, K. S., Brandon, D. E., Cash, K. A., & McManus, C. D. (2006). Does random urine drug testing reduce illicit drug use in chronic pain patients receiving opioids? Pain Physician, 9(2), 123-129. 39. Pesce, A., West, C., Rosenthal, M., Mikel, C., West, R., Crews, B., . . . Horn, P. S. (2011). Illicit drug use in the pain patient population decreases with continued drug testing. Pain Physician, 14(2), 189193. 40. Laffer, A., Murphy, R., Winegarden, W., Pesce, A., Mikel, A., West, C., . . . Christie, J.M. (2011). An Economic Analysis of the Costs and Benefits Associated with Regular Urine Drug Testing for Chronic Pain Patients in the United States. 41. The National Association of Drug Court Professionals, Drug Court Standards Committee. (2004). Defining Drug Courts: The Key Components. Retrieved from http://www.unodc.org/documents/ungass2016/Contributions/Civil/Drug_Court_Professionals/ Key_Components.pdf. 42. Mumola, C.J. ; Karberg, J.C. (2007). Drug Use and Dependence, State and Federal Prisoners, 2004. Retrieved from http://www.bjs.gov/content/pub/pdf/dudsfp04.pdf. 43. Mitchell, Ojmarrh, Wilson, David B., Eggers, Amy, & MacKenzie, Doris L. (2012). Assessing the effectiveness of drug courts on recidivism: A meta-analytic review of traditional and nontraditional drug courts. Journal of Criminal Justice, 40(1), 60-71. doi: 10.1016/j.jcrimjus.2011.11.009 44. Klag, Stefanie, O'Callaghan, Frances, & Creed, Peter. (2005). The Use of Legal Coercion in the Treatment of Substance Abusers: An Overview and Critical Analysis of Thirty Years of Research. Substance Use & Misuse, 40(12), 1777-1795. doi: 10.1080/10826080500260891 45. Yellowlees, P. M., Campbell, M. D., Rose, J. S., Burke Parish, M., Ferrer, D., Scher, L. M., . . . DuPont, R. L. (2014). Psychiatrists With Substance Use Disorders: Positive Treatment Outcomes From Physician Health Programs. Psychiatr Serv. doi: 10.1176/appi.ps.201300472 46. DuPont, R. L., McLellan, A. T., Carr, G., Gendel, M., & Skipper, G. E. (2009). How are addicted physicians treated? A national survey of Physician Health Programs. J Subst Abuse Treat, 37(1), 1-7. doi: 10.1016/j.jsat.2009.03.010 47. DuPont, R. L., McLellan, A. T., White, W. L., Merlo, L. J., & Gold, M. S. (2009). Setting the standard for recovery: Physicians' Health Programs. J Subst Abuse Treat, 36(2), 159-171. doi: 10.1016/j.jsat.2008.01.004 48. Soberlink. (2015). Retrieved 9/27/2015, 2015, from http://www.soberlink.com/