Fever in Children
advertisement

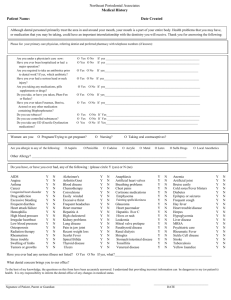
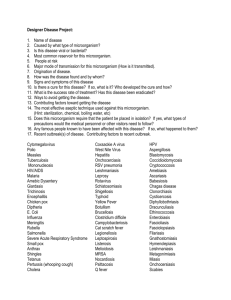
Fever in Children Axillary 1°C lower than core; tympanics unreliable; Height of fever irrelevant; may be hypothermic; concern if >38°C; those <3/12 with viral illness have significant incidence of UTI, so still need to do urine Appears ill 13-21% SBI Appears well <5% SBI Appears ill 13-21% SBI Appears well <5% SBI Neonates have 2x risk of SBI than 4-8/52 <1/12 <3/12 3-6/12 Pyrexia <1% SBI UTI in 3-8% T <38.9°C 1% bacteraemia UTI most common cause of fever without focus T >39°C 3% bacteraemia T > 40°C 10% bacteraemia WCC >15 + fever 10% bacteraemia 3-36/12 + febrile + appears well 0.5-0.7% sepsis 6/12 – 2yrs Any fever 10% SBI T >40°C 10% SBI SIRS Definitions Aetiology UTI most common cause T >38°C / <36°C + HR >160 (infants) / >150 (children) + RR >60 (infants) / >50 (children) + WCC >12 / >10% band forms Severe sepsis As above + hypotension (<65 infants, <75 children, <90 adolescent) Simple febrile convulsion 6/12 - 5yrs; T >38.5°C; generalised seizure; short post-ictal period; 1 seizure / fever; duration <15 minutes; no focal neurological deficit afterwards Neonate Gp B Strep (30%) > E coli (30-40%) > N meningitidis > Hib > Strep pneumoniae > Listeria Vertical transmission more likely; higher mortality; pneumonia common; other G-ive 1520% (eg. Klebsiella), G +ive 10%; enterococci, C trachomatis, herpes simplex; enterovirus, RSV, influenza A <3/12 N meningitidis > Hib > Strep pneumoniae > Gp B Strep > E coli > Listeria In pneumonia: Chlamydia trachomatis (develops in 3-16% exposed, conjunctivitis in 50%) > RSV > other viruses > Bordatella pertussis <1yr In pneumonia: RSV > other viruses > strep pneumoniae > Hib > C trachomatis > mycoplasma pneumoniae <5yrs N meningitidis > Strep pneumoniae > Hib In pneumonia: viruses > S pneumonaie > Hib > M pneumoniae > C pneumoniae (also S aureus, B pertussis) >5yrs N meningitidis > Strep pneumoniae In pneumonia: M pneumoniae > S pneumonaie > C pneumoniae > Hib/a > adenovirus > other viruses (also S aureus, Legionella) Aetiology (cntd) Immunocompromised, neurosurgery, trauma: Staph, gram negativess, cryptococcus neoformans Developing countries: mycoplasma TB Brain abscess: strep viridans, anaerobes, G negatives, staph aureus Viral: enterovirus, HSV, VZV, CMV, EBV Chronic lung disease (pneumonia): Cystic fibrosis: S aureus, pseudomonas Sickle cell anaemia: encapsulated Immunocompromised: pneumocystis, aspergillis, histoplasma (nodular on CXR), CMV, fungi Febrile Convulsions Epidemiology: in 3-5% children; 30-40% recurrent especially if <1yr; ; 3% go on to suffer epilepsy; have no effect on CSF WCC LP in first febrile convulsion: if you think it’s meningitis, treat and do LP when improve Pros: mental state difficult to assess post-ictally; fulminant infections require early diagnosis; quick Cons: <5% have meningitis; traumatic to child / family; may cause meningeal seeding if bacteraemia; coning Management: seek cause of fever; seek concurrent antibiotics; investigate as per usual fever; consider need for cancer / glucose / pyridoxine Remember: weight = (age + 4) x 2 or >10yrs = age x 3 1. Diazepam 0.25mg/kg IV / 0.5mg/kg PR or Midazolam 0.15mg/kg IV / IM / buccal 2. Repeat after 5mins 3. Phenytoin 18mg/kg over 30mins (will be slow at controlling seizures) Or Phenobarbitone 18mg/kg over 30mins 4. Thiopental 5mg/kg IV + RSI If no IV access: paraldehyde 0.3mg/kg PR (good if mentally handicapped / recurrent seizures) Prognosis: risk of febrile convulsion recurrence if: repetitive seizures, focal features, onset <1yr, brief duration between fever onset and seizure; FH Differential diagnosis: Infantile spasm: sudden brief flexion of arms, head and trunk, occurring in clusters Breath-holding spells: noxious stimulus; after brief cry / vigorous crying Benign neonatal sleep myoclonus / Benign focal epilepsy of childhood / Nocturnal frontal lobe seizures / Night terrors Urinary Tract Infections Epidemiology: incidence 5% in children aged 3-24/12 with fever; affects 1% boys, 3% girls before puberty; females:males 3:1 (except in neonates); circumcised:uncircumcised 10:1; most common SBI; present in 3-8% young children presenting with fever and no obvious source; 5-10% with symptomatic UTI will develop renal scarring ( HTN, CRF, eclampsia) and bacteraemia; systemic sepsis in 30% 13/12, 5% >3/12; 2% children have asymptomatic bacteruria which is not cause for presentation; pyelonephritis suggested if T >39°C and +ive urine; 10% young infants with UTI have sterile WCC in CSF Pathophysiology: haematogenous seeding in neonates; ascending otherwise; cystitis can cause vesicoureteric reflux Bacteria: 84% E coli, 6% proteus, 5% klebsiella, 3.5% enterococcus; G+ives in older boys and children with underlying medical conditions Investigation: Urine: always send for culture if suspect UTI; always send for microscopy regardless of result of dipstick (unless low risk and negative dipstick); do repeat urine at 10/7 to ensure clearance Nitrites: 40% sensitivity (doesn’t develop with G+ives) 95-99% specificity WBC dipstick: 70-80% sensitivity 80-90% specificity Gram stain 80-97% sensitivity; sensitivity if <2yrs WBC: 50-90% sensitivity 50-90% specificity Bacteria: 50-90% sensitivity 10-90% specificity Microscopy – 15% false negative rate; significant number missed; may get moderate leucocytess in 40% febrile children without UTI MSSU: good sensitivity, positive if WCC >5-10 Bag spec: unreliable; if negative still needs to be sent for culture; can be used if pre-test probability low Catheter spec: positive if WCC >1-5 SPA: positive if WCC >0; must have at least 15ml on USS, go 1cm superior to pubic symphysis with 23G needle; 50% success rate blind, 95% with USS guidance) Blood: do blood culture if positive urine and <1yr, or ill enough to require admission LP: consider if <1/12 Renal USS: do in all children with 1st UTI, 3-6/52 after infection; also do if sibling of child with VUR; abnormalities found in 40%; obstructive lesions found more commonly in young (<3/12) Urinary Tract Infections (cntd) Meningitis DMSA scan: do after 6/12 or at age 3-4yrs to look for scarring if required hospitalisation MCU: do if <3/12 or if abnormal USS Admit if: <6/12, septic, significant underlying disease, urinary obstruction, pyelonephritis, failure to respond to PO’s Prophylaxis: give if recurrent UTI’s, <3/12 awaiting MCU, known VUR or other renal abnormality; continue until after USS; give 2mg/kg co-trimoxazole or 3mg/kg nitrofurantoin nocte or 5-10mg/kg cefaclor nocte Epidemiology: 90% occur <5yrs; 5% mortality; 10-20% intellectual / auditory complications; asymptomatic N meningitidis nasal carriage in 10%; meningococcal sepsis bimodal (0-4yrs, 15-25yrs); <3/12 + febrile = 1% incidence Pathophysiology: usually haematogenous spread from URTI; can also be direct (eg. Otitis media), injury Risk factors: young, male, low SEG, congenital abnormalities, shunt, trauma, immunocompromised Assessment: may be afebrile / hypothermic; bulging fontanelle is late finding and masked by dehydration; signs of meningeal irritation may be absent <18/12; focal neurological deficit in 15% (30% pneumococcus); seizures in 30% (with worse than expected mental status after); 15-20% LOC (more in pneumococcus); subdural effusion / empyema (30% in Hib, 20% in strep); may deteriorate after antibiotics (bacteriolysis inflammation); beware partially treated meningitis (more frequent vomiting, longer duration of symptoms); suspect encephalitis if seizures / altered LOC / behaviour; early purpura may just be erytematous macules LP: consider pre-oxygenation before LP; use non-styleted needle in small infants; neck in mid-flexion CSF interpretation: CSF protein 0.01g for every 1000 RBC; lymphocytes >50% in 10% bacterial meningitis; Gram stain 80% sensitivity (50% if pre-treated); may mistake G+ive for G-ive if pre-treated; nearly 100% mononuclear when viral (may be more PMN’s if <48hrs; monocytes are most common WBC in viral); visible budding MO’s on Indian ink staining = cryptococcal; CSF antigen tests have high sensitivity and specificity (especially for Hib and N meningititis) CT before LP if: FND, LOC Contraindications to LP: signs of ICP, coma, FND, focal seizures, seizures >30 minutes, haemodynamically unstable, significant respiratory compromise, purpura, coagulopathy, platelets, localised skin infection Other Investigations: bloods; meningococcal PCR; antigen studies on blood and urine; throat swab for N meningitidis Management: if shocked, 10-20ml/kg N saline; SIADH in 30% so use 50% maintenance after resus; treat seizure, fever, hypoglycaemia, hyponatraemia (fluid restriction if Na <135), intracranial pressure Antibiotics: give antibiotics before LP if there will be >20min delay to LP Dexamethasone: 0.25mg/kg (max 10mg) IV/IM Q6h for 48hrs; use if >1/12 to host response to bacteria and deafness; give at least 15-30mins before (or within 1hr of antibiotics); best in Hib Contact prophylaxis: meningococcus / Hib – give rifampicin 10mg/kg BD x4 (contraindicateded in pregnancy and liver disease; ceftriaxone IM or ciprofloxacin PO if contraindicated); contact = family and household contacts, those exposed to oral secretions, sexual partners, health care workers, staff and children at pre-school in last 10/7 Normal neonate Normal child Bacterial Partially treated Viral Encephalitis TB Opening pressure 5 8.5 WCC <30 <5-10 200-5000 200-5000 100-700 <500 100-500 % PMN’s <2 0 PMN (neutrophils) <5 0 >100-10,000 >10-100 <100 <100 early MMN (lymphocytes) <20 <5 <100 >100 late Protein <0.3 <0.4 Normal/ 0.4-1 Glucose >2.5 >2.5 Normal/ Normal late Glucose % in serum 50 >40 RBC <2 <2 + +/- Gram stain Pneumonia Epidemiology: up to 40% are mixed; viral more common than bacterial; strep pneumoniae most common bacterial cause (especially <5yrs); mycoplasma up to 30% History: if neonate, ask about mother’s pre- and perinatal health including infections and fever, premature rupture of membranes, peripartum complications, meconium; wheeze in young infant = bronchiolitis, in child = mycoplasma Atypical pneumonias (eg. Mycoplasma, C pneumoniae) non-specific appearance Staph rapidly progressive symptoms high fever, toxic, abscesses, cavitations, pleural effusions C trachomatis staccato cough, diffuse rales, no fever, sore throat Mycoplasma hacking dry cough, arthralgia, rash (in 10%), indolent course, Kawasaki syndrome, erythema multiforme, Guillian Barre syndrome B pertussis paroxysmal coughing, gasping, colour change, URTI Pneumococcal round pneumonia (should have FU to ensure resolution) If severely unwell: ?staph aureus, grp B strep If underlying lung disease: ?Hib Apnoeas: more common in RSV, chlamydia, B pertussis Effusions: strep pneumoniae most common cause; also mycoplasma, Hib Empyema, pneumatocoele, cavitation: staph aureus Examination: toxic appearance has better sensitivity than other parts of exam; SaO2 <90% on air risk of treatment failure with PO amoxicillin; fever + RR / BS / fine crackles predicts XR positive pneumonia with 93-96% sensitivity; fever + all 3 = 98% sensitivity; absence of RR, respiratory distress, rales and BS excludes pneumonia in 100%; SOB is best sign to rule out Bloods: blood culture +ive in <5%; NPA helpful to identify virus in younger, mycoplasma in older; mycoplasma cold agglutinins 72-92% sensitivity CXR: cons: may be false –ive / +ive; may be poor quality image; cost; delay; exposure to radiation; can’t distinguish between bacterial and viral Indications for CXR: toxic appearance with respiratory findings; <3/12 as part of septic screen; <5yrs with T >39°C, WCC >20 and no source; ambiguous clinical findings; ?complication; not responding to antibiotics; ?congenital lung malformation; follow up of round pneumonia; specific exam findings suggesting pneumonia Admission criteria: <6-12/12, toxic, altered LOC, complicated pneumonia, hypoxia, unrelieved respiratory distress; inability to feed; co-morbidities, dehydration, not tolerating PO antibiotics, social issues Assessment of the Febrile Child If find source, still do extensive search especially if <3/12; after fever reduction, no difference between appearance of bacteraemic and non-bacteraemic child (fever reduction may mask signs of severe infection); ask about birth history, peri- or neonatal complications; all criteria missed SBI in those <1/12 Rochester Criteria: if <60d and well looking, no peri-partum or prior illness, normal FBC, urine and CXR– SBI excluded; will miss 1% SBI; least sensitive of the 3 Philadelphia Protocol: if 29-56d and well looking, no immunodeficiency, normal RBC, urine, CXR and CSF; sensitivity 98%, specificity 44% Boston Criteria: if 28-89d and well looking, no recent immunisations / antibiotics, WBC <20, normal urine, CXR and CSF; >99% sensitivity <1/12 <3/12 Investigation of the Febrile Child >3/12 Appears well FBC, blood culture, urine, CSF, CXR; stool if diarrhea; admit and give antibiotics Appears well As above; but can discharge if WCC <15, urine –ive, CSF WBC <10 and normal CXR; admit otherwise ?bronchiolitis Still need to do urine ?viral Still need to do urine and bloods Appears well Urine; discharge if negative Appears unwell, any age Admit and treat Septic screen: do if: 3/12 or under Concurrent antibiotic use and fever without focus Toxic appearance Bloods: WCC, ANC, CRP, procalcitonin improve prediction of SBI; CRP 75% sensitivity and specificity for SBI Management of the Febrile Child Fever reduction: Pros: metabolic demands; improved neurological assessment; symptomatic relief Cons: doesn’t febrile convulsions, fever WBC motility and Fe, fever beneficial to immune response, ability to assess children with SBI Admit for antibiotics if: <1/12 (regardless of septic screen result); <3/12 with WCC >15 or any abnormal result on septic screen Sepsis: 10-20ml/kg IV saline bolus until perfusion improves (stop if rales or hepatomegaly develops); if shock not reversed, begin inotrope (use dopamine if “cold shock”, noradrenaline if “warm shock”); give hydrocortisone if resistant to inotropes Fever without Focus <3/12 Amoxicillin 50mg/kg QID (TDS if <1/52) (or ampicillin 50mg/kg QID) (to cover Listeria + Gp B strep) + Cefotaxime 100mg/kg loading dose 50mg/kg QID (BD if <1/52) (to cover G-ive) or Gentamicin 7mg/kg OD and consider aciclovir >3/12 Cefotaxime 100mg/kg loading dose 50mg/kg QID Urinary Tract Infection <3/12 CNS not excluded Amoxicillin 50mg/kg QID (TDS if <1/52) + Cefotaxime 100mg/kg loading dose 50mg/kg QID (BD if <1/52) <3/12 CNS excluded Amoxicillin 50mg/kg QID (TDS if <1/52) (use ceftriaxone 25mg/kg BD if penicillin allergy) Gentamicin 7.5mg/kg OD (max 240-360mg) IV (Not as good at CNS penetration as cef) Gentamicin 7.5mg/kg OD (max 240-360mg) IV or Cefuroxime 25-30mg/kg/dose IV >3/12 Antibiotic Choice in Paediatrics + Well Child If 6-24/12, give 1x IV/IM dose ceftriaxone 50mg/kg, then discharge on PO for 10/7 (<2yr) or 7/7 (older child) Augmentin 10mg/kg TDS PO Or Cotrimoxazole 4mg/kg BD PO Or Cephalexin 10mg/kg TDS PO Meningitis <1/12 Amoxicillin 50mg/kg QID (TDS if <1/52) + Cefotaxime 50mg/kg QID (BD if <1/52) or Gentamicin 2.5mg/kg TDS (BD if <1/52) <3/12 Amoxicillin 50mg/kg QID + Cefotaxime 100mg/kg loading dose 50mg/kg QID >3/12 Cefotaxime 100mg/kg loading dose 50mg/kg QID Or Ceftriaxone IM 100mg/kg loading dose 80-100mg/kg OD if no IV access Once sensitivities available: if Hib – amoxicillin; if pneumococcus / meningococcus – penicillin G, vancomycin Meningococcal Sepsis <1/12 Amoxicillin 50mg/kg QID (TDS if <1/52) + Cefotaxime 50mg/kg QID (BD if <1/52) ?+ Gentamicin 7.5mg/kg OD (5mg/kg if <1/52) <3/12 Amoxicillin 75mg/kg QID + Cefotaxime 100mg/kg loading dose 50mg/kg QID >3/12 Cefotaxime 100mg/kg loading dose 50mg/kg QID Or Ceftriaxone 50mg/kg BD Or Ceftriaxone IM 100mg/kg loading dose 80-100mg/kg OD if no IV access Brain Abscess: fluclox 50mg/kg IV Q4hrly + cefotaxime 50mg/kg QID + metronidazole 7.5mg/kg TDS HSV encephalitis: aciclovir <3/12 = 20mg/kg TDS <12yrs = 500mg/m2 TDS >12yrs = 10mg/kg TDS Pneumonia <3/12 Antibiotic Choice in Paediatrics (cntd) >3/12 >3/12, complicated >3/12, unwell ++ If well Mycoplasma Staph Discharge Criteria Amoxicillin 50mg/kg QID (TDS if <1/52) (or ampicillin 50mg/kg QID) + Cefotaxime 100mg/kg loading dose 50mg/kg QID (BD if <1/52) (or gentamicin) Amoxicillin 30-50mg/kg TDS Or + Augmentin 30mg/kg TDS-QID (ie. ?staph, lung abscess, pleural effusion) Cefuroxime 30mg/kg TDS Erythromycin / clarithromycin if severe (for atypicals, mycoplasma) + Flucloxacillin 50mg/kg QID IV (to cover staph) Cefotaxime 50mg/kg QID IV Amoxicillin 30mg/kg TDS PO for 5-7/7 Erythromycin 12.5mg/kg QID PO for 7-10/7 or Roxithromycin 4mg/kg BD PO Flucloxacillin 50mg/kg QID IV +/- Clindamycin 10mg/kg TDS-QID IV (if not improving on amoxicillin) (unwell, post-viral, abscesses) In fever: Term baby; no co-morbidities; no antibiotics during illness; WCC 5-15; other investigations normal; responsible carer; high probability of follow up In febrile convulsion: simple seizure, now normal neurological exam, source of fever determined, sensible parents with action plan, able to access help; consider seizure prophylaxis if prolonged recurrent seizures