Gilbert.Osmoregulation
advertisement

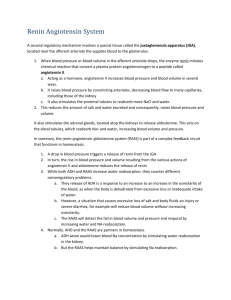
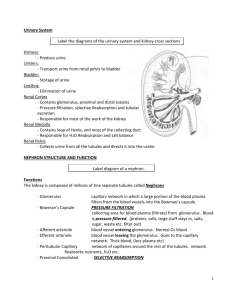
Osmoregulation. Gilbert. Fluid & Electrolytes. Katelyn Rogers. 12.01.09. Questions: With respect to renal hormone systems, what does RAS stand for? 1. Really active steroids 2. Rat sarcome 3. Renin angiotensin system 4. Rennin aspartate system Answers: 3, 3, 4, & 4. Summary of Body Fluids A patient w/ renal failure devps symptoms caused by the loss of a hormone produced by the kidney. Which is the most likely diagnosis? 1. Edema 2. HTN 3. Anemia 4. Uremia 5. Acidosis The following factor(s) tend(s) to INC the rate of GFR: 1, Sympathetic stimulation (NE) of the afferent arteriole 2. Obstruction of the renal tubules, ureter, or urethra 3. Vasodilation of the efferent arterioles 4. none are correct 5. all are correct A 55 yo woman w/ RA who is taking penicillamine & ibuprofin is diagnosed w/ the nephritic syndrome after a workup for lower extremity edema reveals large amounts of protein in her urine. Although the forces promoting filtration across the glomerulus are altered in this patient, which of the following Starling forces is normally the controlling factor favoring filtration? 1. Glomerular capillary oncotic pressure 2. Bowman’s space hydrostatic pressure 3. Oncotic pressure in Bowman’s space 4. Glomerular capillary hydrostatic pressure 5. Brownian motion The reason NaCl is in the ECS is because Na & H2O pairing are impt for the regulation of osmolarity. Total Body Water In the average 70 kg adult human: -~60% (42L) of BW is water -% of BW as water declines with: -age -incs in body fat % -gender/sex (I believe F is decd) Quantifying Urine Concentration Dilution The process of concentg or diluting the urine reqs the kidnesy to excrete water & solutes somewhat independently. Dilute urine = water excrtn in excess of solutes. (ie. More water) Conctd urine = solute excrtn in excess of water. (ie. More solute) This can be calculated as: In healthy indvl: intake always = output even in exercise. Concentration & Dilution of the Urine -Maximal urine conc = 1200 -1400 mOsm/L (specific gravity ~ 1.030) -Minimal urin concentration = 50-70 mOsm/L (specific gravity ~1.003) Even in dx states (not kidney), the Na excretion = intake. Obligatory Urine Volume The minimum urine volume in which the excreted solute can be dissolved & excreted. Example: If the max urine osmolarity is 1200mOsm/L, & 600 mOsm of solute must be excreted each day to maintain electrolyte balance, the obligatory urine volume is: (600mOsm/day)/(1200mOsm/L) = 0.5 L/day Way to tell if pt is dehydrated or vol loaded. Water diuresis in a human after ingestion of 1L of water Why was hyponatremia the most common medical condition at Grandma’s marathon last year despite the high Ts? Under normal conds, when you drink 1L of H2O the urine osmolarity decs, but the plasma osmolarity does not change much. The urine solute excretion is maintained even though the urine flow rate is greatly increased. At Grandma’s marathon, runners stop at each stand and get something to drink & many aren’t sweating enough to lose all that water. Remember exercise stimulates ADH, which retains water decreasing the urine outflow rate. So, the retention of water & incd ingestion of water leads to hyponatremia. Do not start an IV after a marathon, runner may be volume overloaded rather volume under loaded like one would assume. Factors that Dec ADH Secretion: -Decd osmolarity -Incd bld vol (cardiopulm reflexes) -Incd BP (arterial baroreceps) -Other factors: -alcohol -clonidine (antihypertensive drug) -haloperidol (antipsychotic, tics, Tourette’s) AVP= Arginine vasopressin Incd ECosmADH releaseinc H20 reabsorpthirst Osmoreceptor-antidiuretic hormone (ADH) feedback mechanism for regulating ECF osmolarity (post-pit = neurohypophysis) ADH synthesis in the magnocellular (neurons of hypothalamus), release by the post pituitary, & action on the kidneys (esp collecting duct) Vol depletion triggers AVP release Incd percent change with incd plasma ADH. Seen in both isotonic volume depletion and isovolemic osmotic inc. Note: isotonic volume depletion changes more with a given increase in plasma ADH than does isovolemic osmotic increase. Isovolemic osmotic increase will change less for a given plasma ADH. Stimuli for Thirst -Incd osmolarity -Decd bld vol (cardiopulm reflexes) -Decd BP (arterial baroreceps) -Incd angiotensin II -Other stimuli: dryness of mouth (Basically the same as what stimulates vasopressive release.) When the thirst feedback syst (ADH) is blocked, large changes in sodium intake leads to large inc in plasma Na; regulation is not intact! Sodium conc is maintained relatively constant over wide range of Na intakes, with or without Ang II-aldosterone feedback control. AVP-Mechanisms of Action Peripheral: -V1 recs in vasculature vasoconstriction -V2 recs in kidney stimulate generation & translocation of aquaporins Central: -V1 recsthirst, aggression?, memory? Factors that Dec Thirst -Decd Osmolarity -Incd Bld Vol (cardiopulmon reflexes) -Incd BP (arterial baroreceps) -Decd angiotensin II -Other stimuli: gastric distention LOOK AT PARALLELS BTWN THIRST & ADH. Disorders of Urine Concentrating Ability -Failure to produce ADH “Central” diabetes insipidus -Failure to respond to ADH: “nephrogenic” diabetes insipidus -impaired loop NaCl reabs (loop diuretics) -drug induced renal damage: lithium, analgesics -malnutrition (decd urea conc) -kidney disease: pyelonephritis, hydronephrosis, chronic renal failure. This is also why babies, puppies, & kittens pee so much, as get older devp recs to respond to nonconcentrated urine. Normally impermeable to H20. But when Aquaporin are present in vesicles ADH binds to V2stim cAMPAquaporins in walls of cell to allow passage of water from tubular into peritubular caps, vasa recta & ISF (REABSORPTION). Aquaporins also affect txn & tsln. Concentration & Dilution of Urine (understand this image!): PCT= Proximal Convoluted Tubule DCT= Distal CT For the kidney to fxn properly there must be a conc gradient: Low osm near cortex (outside) and high osm at medulla (inside) & it gradually incs from cortex to medulla. In this image, urine in tubule flows LR. Peritubular bld flows slowly RL. Flow must be maintained in both to fxn. This is done by controlling the expression of proteins along the tubule, regulating the permeability of solutes & water. Only 1-2% of RBF flws through the vasa recta. If BF incs washout of solutesdecg the grad. In desc limb, both solutes & water move passively in and out, matching the gradient in the bvs, not tubule. (All pumping is in the tubule, not the vessel) In the asc limb, solutes (esp Na) are pumped out, into ISF but NOT water. The concentration or dilution of urine really occurs in the collecting duct. Desert animals have long loops, while beavers have shorter loops. Animals awaking from hibernation or humans, who have just received a kidney transplant, will have this system working within an hour. This is crazy after there was no conc gradient! Gilbert likes that the permeabilities are labeled all the way through for both H2O & solutes. Know the consequences of the absence of a conc gradient. Changes in osmolarity of the tubular fluid as it passes through the different tubular segments in the presence of high levels of antidiuretic hormone (ADH) and in the absence of ADH. In collecting tubules & ducts the affect of ADH is very impt and this is the only part that is very perm to H2O. Gilbert’s Review Questions: Q1. Know the value (+ or -) of the clearance of H2O given difft Uf, UOsm, & POsm values. Q2. After surgery BP remains similar compared to pre-surgical BP. If kidney was taken from a HTNive patient, than person would become HTNive. Q3. Know that the endo R-A-Aldo syst includes angiotensinogen production by the liver, renin secretion by the juxtaglom apparatus & ACE present at the luminal surface of endo cells. The following is not true: Aldo, but not ALL, stimulate thirst & salt appetite (rather stims Na reabsortpion- activated by salt depletion) The following is not true: Ang II induces marked incs in Na reabsroption by the loop of Henle and the collecting duct (Ang II stimulates aldo secretion also not at loop of Henle) Q4. Severe renal artery stenosis, all of the following would be expected to be incd above normal except: a. b. c. d. e. plasma renin conc plasma ang II conc Hyd P in glom caps R to BF in eff arterioles Systemic arterial P Formation of a Dilute Urine: LOW AVP (LOTS OF URINE): -Cont electrolyte reabsorption in order to maintain the conc gradient. -Dec water reabsorption -Mechanism: Decd ADH release & reduced water permeability in distal & collecting tubules. Formation of a Dilute Urine: Size Matters -Nephron heterogeneity (not all nephrons have the same abilities to conc bc of difft lengths) Eg. Cortical, medullary, & juxtamedullary nephrons. Fish don’t even have a loop of Henle, they don’t conc urine bc they don’t need too w/ so much water. -Difft responsiveness to AVP – Babies, kittens, & puppies do not have a fully developed response system to AVP. The recs are not expressed as much and the response (incd cAMP) is not as great. Formation of a Concentrated Urine -Cont electrolyte reabsorption -Inc water reabsorption Mechanism -Increased ADH release which incs water permeability in distal & collecting tubules. -High osmolarity of renal medulla -Countercurrent flow of tubular fluid Formation of a Concentrated Urine when ADH Levels are High H2O goes into the ISF & is then carried away by the vasa recta. Formation of a Concentrated Urine: Size Matters Again! -Desert adapted animals: spiny mouse, etc have long tubules. Never are there adaptations in girth. The most impt length is in the loop of Henle. Reminder of process. Factors that Contribute to Buildup of Solute in Renal Medulla – Countercurrent Multiplier -Active transport of Na+, Cl-, K+ & other ions from thick ascending loop of Henle into medullary interstitium. -Active transport of ions from medullary collecting ducts into interstitium. -Passive diffusion of urea from medullary collecting ducts into insterstitium. -Diffusion of only small amounts of water into medullary interstitium. Net Effects of Countercurrent Multiplier -More solute than water is added to the renal medulla. Ie. Solutes are “trapped” in the renal medulla. -Fluid in the ascending loop is diluted. -Most of the water reabsorption occurs in the cortex (ie. In the proximal tubule & in the distal convoluted tubule) rather than in the medulla. -Horizontal gradient of solute conc establish by active pumping of NaCl is “multiplied” by countercurrent flow of fluid. The Vasa Recta Preserve Hyperosmolarity of Renal Medulla -The vasa recta serve as countercurrent exchangers. -Vasa recta blood flow is (only 1-2% of total RBF). -Again if BF incs, some of solutes may be washed out. -Passive diffusion easily occurs in both directions. Urea Recirculation (probably NOT on exam, but on BOARDS) -Urea is passively reabsorbed in proximal tubule (~50% of filtered load is reabsorbed) – this is impt to the regeneration of the conc gradient. -In the presence of ADH, water is reabsorbed in distal & collecting tubules, concentrating urea in these parts of the nephron. -The inner medullary collecting tubule is highly permeable to urea, which diffuses into the medullary interstitium. -ADH incs urea permeability of medullary collecting tubule. Recirculation of urea absorbed from medullary collecting duct into interstitial fluid Questions: 1. 2. 3. 4. 5. 6. 7. T/F. Decreased extracellular osmolarity (NaCl) stimulates ADH release, which incs H2O reabsorption, & inhibits thirst. Match the following as either stimuli for ADH secretion or factors that decrease ADH secretion: a. Increased osmolarity b. Increased blood volume c. Decreased BP d. Alcohol e. Clonidine f. Fear g. Angiotensin II h. Haloperidol i. Nausea j. Nicotine k. Morphine Where does ADH synthesis occur? Where does ADH act? Does increased ang II stimulate or decrease thirst? T/F. Decreased ADH release & increased water permeability in distal & collecting tubules forms a concentrated urine. T/F. Size matters in formation of both dilute and concentrated urine. Answers: 1. F. Increased extracellular osmolarity (NaCl) stimulates ADH release, which increases H2O reabsorption, & stimulates thirst (intake of water). 2. Stimuli for ADH secretion Factors that decrease ADH secretion a. Increased osmolarity b. Increased blood volume c. Decreased blood pressure d. alcohol f. Fear e. Clonidine g. Angiotensin II h. Haloperidol i. Nausea j. Nicotine k. Morphine 3. Magnocellular (neurons of hypothalamus). 4. Collecting duct 5. Stimulate 6. F. Decreased ADH release & reduced water permeability in distal & collecting tubules forms a dilute urine. 7. T.