Liver PBL Patient Chart: Gloria Stone 1/21/1970 PMH: HTN
advertisement

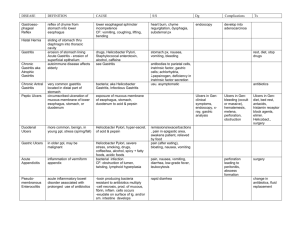
Liver PBL Patient Chart: Gloria Stone 1/21/1970 PMH: HTN, Hyperlipidemia Meds: HCTZ 25 mg daily, Acetaminophen 650mg every 4-6 hours as needed, Garlic 200mg TID Allergies: NKDA FH: Dad: Deceased age 70 from MI, HTN, Hyperlipidemia Mom: 74 yrs., alive, breast cancer at age 45 Sister: 45 yrs., alive, ETOH abuse SH: Works at daycare center, separated from spouse, 2 children, 1 year college completed, No routine physical activity, Drinks 20 oz. of soda daily, 2 glasses of ETOH daily, Smokes ½ PPD, Previous experimentation with marijuana and meth. Past Clinic Visit Information: 03/11: BP 160/90 HR 80 Re-establish care. Dx: HTN, Hyperlipidemia, On Garlic currently and restarted on HCTZ 11/08: BP 150/86 HR 70. New patient- establish care On Garlic currently and HCTZ started, treat Lipid panel with diet and activity Past Diagnostics: 03/11: Fasting glucose 122, Na 139 K+4.3 Chloride 102 Co2 27.5 BUN 13 Creatinine 0.9 AST 150 ALT 60, Hgb 12 Hct 37 MCV 105 Total Cholesterol 230 HDL 40 LDL 160 Triglyceride 150 11/08: Fasting glucose 120, Na 138 K+3.8 Chloride 102 Co2 28.5 BUN 16 Creatinine 1.1 AST 90, ALT 40, Hgb 12 Hct 37 MCV 100 Total Cholesterol 227 HDL 49 LDL 150 Triglyceride 140 Liver/Hepatitis PBL Assignment: References: 2 journal articles and 2 textbooks within the last five years (2pts) 1. Prior to class, students should review the Hepatitis and Liver Function Test Powerpoints as well as recommended readings for this topic. Students should also review the various causes of elevation of hepatic enzymes in detail using current journal articles pertinent to this topic. 2. A “patient chart” will be posted in the Liver/Hepatitis content section in the course prior to the session. 3. One student will be selected to be the designated spokesperson for the class. Students in class and online will interview the patient. The session will be recorded; therefore if a student is not able to be present in class or online, they are responsible for listening to the recorded session. 4. After class is complete, as a group, students will have an on-line discussion in the discussion section under Liver PBL. Students need to discuss the mostly likely three differentials with rationale and references, with the mostly likely listed as number one. All students should submit their answers and a consensus will need to be decided. Include also the diagnostics, with rationale, that should be done at this visit. The results of the diagnostics requested by the spokesperson will be posted in the Liver/Hepatitis content section within 24 hours of the diagnostic request. (2.5points) 5. After you have received the diagnostic results, individually, select your final diagnosis for today’s visit. Explain the rationale, references and the pathophysiology of the diagnosis. (2.5 points) Write your plan in detail. This should be written as if you are the NP writing the prescriptions and talking with the patient—everything that you would actually discuss in the office visit. Points will be deducted if this is not clear to the patient. (9 points) 6. In your plan, address any other medical issues that are pertinent to this patient and changes in the medical plan, if any, which should be considered at today’s visit or at future visits. Please be specific. (9 points) Please save the final document as a word file. Save with your last name and case name (i.e. SmithRenalPBL). The document must use 12 point font. No more than 5 pages with the reference page as an additional page. Be sure your name is on each page of the document. Liver PBL Rubric Section Diagnostics with differentials and rationales (group work) (2.5 pts.) Final Diagnosis for today’s visit with rationale and pathophysiology (individual work) (2.5 pts.) Detailed plan including pharmacological and non- Points Obtained/Points Earned Comments pharmacological interventions, including patient education (individual work) (9 pts.) Additional medical issues or follow-up (individual work) (9 pts.) Professional References with appropriate in –text citation and reference list using APA format. All citations/reference list needs to be complete. (2 pts.) Total Points (25 pts.) Liver PBL case CC: Here because you told me my liver labs were bad. HPI: Taking medication as prescribed. No HA, dizziness, vision changes, CP, SOB, Abd pain, pain or swelling in legs. No N/V/D. No yellowing of skin or eyes. No change in stools or urine. Not routinely exercising- Just don’t have time with 2 kids and no husband to help and working full time. Just anxious and depressed at times. Cries for no reason. Unable to sleep or eat at times. Uses ETOH to help sleep. No SI or thoughts of self harm. Gets teary at work. Little interest in hobbies. Fatigued, occasionally feels worthless. Sometimes think should cut down ETOH. Husband left due to drinking- annoyed me. Feels guilty at times because not with kids when drinking, Never needed an eye-opener. Drinks 1-2 20 ounces of pop daily. 2-3 ETOH drinks. Smoke ½ PPD. PMH: No surgery, HTN, hyperlipidemia- no treatment other than diet. No blood transfusions. No liver, gall bladder or bleeding disorder Immunizations- no idea- had flu shot but not sure if others. Meds- HCTZ, Garlic, Tylenol NKDA Family history- no gall bladder disease, liver disease or bleeding problems Social: ½ PPD, ETOH as above- hard liquor, beer, wine. Married but separated, 12 partners lifetime 3 in past month. Occasionally uses condoms- if I remember. 2 children. Used IV meth and marijuana before. No foreign travel. Works in child care. ROS: general- no fever, chills, or night sweats, Fatigued at times. Feels well overall HEENT: no vision changes, yellow eyes, or sore throat CV: no CP, lightheadedness, or palpitations, no edema Resp: No SOB, cough, or wheezing Abd: no abd pain or N/V/D, no constipation, Appetite decreased lately- from stress, no abd edema Renal: No urgency, burning or hematuria Genitalia: No STI testing, no discharge, no sores or lesions MS- no muscle aches or pains, no decreased strength Neuro- no HA, dizziness, dec sensation, seizures or tremors Endo- no heat/cold intolerance, polyuria, polydipsia, or polyphagia Skin- no rashes, hair loss, brittle nails, or yellow skin, no dryness Lymph- no tender lymph nodes Ext- no decreased sensation Psych- feeling anxious and sad- depression after birth of child on Zoloft- quit 3 months after started. PA: 97 F, 160/88, HR 70, Ht 5 ft 10” Weight 210 pounds Eyes: PERRLA, 3mm bilat, optic disc crisp- no AV nicking, sclera white, conjunctiva clear Neck: supple, no thyroid enlargement or masses, no carotid bruits Lymph: no lymph node enlargement CV: S1S2 no S3S4 or murmurs, no heaves lifts or thrills Resp: clear Abd: BS + no renal, iliac, or femoral bruits, soft, mild right upper quadrant tenderness, no rebound tenderness, neg Murphy’s sign, liver span 16 cm , no spleen enlargement, no dullness to percussion, no hepatojugular reflex Gentiallia: no sores or lesions Ext: no edema MS- 5+ strength bilat, full ROM, no redness or swelling of joints Neuro: CN II to XII intact, reflexes 2+ bilat, neg Romberg, gait normal, finger to nose normal, no tremors Psych- tearful at times.