22_Immunodeficiency - V14-Study
advertisement
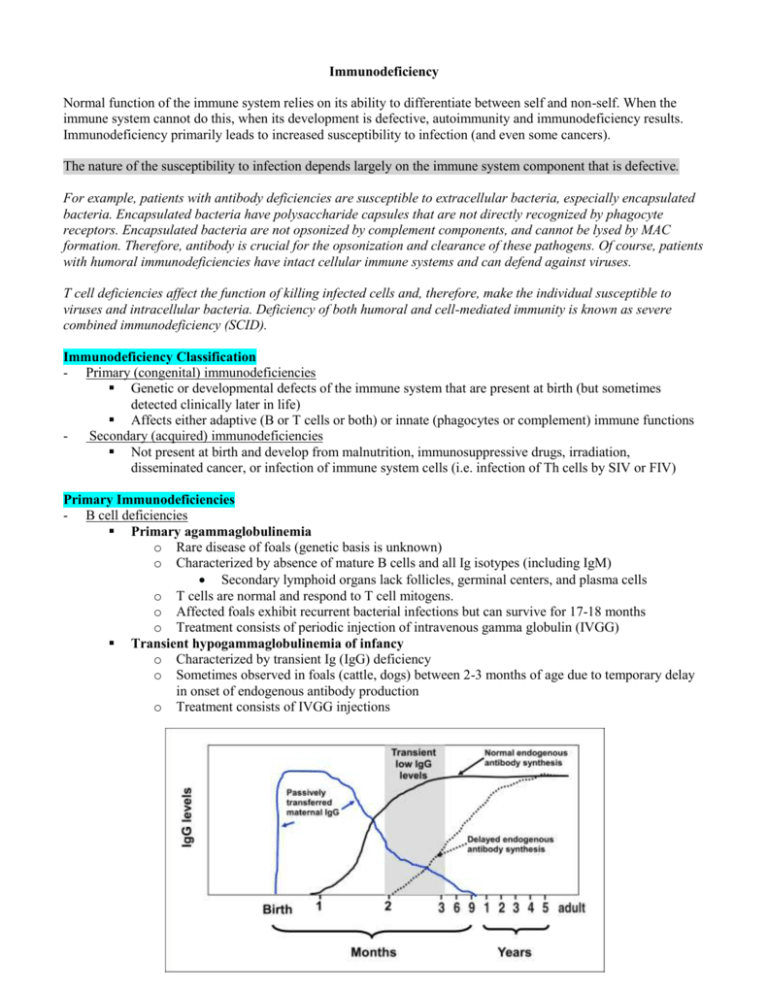
Immunodeficiency Normal function of the immune system relies on its ability to differentiate between self and non-self. When the immune system cannot do this, when its development is defective, autoimmunity and immunodeficiency results. Immunodeficiency primarily leads to increased susceptibility to infection (and even some cancers). The nature of the susceptibility to infection depends largely on the immune system component that is defective. For example, patients with antibody deficiencies are susceptible to extracellular bacteria, especially encapsulated bacteria. Encapsulated bacteria have polysaccharide capsules that are not directly recognized by phagocyte receptors. Encapsulated bacteria are not opsonized by complement components, and cannot be lysed by MAC formation. Therefore, antibody is crucial for the opsonization and clearance of these pathogens. Of course, patients with humoral immunodeficiencies have intact cellular immune systems and can defend against viruses. T cell deficiencies affect the function of killing infected cells and, therefore, make the individual susceptible to viruses and intracellular bacteria. Deficiency of both humoral and cell-mediated immunity is known as severe combined immunodeficiency (SCID). Immunodeficiency Classification - Primary (congenital) immunodeficiencies Genetic or developmental defects of the immune system that are present at birth (but sometimes detected clinically later in life) Affects either adaptive (B or T cells or both) or innate (phagocytes or complement) immune functions Secondary (acquired) immunodeficiencies Not present at birth and develop from malnutrition, immunosuppressive drugs, irradiation, disseminated cancer, or infection of immune system cells (i.e. infection of Th cells by SIV or FIV) Primary Immunodeficiencies - B cell deficiencies Primary agammaglobulinemia o Rare disease of foals (genetic basis is unknown) o Characterized by absence of mature B cells and all Ig isotypes (including IgM) Secondary lymphoid organs lack follicles, germinal centers, and plasma cells o T cells are normal and respond to T cell mitogens. o Affected foals exhibit recurrent bacterial infections but can survive for 17-18 months o Treatment consists of periodic injection of intravenous gamma globulin (IVGG) Transient hypogammaglobulinemia of infancy o Characterized by transient Ig (IgG) deficiency o Sometimes observed in foals (cattle, dogs) between 2-3 months of age due to temporary delay in onset of endogenous antibody production o Treatment consists of IVGG injections - Common variable immunodeficiency (CVID) o Diagnosed in adult horses (older than 3 years of age), though genetic basis is unknown o Presentation and pathogenesis is variable o Characterized by persistent B-cell lymphopenia (lack of mature B cells) and trace to low levels of all Ig isotypes, including IgG (hypogammaglobulinemia) o Patients typically present with recurrent bacterial infections Selective immunoglobulin deficiency o IgA deficiency Reported in several dog breeds (German shepherds are predisposed) Normal IgM and IgG levels, low IgA Normal IgA+ B cells and plasma cells in gut (suggests that impairment of mucosal IgA production is probably related to defective synthesis or secretion rather than reduced numbers of IgA-producing immunocytes) Patients may suffer from mucosal infections o IgG or IgG subclass deficiency Reported in foals, cattle, and dogs Normal IgM and IgA, low IgG Patients tend to be susceptible to respiratory disorders (i.e. pneumonia) o IgM deficiency Reported in foals (Arabia and Quarter horses are predisposed) Normal IgG and IgA levels, low IgM Affected foals exhibit recurrent respiratory infections and die by 10-24 months of age Severe combined immunodeficiency (SCID) Disorder that leads to lack of or defective humoral (B cell) and cell-mediated (T cell) immunity Characterized by several traits o Low lymphocyte levels Normal IgM levels (due to mother’s milk intake), low or absent IgG and IgA o Lack of or defective humoral and cellular immunity o Cells do not respond to mitogens o Cells cannot proliferate in response to antigens o Tonsils, thymus and lymph nodes are small or absent o Recurrent microbial infections of any kind Treatment consists of bone marrow transplantation from a histo-compatible donor Molecular mechanism of SCID in foals o Autosomal recessive disorder limited to Arabian horses o Foals rarely survive recurrent infections longer than 5 months of age o Caused by 5 base pair deletion of one DNA-PK catalytic subunit (DNA-PKcs), resulting in a frame-shift mutation and premature stop codon (DNA-PKcs is absent, no DNA-PK activity) Deoxyribonucleic acid-dependent protein kinase (DNA-PK), composed of three catalytic subunits (all required for functional activity), acts after RAG-1 and RAG-2 to rejoin cut DNA to produce genes for TCR and BCR Failure to properly complete gene rearrangemnt events (due to deficiency of DNA-PK, RAG-1, or RAG-2) results in elimination of lymphocyte precursors and near absence of functional T and B cells Molecular mechanisms of SCID in dogs o Absence of DNA-PKcs Occurs in Jack Russell Terriers A point mutation leads to premature stop codon and absence of DNA-PKcs o X-linked SCID due to mutation in common IL-2Rγ chain Occurs in Basset Hounds Mutation in gene coding the common γ chain of the IL-2R results in premature stop codon and translation of non-functional protein product o IL-2 receptor (IL-2R) is composed of three chains (IL-2Rα, IL-2Rβ, IL-2Rγ) Because γ chain is also found in receptors for IL-4, IL-7, IL-9, and IL-15, a defect in this chain impedes signaling through all these receptors Disease results from non-functional IL-7 o IL-7 is a lymphopoietic cytokine that stimulates immature thymocyte growth o Ensures availability of a large pool of progenitor cells to generate a highly diverse repertoire of antigen-specific T cells o In absence of IL-2Rγ chain, mature T cells do not develop Defective IL-15 contributes to immunodeficiency o IL-15 is a potent stimulator of NK cell proliferation o The absence of IL-2Rγ chain also results in NK cell deficiency o Disorders of Innate Immunity - Complement deficiencies – SEE PREVIOUS LECTURES - Canine cyclic neutropenia Autosomal recessive disease in collies Loss of neutrophils occurs about every 11-12 days and lasts for ~ 3 days Episodes of neutropenia are followed by normal or elevated neutrophil counts for ~7 days o Severe neutropenia suppresses inflammation and increases susceptibility to bacterial and fungal infections, commonly leading to GI and respiratory infections, gingivitis, lymphadenitis Etiology not clear but probably due to fluctuations in myeloid stem cell numbers due to abnormalities in myeloid growth factor production Patients rarely live past 3 years - Leukocyte adhesion deficiency Autosomal recessive disease in Holstein calves Caused by point mutation in gene coding for CD18 (β chain) o The integrin or adhesion molecule, leukocyte function-associated antigen-1 (LFA-1), is expressed on leukocytes and interacts with vascular endothelium, leading to firm attachment of leukocytes on endothelium and their migration to extravascular space o LFA-1 is composed of CD11a (α chain) and CD18 (β chain) o Lack of CD18 production results in dysfunction of LFA-1, resulting in inability of leukocyte migration to infected tissues Leads to recurrent bacterial infection, delayed wound healing, and chronic neutrophilia Patients usually die between 2-7 months of age - Chediak-Higashi syndrome Autosomal recessive disorder in cattle, Persian cats, white tigers, and killer whales Mutation in gene-LYST, a gene that regulated lysosomal trafficking within cells o Results in defective phagosome-lysosome fusion within neutrophils and other phagocytes o Phagocytosis is impaired o Produces abnormally large granules and lysosomes Patients are susceptible to bacterial infections and prognosis is poor Secondary Immunodeficiencies - Canine distemper virus (CDV) Infects young dogs Replicates in T cells of upper respiratory tracts and then disseminates to systemic lymph nodes, thymus, spleen, bone marrow, and GI lymphoid tissues Induces severe immunosuppression and lymphopenia (without significant decrease in leukocytes) o Results in bronchopneumonia, acute encephalitis, and demyelinating leukoencephalitis due to secondary infection (most serious complication is CNS infection) Pathogenesis remains unclear o Lymphopenia is probably due to virus-induced apoptosis o T cells are more affected than B cells o CD4+ cells are depleted for several weeks o CD8+ cells are less severely affected and recover relatively quickly - Retroviral-induced immunodeficiency Simian and Human immunodeficiency virus (SIV and HIV) o Primary viral receptor is CD4, which targets CD4+ T cells and results in their depletion and eventual development of acquired immunodeficiency syndrome (AIDS) o Acquisition of HIV also requires infection of co-receptors on dendritic cells and macrophages o Entry of HIV into cell is a multistep process Viral antigen, glycoprotein gp120, attached to CD4, resulting in conformational change in gp120 Conformational change promotes binding of gp120 to chemokine co-receptor (i.e. CCR5) Co-receptor binding induces conformational change in viral antigen gp41, which exposes a fusion peptide (hydrophobic region of gp41) that inserts into the host cell membrane Viral membrane fuses with the target cell membrane o Diagnosis of AIDS infection CD4+ T cells diminish (CD8 cells outnumber CD4 cells) Presence of antibodies to various lentiviral gene products (i.e. gp120) Presence of viral antigens in serum during infection Loss of delayed type hypersensitivity (Type IV DTH) skin tests Feline immunodeficiency virus (FIV) o Induces disease similar to AIDS o Characterized by progressive depletion of CD4+ T cells Results in wasting, CNS dysfunction, chronic infection, and increased lymphoma o In contrast to HIV, CD4 is not the primary viral receptor Viral receptor is CD134 (member of TNF receptor family) CD134 expression is greatest on activated CD4+ Th cells (not naïve Th cells) o Viral co-receptor is CXCR4 o CD4+ cells are the primary targets earlier in infection o CD8+ T cells and B cells are targeted in chronic infection o In chronic infection, FIV can adapt to infect only CXCR4 (CD134-independent infection) o Vaccination can lead to enhancement of AIDS-like infection and may be counterproductive CD134 is a T cell activation antigen Vaccination may induce expansion of a cell population expressing viral receptor