Chpt. 27: Fluid, Electrolyte, Acid-Base
advertisement

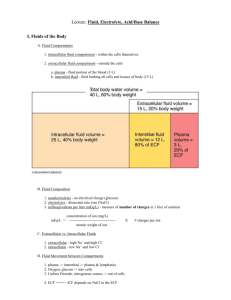
Chpt. 27: Fluid, Electrolyte, Acid-Base Balance Human Body consists of: water, proteins, lipids, minerals, carbohydrates, miscellaneous Body Fluids water accounts for 50-60% of body weight total body water depends on: skeletal muscle vs. adipose tissue Fluid Balance: amount of water gained = amount of water lost to environment Digestive system Urinary system Electrolyte Balance: balancing absorption in digestive tract with loss at sweat glands & urine Acid-Base Balance: – pH Kidney important for eliminating excess H+ and HCO3- ions Importance of Water: 99% of Extracellular Fluid Essential component of intracellular fluid Optimal heating/cooling Prevent mucus membranes from drying out Diffusion medium for gasses, nutrients, wastes Fluid Compartments: 2 main compartments to store water 1. Intracellular Fluid Compartment (ICF): cytosol 1 2. Extracellular Fluid Compartment (ECF): *1.) plasma 2.) interstitial fluid (IF) 3.) other – CSF, synovial exchange of water between plasma and IF due to HP and OP Composition of Body Fluids: water: solutes: electrolytes & nonelectrolytes 1. nonelectrolytes: do not dissociate 2. electrolytes: dissociate into ions in water -ions are charged particles, electrolytes more important for osmolarity Each fluid compartment has specific electrolytes ECF: chief cation: chief anions: chief cation: chief anion: ICF: Basic Concepts in the Regulation of Fluids and Electrolytes 1.) receptors monitoring fluids monitor ECF not ICF mainly plasma and CSF 2.) no receptors for water or specific electrolytes osmoreceptors monitor osmolarity of fluid plasma volume indicates water balance 2 3.) cells cannot move water by active transport: water moves via osmosis 4.) balance between intake and excretion determines overall fluid balance Main Hormones for Water/Electrolyte Balance: 1. ADH: released from? Released in response to Concentrates urine Stimulates thirst 2. Aldosterone: Released from Released in response to ↓plasma Na+ levels and/or ↑K+ Renin also triggers its release Increases reabsorption of Na+ 3. ANP Released from Released in response to ↑plasma Na+ levels and/or ↓K+ Increases secretion of Na+, H2O follows so it? Fluid Balance water circulates freely within ECF (from capillaries due to HP), in lymph, serous fluid, CSF water moves between ICF and ECF due to osmotic pressure (OP) 3 normally ECF and ICF are in osmotic equilibrium Water Gains: cellular metabolism Water Losses: urine, feces insensible perspiration: water vaporizes with breathing or through skin sensible perspiration: other: fever maintain tonicity of fluids via water shifts Fluid Shifts - water movement between ECF and ICF in response to osmotic gradient • if ECF osmotic concentration increases, it becomes hypertonic: • If ECF osmotic concentration decreases, it becomes hypotonic: Note ICF volume higher than ECF ICF acts as water reserve Remember: anything that changes solute concentration effects osmotic pressure Edema: anything that increases fluid flow out of bloodstream or decreases its return factors that increase fluid loss: 1. increased capillary hydrostatic pressure: 4 2. increased capillary permeability: Dehydration: water loss exceeds water intake -common with hemorrhage, severe burns, vomiting, diarrhea, sweating, water deprivation, diuretic abuse and endocrine disorders water loss from ECF so Na ion concentrations increase (hypernatremia) increased plasma osmolarity causes: 1. 2. Thirst Mechanism: • decrease plasma vol. by 10% and/or increased in plasma osmolarity triggers hypothalamic thirst center. • hypertonic plasma pulls water from salivary glands which creates dry mouth • when water leaves cells in thirst center (hypothalamus) it depolarizes them = sensation of thirst • thirst quenched Overhydration – water excess Hypotonic Hydration: water intoxication renal insufficiency, drinking large amounts very quickly, renal failure, heart failure, endocrine disorder hyponatremia -causes water to - s/s: confusion, hallucinations, convulsions, coma, death 5 -must be infused with IV of salt (hypertonic) solution Electrolyte Balance: (salts, acids, bases) salts important for most important are: salts: thru foods & water salts lost thru GI disorders: renal mechanisms extremely important: (table 27-2 page 1010 causes & consequences of electrolyte imbalances.) Sodium Balance (135 – 145 mEq/L) Na+ salts 90% of all solutes in Na+ important for: cause mosm of total 300 mosm Sodium Balance: Gains via digestive tract vs. losses from urine/perspiration hypernatremia (>145 mEq/L): dehydration triggers thirst center in hypothalamus & release of ADH hyponatremia (<135 mEq/L): water intoxication inhibits release of ADH 6 Regulation of Sodium Balance: (function to restore BV & BP) 1. Aldosterone: secreted by Controls Na+ reabsorption in DCT with or without Aldosterone:75-80% Na+ reabsorbed in PCT w/ aldosterone: remaining 20-25% is reabsorbed in DCT Triggers for Aldosterone: Addison's Disease: 2. ADH: released from regulates water reabsorption in DCT & decreased ADH: increased ADH: osmoreceptors in hypothalamus sense osmolarity of plasma 3. ANF (Atrial Natriuretic Factor) hormone released from released in response diuretic and natriuretic 7 promotes excretion inhibits distal tubule cells ability inhibits release of 4. Other Hormones: A. estrogens: similar to aldosterone B. progesterone: C. glucocorticoids: cortisol Potassium (K+) Balance (3.8 – 5.0 mEq/L) main intracellular cation (98% in ICF) necessary for: RMP, neuromuscular functioning balance due to rate of absorption vs losses in urine 3 factors determine the rate of K secretion from tubules: 1. K+ concentration in the ECF: higher ECF concentration increases rate of secretion 2. pH of ECF: H+ & K+ compete for secretion for every Na+ reabsorbed therefore if pH decreases: H+ secretion if pH increases: H+ secretion and K secretion and K secretion 3. Aldosterone levels: stimulates reabsorp. of Na and excretion of K 8 1:1 exchange adrenal cortex cells sense hyperkalemia (>5 mEq/L): from renal failure, chronic acidosis causes cardiac arrhythmias, muscle spasms hypokalemia (<3.5 mEq/L): from low-K diet, diuretics, hypersecretion of aldosterone, chronic alkalosis cells hyperpolarize: muscle weakness, paralysis, cardiac arrest Calcium Balance (4.3 – 5.3 mEq/L) most abundant mineral in body - 99% of calcium found in Ca++ important for: calcium levels regulated by PTH and calcitonin PTH: 1. increases calcium levels by reabsorbing Ca++ from bones (osteoclasts) 2. increases intestinal absorption of Ca++ 3. increases Ca++ reabsorption by kidney tubules Calcitonin: 1. decreases blood calcium levels by putting calcium into bones (osteoblasts) hypercalcemia (>11 mEq/L): confusion, muscle pain, cardiac arrhythmias, kidney stones hypocalcemia (<4 mEq/L): muscle spasms, convulsions, cramps, weak heart beat, cardiac arrhythmias, osteoporosis 9 Magnesium (Mg) Balance (1.4 – 2.0 mEq/L) important for: bone structure, co-factor for enzymes 60% found in the skeleton and higher in ICF then ECF hypermagnesemia: confusion, lethargy, respiratory depression, hypotension hypomagnesemia: hypocalcemia, muscle weakness, cramps, cardiac arrhythmia Phosphate Balance important for: bone mineralization, metabolism, synthesis of nucleic acids Chloride Balance (100-108 mEq/L) major anion in ECF: follows Na+ absorbed across digestive tract with Na+ hyperchloremia causes acidosis hypochloremia causes alkalosis, muscle cramps Acid-Base Balance pH of body fluids is altered by acids & bases strong vs. weak acids & bases: strong acids completely dissociate into H+ weak acids do not completely dissociate strong bases completely dissociate into OH- 10 critical for homeostasis arterial blood pH: interstitial fluid and venous blood pH: Acidosis: physiological state resulting from abnormally low plasma pH blood pH < 7.35: acidosis* or acidemia *note: 7-7.35: physiological acidosis Alkalosis: physiological state resulting from abnormally blood pH > 7.45: alkalosis or alkalemia Both effect all body systems – especially nervous & cardioavascular Acidosis more common because acidosis can be fatal – CNS degenerates – coma cardiac contractions become weak, irregular circulatory collapse from vasodilation Acids classified as: 1. volatile: can leave solution and enter atmosphere Carbonic acid 2. fixed & organic: from metabolism phosphoric and sulfuric acid from protein metabolism are fixed acids Lactic acid, pyruvic acid, ketone bodies: organic acids 11 Volatile Acids: Most CO2 in solution converts to carbonic acid which dissociates PCO2 most important factor affecting pH in body tissues PCO2 and pH are inversely related: CO2 levels ↑ = ↑H+ = ↓ pH H+ ion concentration regulated by: 1. Chemical Buffers 2. Respiratory Buffers 3. Renal Mechanisms Mechanisms of pH control: balance gains and losses of H+ Through buffers: buffers are dissolved compounds that stabilize pH by providing or removing H+ 1. Chemical Buffers: acids: proton donors: -acidity: due to Weak acids: Strong acids: bases: proton acceptors -strong bases: hydroxides: 12 -weak bases: HCO3 and NH3 Chemical Acid-Base Buffers: buffer pairs when pH decreases: weak base binds to/picks up H+ to when pH increases: 3 major chemical buffers: (figure 27-10 page 1014) A . Protein Help regulate pH in ECF and ICF B. Sodium – Bicarbonate: Carbonic Acid - Bicarbonate C. Phosphate Buffers pH of ICF and urine A. Protein Buffer System: depends on amino acids Amino acids have carboxyl (acid) groups COOH: which functions as an acid R - COOH --> R-COO + H+ the same protein molecule also has NH2 which functions as a base R-NH2 + H+ --> R-NH3 amphoteric molecules: function as The Hemoglobin Buffer System Hydrogen ions from CO2 loading are buffered by hemoglobin molecules CO2 + HHb ↔HbCO2 + H+ O2 + HHb ↔ HbO2 + H+ B. Sodium- Bicarbonate System 13 in ECF and ICF H2CO3 and NaHCO3 HCl + NaHCO3 --> H2CO3 + NaCl When buffering strong acid – the weak base is used to convert the strong acid into a weak acid Goal: to replace strong acid with weak acid (and salt by-product) NaOH + H2CO3 --> NaHCO3 + H2O When buffering strong base – the weak acid is used to convert the strong base into a weak base Goal: to replace strong base with weak base (and water by-product) w/i cells K and Mg bicarb. help w/ bicarb. system the buffering power is directly proportional to the concentration of the buffers need base bicarb. (BB) to carbonic acid ratio of 20:1 C. Phosphate Buffer System: uses phosphate: weak acid: NaH2PO4 weak base: Na2HPO4 When buffering a strong acid: the weak base is used to convert the strong acid into a weak acid HCl + Na2HPO4 --> NaH2PO4 + NaCl and if buffer a strong base: The weak acid is used to convert the strong base into a weak base NaOH + NaH2PO4 --> Na2HPO4 + H2O 14 Limitations of these buffers: Provide temporary solutions – do not eliminate H+ ions Maintenance of Acid–Base Balance For homeostasis to be preserved, captured H+ must: 1. Be permanently tied up in water molecules: – through CO2 removal at lungs 2. Be removed from body fluids: – through secretion at kidney 2. Respiratory System Regulation Respiratory system is a physiological buffer: ties up H+ in H2O Cannot protect ECF from changes in pH that result from Functions only when respiratory system and control centers are working normally Ability to buffer acids is limited by if pH decreases: if pH increases: 3. Renal Mechanisms: 15 Renal Compensation Is a change in rates of H+ and HCO3- secretion or reabsorption by kidneys in response to changes in plasma pH The body normally generates enough organic and fixed acids each day to add 100 mEq of H+ to ECF Kidneys assist lungs by eliminating any CO2 that Enters renal tubules during filtration Diffuses into tubular fluid en route to renal pelvis rids body of acids metabolic acidosis: results from their accumulation H+ enter filtrate and must be buffered Regulation of H+ ion Secretion in Urine tubule cells respond to pH of ECF and changes H+ secretion accordingly for every H+ secreted into tubule 1 Na+ reabsorbed H+ secretion is dependant on CO2 levels Bicarbonate Ions: alkaline reserve -must replenish stores of HCO3 in blood -tubule cells very impermeable to HCO3 in filtrate: can't reabsorb them from filtrate -pure H+ ions not excreted directly in urine = decrease urine pH too low 1. First buffered by HCO3 in filtrate -if HCO3 "used up" must secrete H+ into urine. These H+ are then buffered by carbonic-acid buffers 16 2. phosphate buffer system 3. ammonium buffer system 2. Phosphate Buffer System H + Na2HPO4 --> NaH2PO4 which leaves in urine 3. Ammonium Buffer System uses NH3 produced from the metabolism of NH3 diffuses into filtrate and: NH3 + H+ --> NH4 (ammonium) Renal Response to Acidosis: ↑ secretion of H + (less K+ is secreted) ↓ secretion of HCO3- (more Cl- is secreted) Renal Response to Alkalosis: ↓ secretion of H + (more K+ is secreted) 17 - - ↑secretion of HCO3 (less Cl is secreted) Abnormalities of Acid Base Balance Acute: the initial phase Compensated: when condition persists Respiratory: imbalance with CO2 Metabolic: generation of organic or fixed acids 1. Respiratory Acidosis or Alkalosis caused by failure of PCO2 most important indicator of respiratory function normal range: 35 – 45 mmHg respiratory acidosis: Acute: cardiac arrest or drowning Chronic: COPD, pneumonia respiratory alkalosis: Acute: pain, anxiety 2. Metabolic Acidosis or Alkalosis all other abnormalities of acid-base imbalance except those caused by PCO2 levels HCO3 most important indicator of metabolic acidosis/alkalosis normal values 22 - 28 mEq/L metabolic acidosis: 18 1.production of large numbers of fixed or organic acids: ketoacidosis, alcohol poisoning, lactic acidosis 2. Impaired H+ excretion at kidneys 3. Severe bicarbonate loss: diarrhea metabolic alkalosis: 1. Too much HCO3- (constipation, overuse of antacids) 2. Loss of H+ (vomiting) Compensated Acidosis/Alkalosis: one system fails the other “compensates” Respiratory Acidosis: pH= PCO2= HCO3- = Respiratory Alkalosis: pH= PCO2= HCO3- = Metabolic Acidosis: pH= PCO2= HCO3- = Metabolic Alkalosis: pH= PCO2= HCO3- = Anion gap (AG): shows amount of unmeasured anions – a calculation AG = Na+ - [Cl-] + [HCO3-] (are usually more unmeasured anions than cations so its usually + value Normal 3- 11 mmol/L Every HCO3 lost is replaced by a Cl- anion: diarrhea, Kidney loss of HCO3- If increases shows loss of HCO3 without increase in Cl (HCO3 is being used to buffer the acid and the HCO3 negative charge is being replaced with nonmeasured anions (lactate, PO4-, acetoacetate) Interstitial fluid (IF) is too negative 19 anion-gap metabolic acidosis: (ketoacidosis, respiratory failure (cells use anaerobic metabolism), kidney damage, some poisons, excessive aspirin, antifreeze 20