Minor Office Surgery Chapter 14 Clinical Procedures 10

Minor Office Surgery
Chapter 14 Clinical Procedures
KEY TERM ASSESSMENT
A. Definitions
1. M
2. E
3. T
4. U
5. V
6. L
7. N
8. I
9. S
10. B
11. K
12. R
13. Y
B. Word Parts
14.
O
15.
J
16.
F
17.
W
18.
D
19.
A
20.
H
21.
X
22.
C
23.
G
24.
Z
25.
P
26.
Q
Word Part Meaning of Word Part Medical Terms That Incorporate Word
Part
1. bi/o
2. -opsy life to view
3. colp/o vagina
4. -scope
5. -scopy
6. cry/o
7. fibr/o
8. hem/o
9. stasis instrument used for visual examination visual examination cold fibrous tissue blast: developing cell blood control, stop
EVALUATION OF LEARNING
1.Performed in an ambulatory health care facility; can be performed in a short period of time; requires either a local anesthetic, topical anesthetic, or no anesthetic; can be performed safely with a minimum of discomfort to the patient; and does not, under normal circumstances, pose a major risk to life or function of an organ or body parts.
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery 10-2
Chapter 14 Clinical Procedures
2. Explaining patient preparation required for the procedure, obtaining the patient’s signature on a consent form, preparing the treatment room, preparing the patient, preparing the minor surgery tray, assisting the physician during the procedure, administering postoperative care of the patient, and cleaning the treatment room
after the procedure.
3. Are sawlike teeth that grasp tissue and prevent it from slipping out of the jaws of the
instrument.
4. Mosquito hemostatic forceps are used to hold delicate tissue or to clamp off smaller blood vessels. Standard hemostatic forceps are used to grasp and compress larger
blood vessels.
5. To open or distend a body orifice or cavity to permit visual inspection.
6.
Handle instruments carefully.
Do not pile instruments in a heap.
Keep sharp instruments separate from other instruments.
Keep instruments with a ratchet in an open position when not in use.
Rinse blood and body secretions off an instrument as soon as possible.
Always use the instrument for the purpose for which it was designed.
Sanitize and sterilize instruments using proper technique.
7. A closed wound is an injury to the underlying tissues of the body without a break in the skin surface or mucous membrane, whereas an open wound has a break in the skin or
mucous membrane that exposes the underlying tissue.
8. Tetanus bacteria grow best in a warm anaerobic environment as would be found in
a puncture wound.
9. To destroy invading microorganisms and to remove damaged tissue debris from the
area so that proper healing can occur.
10. Redness, swelling, pain, and warmth.
11. A fibrin network forms, resulting in a blood clot that plugs the opening of the wound
and stops the flow of blood.
12. Fibroblasts migrate to the wound and synthesize collagen and a growth of new
capillaries.
13. Collagen continues to be synthesized. The granulation tissue eventually hardens into
white scar tissue.
14. Material, such as fluid and cells, which has escaped from blood vessels during the
inflammatory process.
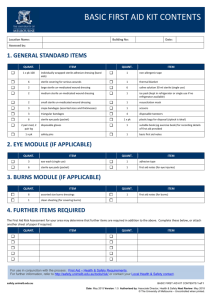
15. a. Serous Contains serum and appears clear and watery. b. Sanguineous Red in color and composed of red blood cells. c. Purulent Contains pus and is usually thick and has an unpleasant odor. It is white in
color but may acquire tinges of pink, green, or yellow. d. Serosanguineous Consists of clear and blood-tinged drainage. e. Purosanguineous Consists of pus and blood.
16. To protect the wound from contamination and trauma, to absorb drainage, and to
restrict motion.
17. a. 4-0 silk
2-0 silk
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery 10-3
Chapter 14 Clinical Procedures b. 0 chromic surgical gut
3-0 chromic surgical gut c. 2-0 polypropylene
2 polypropylene
18. Silk, nylon, polyester, polypropylene, polybutester, stainless steel, and surgical skin
staples.
19. The needle is permanently attached to the end of the suture. The suture material does not slip off the needle; tissue trauma is reduced because there is only a single
strand of suture that must be pulled through the tissue.
20. This area has a better blood supply and heals more rapidly.
21. This is the fastest method of closure of long skin incisions, and trauma to the tissue is
reduced because the tissue does not have to be handled much during insertion.
22. Eliminate the need for skin sutures and a local anesthetic, are easy to apply and
remove, and result in less scarring than skin sutures.
23. To reduce the risk of surgical wound contamination.
24. To provide a sterile area around the operative site to decrease contamination of
the surgical wound.
25. Xylocaine (lidocaine hydrochloride).
26.In its functional position and in a firm, confident manner so that it does not slip out of
the physician’s hand.
27. A thin, closed sac or capsule located just under the surface of the skin containing secretions from a sebaceous gland. It forms when the outlet of a sebaceous gland
becomes obstructed.
28. To keep the edges of the tissue held apart to facilitate drainage of the exudate.
29. Congenital nevi are moles that an individual is born with. Acquired nevi are moles
that develop over time.
30. Small, painless, benign growths that project from the skin from a narrow stalk
(peduncle). They are most frequently found in body areas where the skin creases
such as the eyelids, neck, armpits, upper chest, and groin.
31. They are usually larger than normal moles and have an irregular coloration and shape. The center may be raised and darkened; they are more likely than ordinary
moles to develop into malignant melanoma.
32. Asymmetrical, irregular border, color varies from one area of the mole to another, diameter is larger than ¼ inch, and the mole is painful, tender, itches, bleeds, oozes,
or has a scaly appearance.
33. Shave excision, surgical excision, and laser surgery.
34. To determine whether a tumor is malignant or benign or to determine the presence
of an infection.
35. Occurs when the edge of the toenail grows deeply into the nail groove and
penetrates the surrounding skin.
36. Tight shoes or hose, trauma, improper nail trimming, and infection.
37. To follow abnormal Pap test results and to evaluate a vaginal or cervical lesion
observed during a pelvic examination.
38. To detect the presence of cervical dysplasia or cancer of the cervix; also used to diagnose polyps on the cervix and genital warts.
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery 10-4
Chapter 14 Clinical Procedures
39.
1. A minimum amount of cramping and bleeding may follow the procedure and last
up to 1 week. Contact the medical office if the bleeding lasts longer than 2 weeks.
2. If Monsel’s solution is used to control bleeding, a thick, dark-colored vaginal
discharge may occur following the procedure and last for several days.
3. Do not douche, use tampons, or have intercourse for 1 week following the
procedure to allow proper healing of the cervix to take place.
4. Contact the medical office if the following occur: bleeding that is heavier than normal menstrual bleeding, a foul-smelling vaginal discharge, fever, or lower
abdominal pain.
5. An appointment is scheduled approximately 1 week following the procedure to
make sure that healing is taking place and to discuss the biopsy results.
40. To treat cervical dysplasia and chronic cervicitis.
41.
1. Normal activities can be resumed the day following the cryosurgery.
2. On the first postoperative day, a clear, watery vaginal discharge occurs, which
lasts for 2 to 4 weeks.
3. Use sanitary pads (rather than tampons) to absorb the watery discharge.
4. Do not douche, use tampons, or have intercourse for 2 to 3 weeks following the
procedure to allow proper healing of the cervix to take place.
5. Contact the medical office if any of the following occur: bleeding that is heavier than normal menstrual bleeding, a foul-smelling vaginal discharge, fever, or lower
abdominal pain.
6. The patient must schedule a return visit 6 weeks after the procedure to ensure that
proper healing has occurred.
42. To apply pressure; control bleeding; protect the wound from contamination; hold a
dressing in place; and protect, support, or immobilize an injured part of the body.
43.
Observe the principles of medical asepsis.
Make sure the area to which the bandage is applied is clean and dry.
Do not apply a bandage directly over an open wound.
Do not allow the skin surfaces of two body parts to touch.
Pad joints and prominent parts of bones.
Bandage the body part in its normal position with joints slightly flexed.
Apply the bandage from the distal to the proximal part of the body.
As you apply the bandage, ask the patient if it feels comfortable.
If possible, leave the fingers or toes exposed when bandaging an extremity to check
for signs of circulation impairment.
Obtain a new bandage if the bandage roll has dropped during the procedure.
44. Coldness, pallor, numbness, cyanosis of the nailbeds, swelling, pain, and tingling
sensations.
45. It is easy to apply it too tightly and impede circulation.
46. Allows for a smoother fit and keeps the bandages from gaping because of the
variations in the contour of the limb
47. To hold a dressing in place or to support and immobilize an injured joint.
48. Circular.
49. Fingers, toes, arms, and legs.
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery
Chapter 14 Clinical Procedures
50. It is easier to apply, and it adheres more securely to the body part.
CRITICAL THINKING ACTIVITIES
10-5
A. Medical and Surgical Asepsis
1. Administering oral medication Medical asepsis.
2. Inserting sutures Surgical asepsis: caring for broken skin.
3. Measuring oral temperature Medical asepsis.
4. Applying a bandage to the forearm Medical asepsis.
5. Performing a needle biopsy Surgical asepsis: penetrating a skin surface.
6. Removing a sebaceous cyst Surgical asepsis: penetrating a skin surface.
7. Obtaining a Pap specimen Medical asepsis.
8. Inserting a urinary catheter Surgical asepsis: entering a body cavity that is normally
sterile.
9. Incision and drainage of an abscess Surgical asepsis: penetrating a skin surface.
10. Applying a dressing to an open wound Surgical asepsis: caring for broken skin.
B. Violation of Surgical Asepsis
1. Placing a sterile 4 × 4 within the 1-inch border around the sterile field A 1-inch border around the field is considered contaminated because this area may have become
contaminated when the sterile field was being set up.
2. Wearing rings during the application of sterile gloves Rings may cause the gloves to
tear.
3. Talking over a sterile field Water vapor from the nose, mouth, and lungs is carried out
by the air and contaminates the sterile field.
4. Reaching over a sterile field Dust or lint from the MA’s clothing may fall onto the
sterile field, or the MA’s nonsterile clothing may accidentally touch it.
5. Holding sterile gauze below waist level Anything out of sight may become
contaminated.
6. Not palming the label when pouring an antiseptic solution This may allow solution to
drip on the label, obscuring it.
7. Spilling an antiseptic solution on the sterile field If the sterile field becomes wet, microorganisms can be drawn onto the field by capillary action, resulting in
contamination.
8. Passing a soiled dressing over the sterile field This contaminates the sterile field.
9. Placing a vial of Xylocaine on the sterile field Articles that are medically aseptic
cannot be placed on the sterile field because they would contaminate it.
10. Using bare hands to arrange articles on the sterile field Sterile gloves must be used.
Bare hands would contaminate the sterile articles.
C. Surgical Instruments
1. Needle holder: Used to grasp a curved needle.
2. Retractor: Used to hold tissue aside to improve the exposure of the operative area.
3. Splinter forceps: Used to remove a foreign object from the tissues.
4. Standard hemostatic forceps: Used to grasp and compress larger blood vessels.
5. Suture scissors: Used to remove sutures.
6. Operating scissors: Used to cut through tissue.
7. Thumb forceps: Used to pick up tissue or hold tissue between adjacent surfaces.
8. Scalpel: Used to make surgical incisions and divide tissue.
9. Bandage scissors: Used to remove a dressing or bandage.
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery 10-6
Chapter 14 Clinical Procedures
10. Sponge forceps: Used to hold sponges.
11. Tissue forceps: Used to grasp tissue.
12. Mosquito hemostatic forceps: Used to hold delicate tissue and clamp off smaller
blood vessels.
13. Uterine tenaculum: Used to grasp and hold the cervix.
D. Pioneers in Surgical Asepsis
1. Ignaz Semmelweis Semmelweis was a pioneer in the use of aseptic technique during childbirth. He recognized that infection was carried from one patient to another by physicians, and he advocated preventive measures such as handwashing during
surgery.
2. Louis Pasteur Pasteur is the founder of microbiology and showed that microorganisms cause disease. Pasteur showed that the spoiling of wine by microorganisms could be prevented by partial heat sterilization, which led to the pasteurization of milk and
other perishable foods.
3. Joseph Lister Lister advocated the use of asepsis during surgery to prevent the
development of infection in wounds.
E. Crossword Puzzle: Minor Office Surgery
Across
1 Drape with a hole
4 Produces collagen
6 Clean, smooth cut
8 Boil
9 Sac containing oil secretions
14 Pus formation
15 Clamps off blood vessels
17 Local anesthetic brand name
20 Pus in a cavity
22 Tetanus may grow here
23 A local sign of inflammation
24 Bring together
APPLY YOUR KNOWLEDGE
2 Free of all MOs and spores
3 Bruise
Down
5 Scrape
7 Exudate containing blood
10 Suture/needle combination
11 Tx for chronic cervicitis
12 Father of modern surgery
13 Ragged and irregular wound
16 Discovered penicillin
18 Position for colposcopy
19 Antiseptic brand name
21 Nonabsorbable suture material
1. D. Microorganisms from his mouth can contaminate the sterile field.
2. C. Cover the tray with a sterile towel and leave to get the sutures.
3 .B. Opening the sterile package and allowing Dr. Xylocaine to remove the gauze with his gloved hand
4. B. Phase 2, or the granulation phase
5. D. Lidocaine local anesthetic vial
6. E. All of the above
7. D. Verify that Eric’s mother has discussed the procedure with Dr. Xylocaine and has signed a consent to treatment form
8. A. Soak his foot in tepid water and an antiseptic solution
9. A. Placing the bottle cap on a flat surface with the open end facing down
10. A. Bruising
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery
Chapter 14 Clinical Procedures
VIDEO EVALUATION FOR CHAPTER 10: MINOR OFFICE SURGERY
10-7
Video: Procedure 10-1: Applying and Removing Sterile Gloves
____T___1. Sterile gloves must be worn when changing a sterile dressing.
____F___2. Rings do not need to be removed before applying sterile gloves.
____F___3. Before applying sterile gloves, the hands must be rinsed with Betadine.
____T___ 4. If your gloves are too small, they may rip as you apply them or become uncomfortable to wear.
____F___5. The inside of the glove wrapper is considered contaminated.
____T___6.The first glove should be picked up by the folded back-cuff with the fingers of the opposite hand.
____F___7. The hands should be kept below waist level while gloving.
____T___8. When removing gloves, the bare hands should not be allowed to come in contact with the outside of the gloves.
____T___9. Gloves that are visibly contaminated with blood or other potentially infectious materials should be discarded in a biohazard waste container.
____T___10. After gloves are removed, OSHA requires that the hands be sanitized to remove any microorganisms that might have come in contact with the hands.
Video: Procedures 10-2 and 10-3: Sterile Technique
____T___1. The items included in a sterile pack, depend on the type of procedure to be performed.
____T___2. The inside of a sterile package can be used as a sterile field.
____T___3. A sterile pack that is wet, torn, or opened is contaminated and cannot be used.
____F___4. Autoclave tape that has changed color indicates that the contents of the pack are sterile.
____T___5. An outdated antiseptic solution should not be used because it may produce an undesirable effect.
____T___6. Talking, laughing, coughing, or sneezing over a sterile field contaminates it.
____T___7. Reaching over the contents of a sterile field contaminates it.
____F___8. A 4-inch border around the sterile field is considered contaminated because this area may become contaminated while setting up the sterile field.
____T___9. A 4 × 4 gauze pad should be gently ejected onto the center of the sterile field.
____T___10. The label of the antiseptic solution should be palmed while pouring the solution.
____F___11. After removing the cap from the antiseptic solution, it should be placed on the sterile field with the open end facing up.
____T___12. Holding the solution bottle too high while pouring it may cause the antiseptic to splash onto the sterile field and contaminate it.
Video: Procedure 10-4: Changing a Sterile Dressing
____T___1. Surgical asepsis must be maintained when caring for an open wound and applying a sterile dressing.
____T___ 2. The size, type, and amount of dressing material used depend on the size and location of the wound and the amount of drainage from the wound.
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery 10-8
Chapter 14 Clinical Procedures
____T___ 3. The function of a sterile dressing is to protect an open wound from contamination and trauma.
____F___ 4. A soiled dressing should be removed by gently dragging it horizontally across the wound.
____T___ 5. The inside of the dressing should not be touched to prevent transferring an infected discharge to your gloves.
____T___6. The wound should be inspected for the amount of healing and the presence of drainage.
____F___7. The antiseptic should be applied from the top to the bottom of the wound, working from the outside to the center of the wound.
____T___8. The sterile dressing should be placed over the wound by lightly dropping it in place.
____F___9. The patient should be instructed to keep the wound clean and moist.
____T___10. Signs indicating that the wound is infected include swelling, discharge, and pain.
____T___11. The original signed copy of the wound care instructions protects the physician legally in the event the patient does not follow the wound care instructions and causes harm to the wound.
____T___12. The bag of contaminated items should be discarded in a biohazard waste container.
Video: Procedure 10-5: Removing Sutures and Staples
____T___1. Sutures approximate the edges of a wound and hold them in place until healing occurs.
____T___2. Sutures and staples minimize the amount of scar formation.
____T___3. The sutures should not be removed if the incision line is not approximated, or if redness, swelling, or discharge is present.
____F___4. Removing dried exudates from the suture line makes it harder to remove the sutures.
____T___5. Do not allow any portion of the suture that was previously outside to be pulled through the tissue lying beneath the incision line.
____T___6. The number of sutures should be counted as they are removed.
____F___7. Suturing is the fastest method of closure of long skin incisions.
____T___8. The patient should be told that a pulling sensation may be felt as each staple is removed.
____T___9. When staples are removed, the bottom jaws of the staple remover are placed under the staple to be removed.
____F___10. The staple remover should be lifted at an angle to remove the staple from the incision line.
Video: Procedure 10-6: Applying Adhesive Skin Closures
____T___1. Adhesive skin closures consist of sterile strips of tape available in different lengths.
____F___2. A local anesthetic must be used when applying adhesive skin closures.
____F___3. Sutures have a lower incidence of wound infection than adhesive skin closures.
____T___4. An antiseptic must be applied to the site before applying adhesive skin
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.
Minor Office Surgery 10-9
Chapter 14 Clinical Procedures closures.
____F___5. Applying Betadine helps the adhesive strips adhere to the patient’s skin.
____T___6. The first adhesive strip should be positioned over the center of the wound.
____F___7. The adhesive strips should be applied at one-inch intervals until the edges of the wound are approximated.
____T___8. The skin closures will loosen and fall off on their own approximately 5 to 10 days after they have been applied.
Video: Procedure 10-7: Assisting with Minor Office Surgery
____T___1. Non-sterile articles needed for the minor office surgery are set up on a side table or counter.
____T___2. The sterile tray can be set up using a prepackaged setup or by transferring articles to a sterile field.
____T___3. A fenestrated drape only exposes the operative site and maintains a sterile field around the site.
____F___ 4. The patient should be asked to sign a consent to treatment form after the surgery is completed.
____T___5. The patient should be asked if he needs to void before the minor office surgery.
____T___6. If the patient sneezes on the sterile field, microorganisms from the mouth, nose, and lungs can be transferred to the sterile field.
____F___7. Clean gloves must be worn when handing the physician a sterile instrument during the minor office surgery.
____T___7. A biopsy request form must accompany the tissue specimen to the laboratory.
____T___8. Blood and body secretions should be rinsed off the instruments immediately to prevent them from drying and hardening on the instruments.
Video: Procedure 10-A: Bandage Turns
____T___1. Bandages are used for support, immobilization, and holding a dressing in place.
____F___2. The bandage turn that is used depends on the patient’s age and physical condition.
____T___ 3. The circular turn is applied to a part of uniform width, such as toes, fingers, or the head.
____T___4. The circular turn is used to anchor a bandage.
____T___ 5. The spiral turn is applied to a part of uniform circumference, such as the fingers, arms, legs, chest, or abdomen.
____T___ 6. Each spiral turn is carried upward at a slight angle and should overlap the previous turn by one half to two thirds of the width of the bandage.
____T___ 7. The spiral-reverse turn is used to bandage a part that varies in width, such as the forearm or lower leg.
____T___8. Reversing each spiral turn allows for a smoother fit and prevents gaping caused by the variation in the contour of the limb.
____T___9. The figure-eight turn is used to hold a dressing in place or to support and immobilize an injured joint, such as the ankle, knee, elbow, or wrist.
Notes
Copyright © 2012, 2008, 2004, 2000, 1995, 1990, 1984, 1979 by Saunders, an imprint of Elsevier Inc.