Goals and Objectives Medical University of South Carolina Pediatric
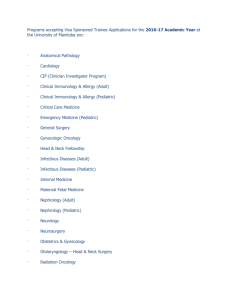
advertisement

Goals and Objectives Medical University of South Carolina Pediatric Emergency Medicine Fellowship Pediatric Emergency Medicine Rotation First Year Goals: 1. Gain experience in managing Pediatric Emergency Department patients. 2. Learn to provide care to ill and injured children of all levels of acuity. 3. Learn to prioritize and simultaneously care of multiple patients. 4. Learn to be an effective team member who works efficiently with nurses, ancillary services and consulting physician groups. 5. Assume bedside teaching role for junior residents and medical students. 6. Be exposed to the many administrative tasks related to providing Pediatric Emergency care (scheduling, billing, patient satisfaction, quality improvement and implementing research projects). Patient Care: Evaluation tools: Attending direct observation, Press Ganey patient satisfaction surveys/ phonecall ED visit follow-up surveys by nursing staff, Simulation Lab, 360 multisource assessment, Procedure skills documentation and performance in labs 1. Provide state of the art pediatric emergency management of common pediatric emergencies and urgencies, including, but not limited to: respiratory distress, seizures, cardiac arrhythmias, allergic reactions, toxic ingestions, hypoglycemia, diabetic ketoacidosis, meningitis, appendicitis, pelvic inflammatory disease, intussusception, volvulus, febrile neonate and infant, fever and neutropenia, and testicular torsion. 2. Perform common pediatric procedures including, but not limited to: lumbar puncture, simple and complex laceration repair, reduction of commonly dislocated joints, esophageal bougienage, hernia reduction, splinting, intravenous, intraosseous and central venous line placement, tracheal intubation with and without rapid sequence induction/intubation, chest tube placement, cardioversion and procedural sedation. Medical Knowledge: Evaluation tools: Attending direct observation, SITE testing, Simulation Lab, Conferences, Lectures given to residents, PALS, ATLS, Prep E-med/CME 1. Acquire knowledge regarding the etiology and natural history of common pediatric emergencies and urgencies. 2. Know potential complications of common pediatric procedures. Interpersonal and Communication skills: Evaluation Tools: 360 Multisource assessment, Patient satisfaction and phone follow-up surveys, Medical Record Review 1. Communicate effectively with patients, families, nursing staff, Emergency Medical Service personnel, ancillary service personnel, referring physicians and consultants. 2. Complete in a timely matter and provide legible and comprehensive medical record documentation. Professionalism: Evaluation Tools: Multisource Assessment (E*value and 360), Professionalism Form by Program Director and Faculty Mentor 1. Follow the standards of behavior established by the Medical University of South Carolina 2. Adhere to the dress code established by the Medical University of South Carolina. 3. Acknowledge the needs of cultural diverse patient populations. Practice-based learning and improvement: Evaluation Tools: QI projects, Journal Clubs and development of treatment guidelines, ILP 1. Focus self education activities on diagnosis and initial management of pediatric problems presenting to the emergency department. 2. Participate in educational activities of the Pediatric Emergency Medicine faculty (didactic lectures, case reviews, Journal Club, simulation lab, Pediatric Emergency Medicine portal and Pediatric Advanced Life Support courses). 3. Become familiar with Pediatric Emergency Department quality improvement activities. 4. Use Pediatric Emergency Medicine faculty as a source for references, information, experience and style. Systems-based practice: Evaluation Tools: SOC assessments, Health care team projects, Patient Safety projects, Administrative/Committee Member 1. Document patient information to promote seamless patient care, accurate billing and a medico-legally sound record. 2. Become familiar with Patient Safety (systems analysis) activities of the Pediatric Emergency Department. 3. Provide situation and age-appropriate injury prevention information and available community injury prevention resources. 4. Provide follow-up communication with referring physicians to gain knowledge in regard to practice types, delivery systems, available resources and the cost and quality of these practice types and systems. 5. Become familiar with the coordination process necessary to implement a research project involving Pediatric Emergency Department patients. Second Year Goals: 1. Assume more of a leadership role in managing Pediatric Emergency Department patients. 2. Provide care to ill and injured children of higher acuity. 3. Prioritize and begin to simultaneously care for multiple patients. 4. Be an effective team member who works efficiently with nurses, ancillary services and consulting physician groups. 5. Supervise and provide bedside teaching to junior residents and medical students. 6. Participate in one or more administrative tasks related to providing Pediatric Emergency care (scheduling, billing, patient satisfaction, quality improvement and implementing research projects). Patient Care: Evaluation tools: Attending direct observation, Press Ganey patient satisfaction surveys/ phonecall ED visit follow-up surveys by nursing staff, Simulation Lab, 360 multisource assessment, Procedure skills documentation and performance in labs 1. Improve ability to independently provide state of the art pediatric emergency management of common pediatric emergencies and urgencies, including, but not limited to: respiratory distress, seizures, cardiac arrhythmias, allergic reactions, toxic ingestions, hypoglycemia, diabetic ketoacidosis, meningitis, appendicitis, pelvic inflammatory disease, intussusception, volvulus, febrile neonate and infant, fever and neutropenia, and testicular torsion. 2. Improve ability to independently perform and supervise common pediatric procedures including, but not limited to: lumbar puncture, simple and complex laceration repair, reduction of commonly dislocated joints, esophageal bougienage, hernia reduction, splinting, intravenous, intraosseous and central venous line placement, tracheal intubation with and without rapid sequence induction/intubation, chest tube placement, cardioversion and procedural sedation. Medical Knowledge: Evaluation tools: Attending direct observation, SITE testing, Simulation Lab, Conferences, Lectures given to residents, PALS, ATLS, Prep E-med/CME 1. Expand knowledge regarding the etiology and natural history of common pediatric emergencies and urgencies. 2. Know alternative methods to common pediatric procedures and the benefits and complications of each so as to be capable of tailoring procedures to the needs of individual patients. 3. Establish self-education habits that assure continued state of the art practice of Pediatric Emergency Medicine Interpersonal and Communication skills: Evaluation Tools: 360 Multisource assessment, Patient satisfaction and phone follow-up surveys, Medical Record Review 1. Communicate effectively with patients, families, nursing staff, Emergency Medical Service personnel, ancillary service personnel, referring physicians and consultants. 2. Complete in a timely matter and provide legible and comprehensive medical record documentation. Professionalism: Evaluation Tools: 360 Multisource assessment, Patient satisfaction and phone follow-up surveys, Medical Record Review 1. Follow the standards of behavior established by the Medical University of South Carolina 2. Adhere to the dress code established by the Medical University of South Carolina. 3. Acknowledge the needs of cultural diverse patient populations. 4. Set an example to junior residents and medical students in regard to professionalism. Practice-based learning and improvement: Evaluation Tools: QI projects, Journal Clubs and development of treatment guidelines, ILP 1. Expand self education activities on diagnosis and initial management of pediatric problems presenting to the emergency department. 2. Organize, lead and improve educational activities of the Pediatric Emergency Medicine faculty (didactic lectures, case reviews, Journal Club, simulation lab, Pediatric Emergency Medicine portal and Pediatric Advanced Life Support courses). 3. Initiate and participate in Pediatric Emergency Department quality improvement activities. 4. Use Pediatric Emergency Medicine faculty as a source for references, information, experience and style. Systems-based practice: Evaluation Tools: SOC assessments, Health care team projects, Patient Safety projects, Administrative/Committee Member 1. Look for opportunities of improving documentation of patient information to promote seamless patient care, accurate billing and a medico-legally sound record. 2. Participate in Patient Safety (systems analysis) activities of the Pediatric Emergency Department. 3. Look for opportunities to improve situation and age-appropriate injury prevention information and making patients aware of available community injury prevention resources. 4. Provide follow-up communication with referring physicians to gain knowledge in regard to practice types, delivery systems, available resources and the cost and quality of these practice types and systems. 5. Participate in the coordination process necessary to implement a research project involving Pediatric Emergency Department patients. Third Year Goals: 1. Assume leadership role in managing Pediatric Emergency Department patients. 2. Provide care to ill and injured children of all levels of acuity. 3. Prioritize and simultaneously care of multiple patients. 4. Be an effective team member who works efficiently with nurses, ancillary services and consulting physician groups. 5. Supervise and provide bedside teaching to junior residents and medical students. 6. Participate in one or more administrative tasks related to providing Pediatric Emergency care (scheduling, billing, patient satisfaction, quality improvement and implementing research projects). Patient Care: Evaluation tools: Attending direct observation, Press Ganey patient satisfaction surveys/ phonecall ED visit follow-up surveys by nursing staff, Simulation Lab, 360 multisource assessment, Procedure skills documentation and performance in labs 1. Progress to independently providing state of the art pediatric emergency management of common pediatric emergencies and urgencies, including, but not limited to: respiratory distress, seizures, cardiac arrhythmias, allergic reactions, toxic ingestions, hypoglycemia, diabetic ketoacidosis, meningitis, appendicitis, pelvic inflammatory disease, intussusception, volvulus, febrile neonate and infant, fever and neutropenia, and testicular torsion. 2. Progress to independently performing and supervising common pediatric procedures including, but not limited to: lumbar puncture, simple and complex laceration repair, reduction of commonly dislocated joints, esophageal bougienage, hernia reduction, splinting, intravenous, intraosseous and central venous line placement, tracheal intubation with and without rapid sequence induction/intubation, chest tube placement, cardioversion and procedural sedation. Medical Knowledge: Evaluation tools: Attending direct observation, SITE testing, Simulation Lab, Conferences, Lectures given to residents, PALS, ATLS, Prep E-med/CME 1. Expand knowledge regarding the etiology and natural history of common pediatric emergencies and urgencies. 2. Know alternative methods to common pediatric procedures and the benefits and complications of each so as to be capable of tailoring procedures to the needs of individual patients. 3. Establish self-education habits that assure continued state of the art practice of Pediatric Emergency Medicine Interpersonal and Communication skills: Evaluation Tools: 360 Multisource assessment, Patient satisfaction and phone follow-up surveys, Medical Record Review 1. Communicate effectively with patients, families, nursing staff, Emergency Medical Service personnel, ancillary service personnel, referring physicians and consultants. 2. Complete in a timely matter and provide legible and comprehensive medical record documentation. 3. Learn communication skills needed to be effective with administrative, media and political leaders. Professionalism: Evaluation Tools: 360 Multisource assessment, Patient satisfaction and phone follow-up surveys, Medical Record Review 1. Follow the standards of behavior established by the Medical University of South Carolina 2. Adhere to the dress code established by the Medical University of South Carolina. 3. Acknowledge the needs of cultural diverse patient populations. 4. Set an example to junior residents and medical students in regard to professionalism. Practice-based learning and improvement: Evaluation Tools: QI projects, Journal Clubs and development of treatment guidelines, ILP 1. Expand self education activities on diagnosis and initial management of pediatric problems presenting to the emergency department. 2. Organize, lead and improve educational activities of the Pediatric Emergency Medicine faculty (didactic lectures, case reviews, Journal Club, simulation lab, Pediatric Emergency Medicine portal and Pediatric Advanced Life Support courses). 3. Participate in Pediatric Emergency Department quality improvement activities. 4. Use Pediatric Emergency Medicine faculty as a source for references, information, experience and style. Systems-based practice: Evaluation Tools: SOC assessments, Health care team projects, Patient Safety projects, Administrative/Committee Member 1. Look for opportunities of improving documentation of patient information to promote seamless patient care, accurate billing and a medico-legally sound record. 2. Participate in Patient Safety (systems analysis) activities of the Pediatric Emergency Department. 3. Look for opportunities to improve situation and age-appropriate injury prevention information and making patients aware of available community injury prevention resources. 4. Provide follow-up communication with referring physicians to gain knowledge in regard to practice types, delivery systems, available resources and the cost and quality of these practice types and systems. 5. Participate in the coordination process necessary to implement a research project involving Pediatric Emergency Department patients. Rotations: Sports Medicine/ Orthopedics Goals: 1. Learn to recognize and manage Peds ED patients with orthopedic injuries or infections. 2. Perform a complete orthopedic examination, including neurovascular status, of an injured extremity. 3. Perform simple reductions: digit dislocations, nursemaid’s elbow, patellar dislocations and shoulder dislocations. 4. Perform arthrocentesis. 5. Gain experience in splinting and other immobilization techniques. Patient Care: 1. Recognize and manage orthopedic infections. 2. Recognize and manage common etiologies of limp: toxic synovitis, HSP, diskitis, toddler’s fracture, physical abuse, osteomyelitis and joint infections, Legg-Calve-Perthes disease, OsgoodSlaughter, slipped capital femoral epiphysis, connective tissue disorders (JRA, Lupus, RA), and Lyme disease. 3. Recognize and manage orthopedic fractures and injuries. Medical Knowledge: 1. Acquire knowledge regarding the etiology and management of common orthopedic injuries, fractures and infections. 2. Explain the anatomic differences between adult and child bones and the types of injuries children sustain Interpersonal and Communication Skills: 1. Describe fractures in regards to angulation and displacement, and communicate findings accurately with a consultant. 2. Coordinate care of patient with consultants including their orthopedic injury and analgesia during injury management. 3. Communicate effectively with family members and patients regarding their injuries and their management. Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with Orthopedic and Sports Medicine residents and faculty to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on common orthopedic injuries and infections. 2. Investigate and discuss controversies in management 3. Participate in educational activities within the Orthopedic Department Systems Based Practice: 1. Document patient information to promote seamless medical care, accurate billing and a medicolegal sound record. 2. Provide and receive information from Orthopedic physicians to coordinate patient’s care. Radiology Goals: 1. Learn indications for medical imaging examinations, including radiographic, ultrasound, nuclear medicine, computed tomography and magnetic resonance procedures. 2. Describe the efficacy of the various medical imaging procedures. 3. Recognize physical abuse with radiographs and communicate those concerns Patient Care: 1. Learn how best to chose the most appropriate imaging examination and imaging procedure for the individual patient Medical Knowledge: 1. Interpret standard chest and abdominal radiographs, and become comfortable diagnosing common chest and abdominal pathology. 2. Be able to interpret CT scans, including head, C-spine, abdomen, sinuses and eye. Interpersonal and Communication Skills: 1. Coordinate care of patient with Radiological consultants including their imaging interpretation and management based on that imaging. 2. Communicate effectively with family members and patients regarding their imaging results and their management Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with Radiology residents and faculty to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on different radiographic imaging’s advantages and limitations. 2. Research and discuss controversies in imaging and management based on imaging. 3. Participate in educational activities within the Radiology Department. Systems Based Practice: 1. Document patient information to promote seamless medical care, accurate billing and a medicolegal sound record. 2. Provide and receive information from Radiology physicians to coordinate patient’s care. Otolaryngology Goals: 1. Recognize and treat common ENT problems, including, but not limited to: otitis media, otitis externa, septal hematoma, TM perforation, hemotympanum, cholesteotoma, soft palate lacerations, peritonsillar and retropharyngeal abscesses, torticollis, facial paralysis, caustic ingestions, sinusitis, stridor, post-T&A bleeding, adenitis, and inflammatory conditions of the airway, including tracheitis, epiglottitis and laryngotracheobronchitis. 2. Recognize and manage head and neck trauma. Patient Care: 1. Gain experience in management of the above common ENT problems 2. Learn when to obtain a ENT consultant to aid in patient care Medical Knowledge: 1. Learn epistaxis management. 2. Explain tracheostomy care and change pre-existing tracheostomies 3. Learn the management of foreign body removal in the ear, nose, and esophagus Interpersonal and Communication Skills: 1. Coordinate care of patient with ENT consultants 2. Communicate effectively with family members and patients regarding their diagnosis and their management Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with ENT residents and faculty to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on common ENT problems and management. 2. Investigate and discuss controversies in management of common ENT conditions. 3. Participate in educational activities within the Otolaryngology Department. Systems Based Practice: 1. Document patient information to promote seamless medical care, accurate billing and a medicolegal sound record. 2. Provide and receive information from ENT physicians to coordinate patient’s care. Ophthalmology Goals: 1. Learn to recognize and manage common eye injuries, problems and infections 2. Coordinate care and follow up with Ophthalmology physicians. Patient Care: 1. Recognize and manage common eye trauma, including, but not limited to: hypehma, globe penetration, blowout fracture, corneal abrasion or burn, foreign body, lid lacerations and retinal hemorrhage Medical Knowledge: 1. Recognize and manage common eye problems, including, but not limited to: contact lens problems, conjunctivitis, glaucoma, iritis, blocked nasolacrimal duct, periorbital and orbital cellulitis and papilledema. 2. Explain the following techniques: flourescein examination, slit-lamp exam, cycloplegia and lid eversion. Interpersonal and Communication Skills: 1. Coordinate care of patient with Ophthalmology consultants 2. Communicate effectively with family members and patients regarding their diagnosis and their management Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with Ophthalmology residents and faculty to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on common eye problems and management. 2. Investigate and discuss controversies in management of common eye conditions. 3. Participate in educational activities within the Ophthalmology Department. Systems Based Practice: 1. Document patient information to promote seamless medical care, accurate billing and a medicolegal sound record. 2. Provide and receive information from Ophthalmology physicians to coordinate patient’s care. Toxicology Goals: 1. 2. 3. 4. 5. To develop a foundation of toxicology knowledge. Understand common poisonings. To develop knowledge of resources needed to evaluate less common exposures. To develop a high level of comfort in the management of overdose and poisoned patients. To develop an understanding of the role a Poison Center plays in the community. Patient Care: 1. Recognize and appropriately manage known or suspected ingestions 2. Effectively communicate management and prognosis to patients and families 3. Utilize the expertise of the Poison Center to assist in care 4. Initiate treatment or be prepared to treat likely complications of common poisons Medical Knowledge: 1. At the end of the rotation, the fellow will: a. Manage and develop treatment plans for the poisoned patient b. Be knowledgeable of antidotes (indications, doses and complications) c. Recognize indications for gastro-intestinal decontamination d. Recognize the symptomatology and treat the following ingestions: i. Anti-depressants, including SSRI’s, Serotonin syndrome and TCA’s ii. Lithium iii. Barbiturates iv. Phenothiazines v. Phenytoin and other anti-epileptics vi. Opiods vii. Clonidine viii. Toxic alcohols ix. Cocaine x. Amphetamines xi. Hallucinogens xii. Salicylates xiii. Acetaminophen xiv. Iron xv. Hydrocarbons xvi. Caustic ingestions xvii. Organophosphates xviii. Mushrooms/ plants xix. Cyanide and carbon monoxide xx. Digitalis, Beta-blockers and calcium channel blockers xxi. Envenomations: snakes, spiders and scorpions Interpersonal and Communication Skills: 1. Coordinate care of patient with Toxicologists and the Poison Center 2. Communicate effectively with family members and patients regarding their diagnosis and their management Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with consulting residents and faculty to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on common ingestions and management. 2. Investigate and discuss controversies in management. 3. Participate in educational activities of the Toxicology Service Systems Based Practice: 1. Document patient information to promote seamless medical care, accurate billing and a medicolegal sound record. 2. Provide and receive information from Ophthalmology physicians to coordinate patient’s care. 3. Understand the Disaster Preparedness plan (local, state and national) for chemical terrorism/accidental exposures. Emergency Medical Services Goals: 1. Understand the capabilities and limitations of the EMS system, especially as they apply to children 2. Gain first-hand experience of the various aspects of pre-hospital care. 3. Understand the role of the EMS director. 4. Become knowledgeable the foundation of pre-hospital research/evidence-based medicine. 5. Learn the expectations and role of the emergency department in disaster medicine. Patient Care: 1. Accompany EMS personnel during emergency responses in the field 2. Assist in communicating medical issues to patients and families Medical Knowledge: 1. Learn the capabilities (especially in children of the EMS system in regard to resuscitation management of the following: i. respiratory failure ii. cardiac failure iii. cardiopulmonary arrest iv. status epilepticus v. altered mental status vi. life threatening trauma injuries 2. Learn role of EMS in regard to disaster preparedness Interpersonal and Communication Skills: 1. Assist in coordinating patient care between EMS and ED personnel 2. Assist in communicating effectively with family members and patients regarding their pre-hospital assessment and treatment Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with pre-hospital personnel to provide the best care to patients. Practice-Based Learning and Improvement: 1. Investigate and discuss controversies in pre-hospital care, especially for children 2. Participate in educational in activities within EMS Systems Based Practice: 1. Become knowledgeable of the EMS communication systems 2. Become knowledgeable of the educational and certification systems for the various levels of EMS personnel Pediatric Intensive Care Unit Goals: 1. Improve knowledge base regarding ongoing monitoring and care of critical physiology derangements including, but not limited to: increased intracranial pressure, hypotension, respiratory distress/ failure, renal failure, coagulopathy, sepsis/ shock and electrolyte disturbances. 2. Improve knowledge base regarding ongoing monitoring and care of the critically ill pediatric patients injured by trauma and burns. Patient Care: 1. Perform critical care procedures, including, but not limited to: central venous access, tracheal intubation and tube thoracostomy. 2. Perform procedural sedation. 3. Transport of critically ill children within the hospital. Medical Knowledge: 1. Learn post resuscitation for common life threatening illnesses and injuries 2. Participate in end-of-life care and discussions regarding organ donation. 3. Gain knowledge regarding common problems suffered by technology dependent children and become familiar with their management. Interpersonal and Communication Skills: 1. Coordinate care and transfer of patient from ED to PICU and from PICU to ancillary services (radiology, operating room) and/or regular in-patient bed. 2. Communicate effectively with family members and patients regarding their diagnosis and their management Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with PICU residents and faculty to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on critical care illnesses and their management. 2. Investigate and discuss controversies in management of critical conditions. 3. Participate in educational activities within PICU faculty. Systems Based Practice: 1. Become familiar with the unique resource of the PICU in the medical community. 2. Become knowledgeable of the work needed to develop and maintain a PICU referral base (onsite visits to referral physician offices and/ED’s, patient updates and treatment summaries to referral physicians). Trauma Goals: 1. Understand the nature of a team approach to trauma patients. 2. Become adept at thoroughly understanding the importance of the primary and secondary survey. 3. Recognize the difference between the stable and critical trauma victims. Patient Care: 1. Procedures may include but are not limited to: central line, surgical airway, and thorocostomy tube placement. 2. Understand the management guideline differences between blunt and penetrating trauma. 3. Understand the management plans for: orofacial, head, neck, orofacial, chest, extremity and abdominal trauma. 4. Understand the appropriate image modalities when approaching the trauma victim. Medical Knowledge: 1. ATLS certification prior to the rotation. 2. Learn recognition and management of traumatic injuries based on mechanism of injury and presentation Interpersonal and Communication Skills: 1. Coordinate care of patient with Trauma surgery and other subspecialty consultants 2. Communicate effectively with family members and patients regarding their diagnosis and their management Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with residents and faculty of the Trauma Service to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on common traumatic injuries and management. 2. Research and discuss controversies in management of common traumatic conditions. 3. Participate in educational activities within the Trauma Surgery and Pediatric Surgery Department. Systems Based Practice: 1. Document patient information to promote seamless medical care, accurate billing and a medicolegal sound record. 2. Provide and receive information from surgeons and consulting physicians to coordinate patient’s care. 3. Be aware of the spectrum of activities performed by a Trauma service: pre-hospital care, emergency department, intensive care, operating room, in-patient care, rehabilitation, research and injury prevention. Anesthesia Goals: 1. Learn, use and understand the implications of ASA levels, airway scores, NPO guidelines and Mallampatti classifications. 2. Understand the role and risks of RSI. 3. Understand the pharmacology of drugs used during RSI. Patient Care: 1. Perform bag-valve-mask ventilation 2. Perform laryngeal mask airway placement, tracheal intubations and become exposed to techniques for difficult airways. 3. Observe methods of regional anesthesia 4. Effectively counsel and discuss risks and benefits with patients and families Medical Knowledge: 1. Learn pharmacology of different drugs used for RSI and sedation 2. Learn procedures to provide analgesia and anesthesia for individual patients and situations Interpersonal and Communication Skills: 1. Communicate effectively with family members and patients regarding their management plan and how to best provide patient comfort with sedation and analgesia 2. Effectively communicate with the various surgical subspecialties and operating room personnel Professionalism: 1. Follow standards of behavior established by the Medical University of South Carolina 2. Effectively work with Anesthesia and Surgical residents and faculty to provide the best care to patients. Practice-Based Learning and Improvement: 1. Focus self-education on common airway problems and management. 2. Investigate and discuss controversies in airway management. 3. Participate in educational activities within the Anesthesia Department. Systems Based Practice: 1. Document patient information to promote seamless medical care, accurate billing and a medicolegal sound record. 2. Provide and receive information from Anesthesia physicians to coordinate patient’s care. 3. Be knowledgeable of the hospital system for activating emergent anesthesia airway consultation EMERGENCY MEDICINE: Patient Care: 1. Perform an efficient complaint directed history and physical on patients presenting to the ED. 2. Have prompt recognition and appropriate emergency stabilization of the unstable patient. 3. Formulate a comprehensive differential diagnosis. 4. Achieve technical proficiency in procedural skills consistent with level of training. 5. Manage multiple patients simultaneously. Medical Knowledge: 1. Demonstrate a more advanced fund of medical knowledge within emergency medicine. 2. Formulate scientific basis for patient care decisions. Interpersonal and Communication Skills: 1. Present a case succinctly and accurately to colleagues. 2. Effectively and confidently relay all pertinent information to patient and family. 3. Demonstrate appropriate conflict resolution skills. Professionalism: 1. Demonstrate the ability to act as a patient advocate at all times. 2. Demonstrate respect, compassion, and integrity with patients, family, and all staff. 3. Demonstrate respect of patient’s privacy and confidentiality. Practice-Based Learning and Improvement: 1. Demonstrate ability to provide evidence-based medicine to patient care decisions. Systems-Based Practice: 1. Utilize the consultation process appropriately. 2. Provides appropriate medical command to pre-hospital providers.