Building Resilience in Children and Youth Dealing with Trauma
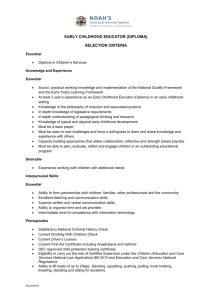
advertisement

Building Resilience in Children and Youth Dealing with Trauma Even from as young as 18 months, children can be affected by traumatic events and have serious problems later in childhood and adulthood. But the great news is that, with help from families, providers, and the community, children and youth can demonstrate resilience when dealing with trauma. Traumatic experiences can range from a one-time incident, such as a sudden death of a loved one or a natural disaster, to ongoing exposure to experiences, such as bullying or family violence. Identifying that a child has experienced trauma is not always easy because emotional and behavioral responses to trauma vary depending on a child’s age, personality, the type and severity of the incident, and availability of adult support. Studies on stress response in children show that there can be physiological and structural changes in the brain and neurological systems and can, without intervention, result in enduring problems such as depression, anxiety, aggression, impulsiveness, delinquency, hyperactivity, and substance abuse. More than 60% of youth age 17 and younger have been exposed to crime, violence and abuse either directly or indirectly. Young children exposed to 5 or more significant adversities in the first 3 years of childhood face a 76 percent likelihood of having one or more delays in their cognitive, language, or emotional development. As the number of traumatic events experienced during childhood increases, the risk for the following health problems in adulthood increases: depression; alcoholism; drug abuse; suicide attempts; heart and liver diseases; pregnancy problems; high stress; uncontrollable anger; and family, financial, and job problems. There is a range of behaviors that could be signs that a child is having difficulty dealing with a traumatic event, such as, but not limited to: Separation anxiety or clinginess towards teachers or caregivers Changes in appetite Decreased interest in and/or withdrawal from friends or family and normal activities Over- or under-reaction to physical contact, sudden movements, and sounds Angry outbursts and/or aggression More frequent complaints of headaches, stomachaches, or fatigue Repeatedly recreating the event through comments, drawings, or activity Emotional “numbing,” or expressing no feelings at all about the event Drop in school performance What can teachers, caregivers, and other adults do to help a child who has experienced trauma? The U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) offers these suggestions: 1 Maintain usual routines Make sure that the child is not being isolated Provide a safe place where the child can talk about the incident Be sensitive to potential environmental cues that may cause a reaction (e.g., an approaching storm or the anniversary of an event) Prepare the child in advance of a change in routine or other event that could be unsettling Monitor what information the child shares with other children to prevent excessive curiosity from peers Nurture the child’s positive self-view Draw on cultural and familiar assets With the support of caring adults, children can recover from traumatic events, reestablish a sense of well-being, and obtain treatment and other services if needed. The more you know about trauma and children, the more you can do to help them. For more resources on early childhood and trauma, visit http://www.samhsa.gov/children/earlychildhood_trauma.asp. April 2011: Childhood Trauma's Impact on Health Risks As the number of traumatic events experienced during childhood increases, the risk for the following health problems in adulthood increases: Depression Alcoholism Drug abuse Suicide attempts Heart, liver, and pulmonary diseases Fetal death during pregnancy High stress Uncontrollable anger Family, financial, and job problems With help from families, providers, and the community, young children can demonstrate resilience when dealing with trauma. As the number of adverse events (i.e., physical, emotional, and sexual abuse; neglect; violence; and natural disasters) experienced in childhood increases, the risk for the following health problems increases: depression; alcoholism; drug abuse; suicide attempts; heart, liver, and pulmonary diseases1; fetal death during adolescent pregnancy; high stress; uncontrollable anger; and family, financial, and job problems.2,3 The effects of these events are long-term, powerful, cumulative, and may be invisible to health care providers, educators, social service organizations, and policymakers because the linkage between trauma and problems later in adulthood is concealed by time, the inability to “see” the process of neurodevelopment, and the effects of the original traumatic events, which may not become evident until much later in life.4 2 Research has shown that caregivers can buffer the impact of trauma and promote better outcomes for children even under stressful times when the following Strengthening Families Protective Factors5 are present: Parental resilience Social connections Knowledge of parenting and child development Concrete support in times of need Social and emotional competence of children Text description of this chart is available on a separate page. 3 Text description of this chart is available on a separate page. 4 Text description of this chart is available on a separate page. For more information on the impact of adverse childhood experiences, please visit http://www.cdc.gov/ace/index.htm . 1. Felitti, V.J., Anda, R.F., Nordenberg, D., Williamson, D.F., Spitz, A.M., Edwards, V., Koss, M.P., & Marks, J.S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study, American Journal of Preventive Medicine, 14 (4), 245-258. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9635069?dopt=Abstract . 2. Hillis, S.D., Anda, R.F., Dube, S.R., Felitti, V.J., Marchbanks, P.A., & Marks, J.S. (February 2004). The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial outcomes, and fetal death. Pediatrics,113(2), 320– 327. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/14754944?dopt=Abstract . 3. Anda, R.F., Felitti, V.J., Fleisher, V.I., Edwards, V.J., Whitfield, C.L., Dube, S.R., & Williamson, D.F. (2004). Childhood abuse, household dysfunction and indicators of impaired worker performance in adulthood. The Permanente Journal, 8(1), 30–38. 4. Perry, B.D. (2009). Examining child maltreatment through a neurodevelopmental lens: clinical application of the Neurosequential Model of Therapeutics. Journal of Loss and Trauma, 14, 240-255. 5. Horton, C. (2003). Protective factors literature review. Early care and education programs and the prevention of child abuse and neglect. Center for the Study of Social Policy. Retrieved from http://strengtheningfamilies.net/images/uploads/pdf_uploads/LiteratureReview.pdf (PDF). Graphs were created by the Center on the Developing Child at Harvard University from the cited articles and are used by permission. For more information from the Center about early childhood development, please visit http://www.developingchild.harvard.edu . Dube, S.R., Anda, R.F., Felitti, V.J., Edwards, V.J., & Croft J.B. (2002). Adverse childhood experiences and personal alcohol abuse as an adult, Addictive Behaviors 2002;27(5):713–725. Retreived from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list _uids=12201379 . Dube, S.R., Felitti, V.J., Dong, M., Chapman, D.P., Giles, W.H., & Anda, R.F. (March 2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The Adverse Childhood Experiences Study. Pediatrics, 111(3), 564-572. Chapman, D.P., Whitfield, C.L., Felitti, V.J., Dube, S.R., Edwards, V.J., & Anda, R.F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217–225. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list _uids=15488250 . 5 Dong, M., Giles, W.H., Felitti, V.J., Dube, S.R., Williams, J.E., Chapman, D.P., & Anda, R.F. (2004). Insights into causal pathways for ischemic heart disease: adverse childhood experiences Study. Circulation, 110(13),1761–1766. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list _uids=15381652 . Use these sample messages to share this early childhood trauma and resilience data point with your connections on Twitter and Facebook and via email. Twitter: More trauma in childhood = increased risk for serious #health issues in adulthood. Which ones? Read: http://1.usa.gov/eXqVRX via @samhsagov #1in5 Facebook: Research shows that more traumatic experiences in childhood increases the risk for serious health problems in adulthood. Learn more about childhood trauma’s impact on health risks in adulthood and pass it on to observe National Children’s Mental Health Awareness Day: http://1.usa.gov/eXqVRX March 2011: Childhood Trauma's Impact on a Child's Developing Brain Studies on the brain show that physical, emotional, or sexual abuse in childhood can: cause permanent damage, reduce the size of parts of the brain, impact the way a child's brain copes with daily stress, and can result in enduring behavioral health problems such as depression, anxiety, aggression, impulsiveness, delinquency, hyperactivity, and substance abuse. With help from families, providers, and the community, young children can demonstrate resilience when dealing with trauma. New brain imaging surveys and other techniques show that physical, emotional, or sexual abuse in childhood (as well as stress in the form of exposure to violence, warfare, or famine) can cause permanent damage to the neural structure and function of the developing brain. In addition to the implications outlined in the data point above, traumatic or stressful experiences can lead to conditions such as borderline personality disorder, dissociative episodes, hallucinations, delusions, psychosis, paranoia, anger outbursts, and impaired attention. Whether in the form of physical, emotional or sexual trauma, or exposure to warfare or famine, stress can set off a ripple of hormonal changes and key brain alterations that may be irreversible.1 However, research has shown that caregivers can buffer the impact of trauma and promote better outcomes for children even under stressful times when the following Strengthening Families Protective Factors2 are present: 6 Parental resilience Social connections Knowledge of parenting and child development Concrete support in times of need Social and emotional competence of children Trauma Data Source: 1. Teicher, M.H. (2002). Scars that won't heal: The neurobiology of child abuse. Scientific American. 68-75. (Retrieved from http://www.icscommunitynetwork.org/scarsthatwon_theal+.pdf [PDF - 295 KB]). 2. Horton, C. (2003). Protective factors literature review. Early care and education programs and the prevention of child abuse and neglect. Center for the Study of Social Policy. (Learn more at www.strengtheningfamilies.net ) Use these sample messages to share this early childhood trauma and resilience data point with your connections on Twitter and Facebook and via email. Twitter: Physical, emotional or sexual abuse in childhood can impact a child's developing brain. Find out how: http://1.usa.gov/faK4p1 via @samhsagov #1in5. Facebook: Studies on the brain show that physical, emotional, or sexual abuse in childhood can impact a child's developing brain. Learn more about childhood trauma's impact on childhood development and pass it on to observe National Children's Mental Health Awareness Day: http://1.usa.gov/faK4p1 7