Maxillofacial Trauma Case 1: 48y male, intoxicated Fell striking
advertisement

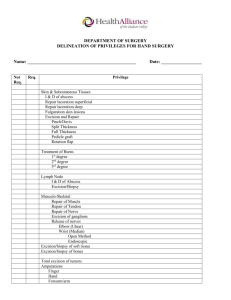
Maxillofacial Trauma Case 1: 48y male, intoxicated Fell striking cheek on the bar Laceration to anterior cheek Through-and-through Q: How to anesthetize? Local infiltration Infraorbital nerve block Q: How to repair? 1) Absorbable to buccal mucosa 2) Absorbable to muscle layer 3) Nonabsorbable to skin Q: Antibiotics? No Yes Case 2: 18y hockey player “Too good” to wear a face mask High stick to the face Upper lip laceration Crosses vermillion border Involves muscular layer Q: How to anesthetize? Infraorbital nerve block (or mark vermillion border and locally infiltrate) Q: How to repair? Vermillion border first Absorbable to muscle/lip mucosa Q: Antibiotics? No Yes Case 3: 25y female MVC, ejected Intubated by STARS on scene Swelling facial and periorbital Extensive abrasions to forehead with gravel/glass in wound Q: One bedside test you need to do? Tonometry Q: Management if test is abnormal? Lateral canthotomy/cantholysis (IOP > 40) Q: Treatment for her abrasions? Vigorous scrubbing to avoid tattooing Can use topical lidocaine Case 4: It’s June 28, 1997 35y male boxer Lac to right ear during fight Through cartilage Claims he was bitten Opponent says it was a punch Case 5: 12y female Skateboarding for the first time Fell Caught tongue between teeth Tongue laceration (V1 block) Q: How to anesthetize? Ear field block Q: How to repair? 6-0 absorbable to cartilage 5-0 nonabsorbable to skin Compression dressing Q: Antibiotics? No Yes Q: Indications for tongue lac repair? Q: How to anesthetize? Inferior alveolar/lingual nerve block or 4% topical lidocaine Q: How to repair? 4-0 absorbable or black silk Q: Antibiotics? No Yes Indications for tongue laceration repair (controversial) (emedicine, EM Clinics of North America, Roberts & Hedges, Rosen) Midline Need hemostasis Maxillofacial Trauma Large flap (>1cm or gaping) Avulsion/amputation Nonlinear laceration or U-shaped Other questions to review if time permits: Q) What are indications for abx in facial trauma Bite wound Devascularized tissue Through-and-through buccal mucosa Cartilage involvement (nose/ear) Extensive contamination Open # # into sinus # with CSF leak Q) What is appropriate mgmt of pediatric peri-oral electrical burns? Perioral burns Can result in severe cosmetic issues and microstomia Trivial looking initial wound may progress over days 5-21 days post-burn get eschar separation and can have lift-threatening labial artery bleeding NEED TO D/W plastics in the ED! o Can d/c home with close watching and F/U ENT/plastics if not extensive initially o Options: early surgery, oral splinting, delayed surgery Q) Management of subperichondral hematoma? Risk factor for cauliflower ear Needs needle aspiration, compressive dressing and R/A in 24hrs to ensure hematoma has not re-accumulated Q) Describe appropriate ED management of eyelid lacerations. Superficial lacs can be repaired with 6-0 Ethilon Lid margin, canalicular, lacrimal involvement need ophtho/plastics Maxillofacial Trauma Case 6: It’s 0100 Dude and his girlfriend come in She was “yawning” and mouth got stuck open Case 7: 16y male Tough guy Punched in the nose Swelling to nasal bridge Crooked nose? Hard to tell… Case 8: 22y female Squash player Hit in eye by ball Diplopia on up-gaze CT shows orbital floor blowout # without entrapment of EOM Case 9: Same polytrauma as Case 3 Still intubated Bleeding into oropharynx & nasopharynx from ? You think her face is mobile Case 10: 35y female, fell down stairs Teeth don’t fit right Neck pain, no c=spine # No other injuries Q: What does she have? TMJ dislocation Q: How will you fix it? Thumbs in buccal recess Push down, rotate chin up, push mandible posteriorly Q: F/U plans? Oral surgery if recurrent Q: One thing on physical exam that you need to rule-out? Nasal septal hematoma Q: Management of that thing if you find it? Incision, expression of clot, anterior packing, R/A in 24hrs Q: Investigations? None (x-rays useless) Q: ED management and F/U? Analgesia, reduce if really crooked F/U plastics in 7-10 days for R/A Q: How does true EOM entrapment present? Vagal tone, vomiting Refusal to move eye Q: Why does she have diplopia? V2 neurapraxia, fat entrapment, intramuscular hematoma Q: Mgmt of her fracture? Analgesia (can D/W plastics) F/U plastics in 7-10 days Q: Describe the Le Fort classification system? See next page Q: Management of her bleeding? Anterior packs Pack naso/oro-pharynx around ETT Reduce Le Fort +/-Interventional radiology Q: What % of mandible # have associated Cspine #? 10% Q: Investigations? Panorex or CT mandible Q: Management/disposition? Consult plastics or maxillofacial sx Maxillofacial Trauma LeFort I – maxilla II – nasal bridge, lacrimal bones, orbital floor, orbital rim, maxilla III – craniofacial dysjunction (rare to get pure III); nasal bridge, ethmoids, maxilla, lateral orbital wall, zygomatic arch