NANCY LEFEBER HUGHES, M.D.
Internal Medicine Associate
1515 Tremont – Galveston, Texas 77550
(409) 771-2040
__________________________________________
Name
Date
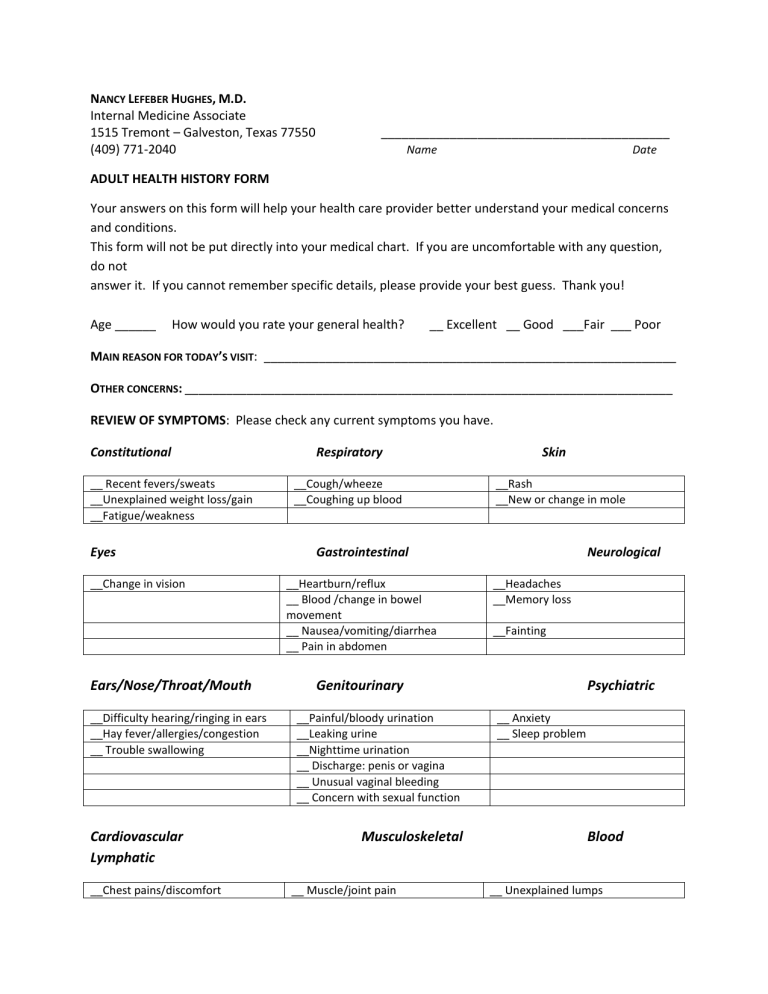
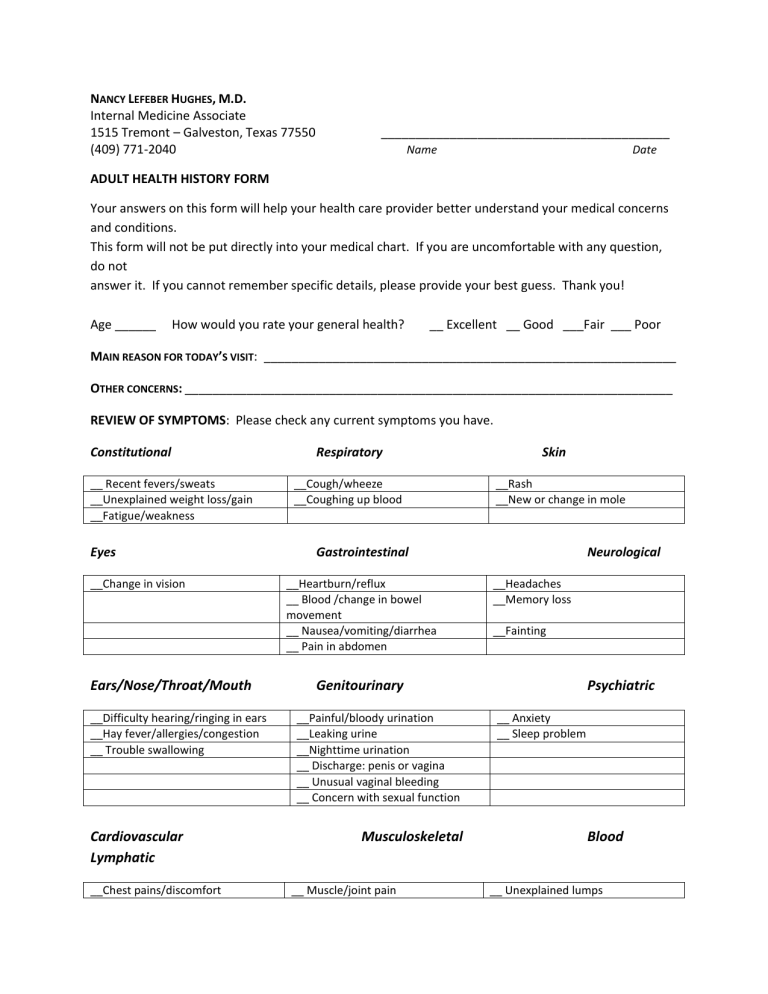
ADULT HEALTH HISTORY FORM
Your answers on this form will help your health care provider better understand your medical concerns
and conditions.
This form will not be put directly into your medical chart. If you are uncomfortable with any question,
do not
answer it. If you cannot remember specific details, please provide your best guess. Thank you!
Age ______
How would you rate your general health?
__ Excellent __ Good ___Fair ___ Poor
MAIN REASON FOR TODAY’S VISIT: ____________________________________________________________
OTHER CONCERNS: _______________________________________________________________________
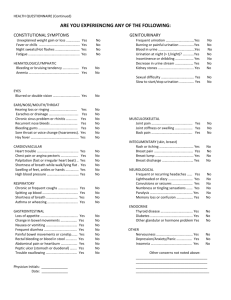
REVIEW OF SYMPTOMS: Please check any current symptoms you have.
Constitutional
__ Recent fevers/sweats
__Unexplained weight loss/gain
__Fatigue/weakness
Eyes
__Change in vision
Ears/Nose/Throat/Mouth
__Difficulty hearing/ringing in ears
__Hay fever/allergies/congestion
__ Trouble swallowing
Cardiovascular
Lymphatic
__Chest pains/discomfort
Respiratory
__Cough/wheeze
__Coughing up blood
Skin
__Rash
__New or change in mole
Gastrointestinal
__Heartburn/reflux
__ Blood /change in bowel
movement
__ Nausea/vomiting/diarrhea
__ Pain in abdomen
Neurological
__Headaches
__Memory loss
__Fainting
Genitourinary
__Painful/bloody urination
__Leaking urine
__Nighttime urination
__ Discharge: penis or vagina
__ Unusual vaginal bleeding
__ Concern with sexual function
Musculoskeletal
__ Muscle/joint pain
Psychiatric
__ Anxiety
__ Sleep problem
Blood
__ Unexplained lumps
__Palpitations
__Short of breath with exertion
__Recent back pain
Breast
__ Breast lump
__Nipple discharge
__ Easy bruising/bleeding
Endo
__ Cold/heat intolerance
__Increase thirst/appetite
HAVE YOU RECENTLY HAD LITTLE INTEREST OR PLEASURE IN DOING THINGS, OR FELT DOWN, DEPRESSED OR HOPELESS?
___ YES ___ NO
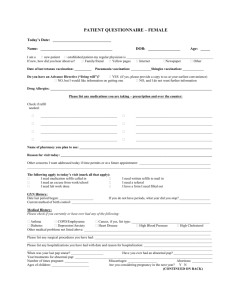
MEDICATIONS:
List Prescription and non-prescription medicines, vitamins, home remedies, birth control pills herbs, etc.
Medication
Dose (e.g., Mg. /pill)
How many times/day
ALLERGIES OR REACTIONS TO MEDICATIONS:
_________________________________________________________
DATE OF YOUR MOST RECENT IMMUNIZATIONS:
Hepatitis A _____ Hepatitis B _____ Influenza (flu shot) _____ MMR _____ Pneumovax (pneumonia)
_____
Meningitis _____ Tetanus (Td) _____ Varicella (chicken pox) shot or illness ____ Tdap (tetanus &
pertussis) ____
HEALTH MAINTENANCE SCREENING TESTS:
LIPID (CHOLESTEROL) DATE: _____ ABNORMAL? __YES __NO
SIGMOIDOSCOPY OR COLONOSCOPY DATE: _______ ABNORMAL? __YES __NO
WOMEN: MAMMOGRAM DATE: _____ ABNORMAL? __YES __NO PAP SMEAR DATE: _____ ABNORMAL? __YES
__NO
DEXASCAN (OSTEOPOROSIS) DATE: _____ ABNORMAL? __YES __NO
MEN: PSA (PROSTATE) DATE: _____ ABNORMAL? __YES __NO
PERSONAL MEDICAL HISTORY: Please indicate whether you have had any of the following medical
problems (with dates)
___Heart disease:
___ High blood pressure
___High cholesterol
specify type ____________________
___Diabetes
___Thyroid problem
___Asthma/Lung disease
___Other (specify) _____________________________
___Kidney disease
___Cancer (specify) ___________________________
SURGICAL HISTORY: Please list all prior operations (with dates)
_________________________________________________________________________________________________________________
_________________________________________________________________________________________________________________
FAMILY HISTORY: Please indicate the current status of your immediate family members:
Please indicate family members (parent, sibling, grandparent, aunt or uncle) with any of the
following conditions.
Alcoholism__________________________________________
High cholesterol _________________________________
Cancer, specify type ________________________________
High blood pressure _____________________________
Heart disease________________________________________
Stroke ____________________________________________
Depression/suicide ________________________________
Bleeding or clotting disorder___________________
Genetic disorders __________________________________
Asthma/COPD ___________________________________
Diabetes ____________________________________________
Other _____________________________________________
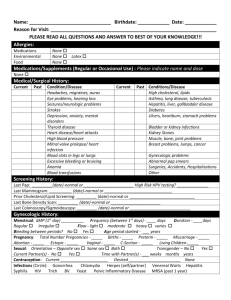
Social History:
OTHER CONCERNS
Tobacco Use
Caffeine Intake: __ none __Cigarettes __Never
__Quit date ___________
Coffee/tea/soda ______ cups/day
Current smoker: Packs/day _______# of yrs. _____
Weight: Are you satisfied with your weight? ____
Are you interested in quitting? ___________________________
Diet: How do you rate your diet? _ Good _ Poor __
Alcohol Use
Do you eat or drink 4 servings of dairy or soy
Do you drink alcohol? ___No ___Yes #drinks/wk. ___
daily or take calcium supplements? __ No __ Yes
Is your alcohol use a concern for others? __No __ Yes
Exercise: Do you exercise regularly? __ No __ Yes
Drug Use
What kind of exercise? ____________________________
Do you use any recreational drugs? ___No ___ Yes
How long (minutes) _____ How often? ___________
Have you ever used needles to inject drugs? ___No ___Yes
If you do not exercise, why? _____________________
Sexual Activity
Safety: Do you use a bike helmet? ___ No ___Yes
Sexually active ___ Yes ___ No ___ Not currently
Do you use seatbelts consistently? ___ No ___ Yes
Current sex partner(s) is/are: ___ Male ___Female
Is violence at home a concern to you __ No __ Yes
Birth control method ___________________ __ None needed
Have you ever been abused? ____ No ___ Yes
Have you ever had any sexually transmitted diseases?
Have you had a gun in your home? ___ No ___ Yes
STDS? ____ Yes ____No
Are you interested in being screened for sexually transHave you completed a living will or durable
mitted diseases? ___ No ___ Yes
power of attorney for health care?___ No ___ Yes
Socioeconomics Occupation: _____________________ Employer: ______________________________________________________
Years of education/highest degree: ____
Marital status: Single ___ Partner/Married ___ Divorced ___ Widowed ____ Other ____________
Number of children/ ages: _______________________________________________________________________________________________
Who lives at home with you? ____________________________________________________________________________________________
WOMEN’S HEALTH HISTORY # of pregnancies ______ # deliveries ____# abortions ____ # miscarriages _______
Age at start of periods: ___________________
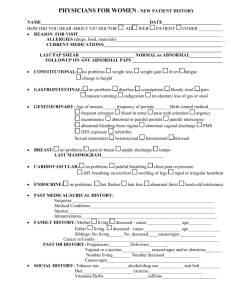
Please check all conditions you currently have or have had and describe complications:
General questions:
Cardiovascular
Angina
Chest pain
Murmurs
Leg cramps
Kidneys & Urinary Tract
Blood in urine
Brown urine
Dribbling after urination
Painful urination
Musculoskeletal
Anemia
Arthritis
Back pain
Bursitis
Excessive thirst
Gout
Anxiety
Waking at night short of
breath & getting out of
bed.
Ankle swelling
Joint aches
Headaches
Cardiac Catheterization
Depression
Cold hands or feet
Meningitis
Congenital heart
defects
Dizziness when standing
up quickly
Heart attacks
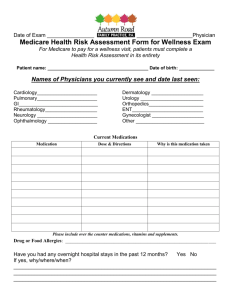
Involuntary
urination/incontinence
Frequent urination
(day)
Frequent urination
(night)
Urinary hesitancy
Weak flow
Easy bleeding
Frequent bladder
infections
Kidney disease
Kidney stone
Easy bruising
Endocrine
Diabetes
Sickle cell
Muscle aches
Gastrointestinal
Diarrhea
Abnormal body hair
Changes in skin texture
Cold intolerance
Reflux
Gallstones
Ulcers
Pleurisy – Wheezing
Heat intolerance
Heartburn
Asthma
History of “borderline”
diabetes
Increased hair loss
Hepatitis
Rheumatism
Black tarry stools
Thyroid disease
Vomiting blood
Constipation
Nausea
Weight loss
Weight gain
Change in sleep patterns
Change in activity
capacity
Neurologic &
Psychiatric:
Paralysis
Seizure
Stroke
Tingling
Tremors
Memory loss
Fainting spells
Dizziness
Head injuries
Black outs or near
blackouts
Change in sensation
anywhere in body
Localized weakness or
numbness
Ears, Eyes, Nose &
Throat
Hay fever
Glaucoma
Polyps
Heart failure
High or low blood
pressure
Irregular heart beat
Purple fingers or lips
Leg pain that resolves
with rest
Heart palpitations
Varicose veins
Respiratory
Breathlessness when
lying flat
Prolonged cough
Coughing up blood
Emphysema
Abnormal blood counts
Blood clots in legs/lungs
Bone Marrow Biopsy
Joint swelling
Morning stiffness
Anal fissures
Allergy
Cataracts
Shortness of breath
Tuberculosis
Male & Female
Painful sexual
intercourse
Loss of sexual interest
Unprotected sex
Problems swallowing
Hiatal hernia
Goiter
Hoarseness
Double vision
Gum problems
Pneumonia
Frequent infections
(bronchitis)
Skin
Abscess
Groin itching
Sexually transmitted
diseases
Males only
Hernia
Sterility
Hemorrhoids
Red blood after bowel
movements
Females Only
D&C
Hot flashes
Eye problems
Ear infections
Glasses/contacts
Acne – Oily skin
Dandruff
Boils – Rashes
Hearing loss
Ear discharge/pain
Hives
Dry skin/Psoriasis
Hernia
Fibroids
Jaundice
Bloody ejaculation
Inability to complete
intercourse
Lump on testicle
Frequent nosebleeds
Ringing in your ears
Athlete’s foot
Penile discharge
Sinus infections
Swollen glands
Excessive body odor
Excessive sweating
Fungal infections
Premature ejaculation
Problems maintaining
or keeping an erection
Prostate disease
Nail problems
Moles – irregular
Sores on penis or warts
Testicular pain
Moles – change/new
Testicular swelling
Provider notes:
Intestinal Obstruction
Liver disease
Abnormal bleeding
between cycles
Complications with
pregnancy
PMS - Endometriosis
Heavy bleeding during
cycles
Discharge from breast
Ovarian cysts
Pelvic Inflammatory
Disease
Postmenopausal
symptoms
Vaginal discharge
Vaginal dryness
Vaginal warts