Adult-EmergenciesSIMDraft
advertisement
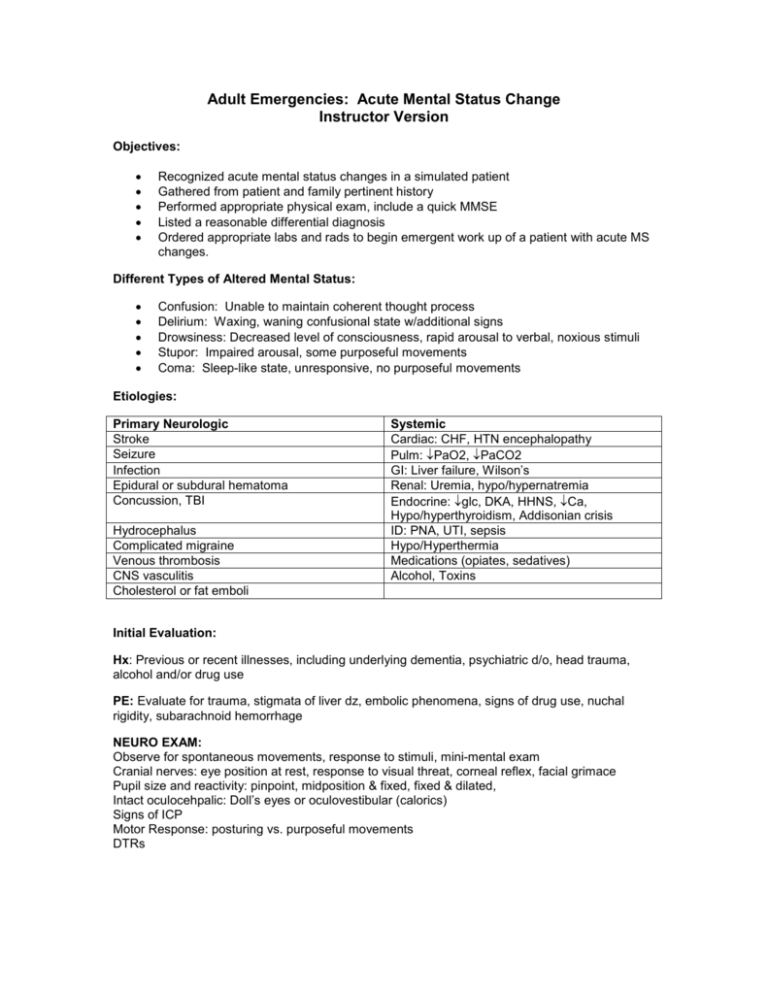
Adult Emergencies: Acute Mental Status Change Instructor Version Objectives: Recognized acute mental status changes in a simulated patient Gathered from patient and family pertinent history Performed appropriate physical exam, include a quick MMSE Listed a reasonable differential diagnosis Ordered appropriate labs and rads to begin emergent work up of a patient with acute MS changes. Different Types of Altered Mental Status: Confusion: Unable to maintain coherent thought process Delirium: Waxing, waning confusional state w/additional signs Drowsiness: Decreased level of consciousness, rapid arousal to verbal, noxious stimuli Stupor: Impaired arousal, some purposeful movements Coma: Sleep-like state, unresponsive, no purposeful movements Etiologies: Primary Neurologic Stroke Seizure Infection Epidural or subdural hematoma Concussion, TBI Hydrocephalus Complicated migraine Venous thrombosis CNS vasculitis Cholesterol or fat emboli Systemic Cardiac: CHF, HTN encephalopathy Pulm: PaO2, PaCO2 GI: Liver failure, Wilson’s Renal: Uremia, hypo/hypernatremia Endocrine: glc, DKA, HHNS, Ca, Hypo/hyperthyroidism, Addisonian crisis ID: PNA, UTI, sepsis Hypo/Hyperthermia Medications (opiates, sedatives) Alcohol, Toxins Initial Evaluation: Hx: Previous or recent illnesses, including underlying dementia, psychiatric d/o, head trauma, alcohol and/or drug use PE: Evaluate for trauma, stigmata of liver dz, embolic phenomena, signs of drug use, nuchal rigidity, subarachnoid hemorrhage NEURO EXAM: Observe for spontaneous movements, response to stimuli, mini-mental exam Cranial nerves: eye position at rest, response to visual threat, corneal reflex, facial grimace Pupil size and reactivity: pinpoint, midposition & fixed, fixed & dilated, Intact oculocehpalic: Doll’s eyes or oculovestibular (calorics) Signs of ICP Motor Response: posturing vs. purposeful movements DTRs Treatment: Control airway, monitor VSs, IV access C-spine precautions, increase HOB if ICP or herniation suspected, hyperventilation, dexamethasone, neurosurgical consult Give thiamine (before dextrose in case of Wernicke’s), dextrose, naloxone, flumazenil Diagnostic Studies: Head CT, MRI CXR, C-spine CBC, ESR, electrolytes, BUN, Cr, ABG, LFTs, coags, tox screen, TSH, VDRL, B12, folate, UA, UDS Lumbar puncture EKG, EEG Glasgow Coma Score Eye Opening Best Verbal Response Spontaneous To Voice To Painful stimuli None Oriented Confused Inappropriate words Unintelligible words None Causes of Metabolic Acidosis M: Methanol U: Uremia D: DKA P: Paraldehyde I: Infeciton L: Lactic Acidosis E: Ethylene gylcol S: Salicylates AEIOUM&MTIPS A: Alcohol E: Epilespy (esp post-ictal) I: Insulin O: Overdose, oxygenation (lack of) U: Uremia, underdose M: Myocardial &: Anesthesia M: Metabolic T: Trauma, fracture I: Infection P: Psych, poisoning S: Stroke, shock Best Motor Response Follows commands Localizes pain Withdraws from pain Flexor response Extensor response None Points 6 5 4 3 2 1 Adult Emergencies: Altered Mental Status Objectives: Recognized acute mental status changes in a simulated patient Gathered from patient and family pertinent history Performed appropriate physical exam, include a quick MMSE Listed a reasonable differential diagnosis Ordered appropriate labs and rads to begin emergent work up of a patient with acute MS changes. Different Types of Altered Mental Status: Confusion: Delirium: Drowsiness: Stupor: Coma: Etiologies: Primary Neurologic Stroke Systemic Cardiac: Seizure Pulm: Infection GI: Epidural or subdural hematoma Renal: Concussion, TBI Endocrine: Hydrocephalus Complicated migraine Venous thrombosis CNS vasculitis Cholesterol or fat emboli ID: Hypo/Hyperthermia Medications (opiates, sedatives) Alcohol, Toxins Initial Evaluation: Hx: Previous or recent illnesses, including underlying dementia, psychiatric d/o, head trauma, alcohol and/or drug use PE: Evaluate for trauma, stigmata of liver dz, embolic phenomena, signs of drug use, nuchal rigidity, subarachnoid hemorrhage NEURO EXAM: Observe for spontaneous movements, response to stimuli, mini-mental exam Cranial nerves: eye position at rest, response to visual threat, corneal reflex, facial grimace Pupil size and reactivity: pinpoint, midposition & fixed, fixed & dilated, Intact oculocehpalic (‘doll’s eyes’) or oculovestibular (calorics) Signs of ICP Motor Response: posturing vs. purposeful movements DTRs Treatment: Control airway, monitor VS, IV access C-spine precautions, increase HOB if ICP, herniation suspected, hyperventilation, dexamethasone, neurosurgical consult Give thiamine (before dextrose in case of Wernicke’s), dextrose, naloxone, flumazenil Diagnostic Studies: Head CT, MRI CXR, C-spine CBC, ESR, electrolytes, BUN, Cr, ABG, LFTs, coags, tox screen, TSH, VDRL, B12, folate, UA, UDS Lumbar puncture EKG, EEG Glasgow Coma Score Eye Opening Best Verbal Response Spontaneous To Voice To Painful stimuli None Oriented Confused Inappropriate words Unintelligible words None Causes of Metabolic Acidosis M: Methanol U: Uremia D: DKA P: Paraldehyde I: Infection L: Lactic Acidosis E: Ethylene gylcol S: Salicylates AEIOU M&M TIPS A: Alcohol E: Epilespy I: Insulin O: Overdose, oxygenation U: Uremia, underdose M: MI &: Anesthesia M: Metabolic T: Trauma I: Infection P: Psych, poisoning S: Stroke, shock Best Motor Response Follows commands Localizes pain Withdraws from pain Flexor response Extensor response None Points 6 5 4 3 2 1