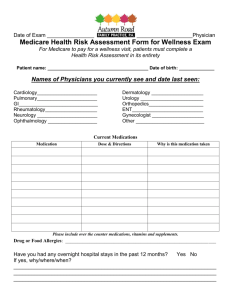
associates in primary care medicine, inc.
advertisement

1 ASSOCIATES IN PRIMARY CARE MEDICINE, INC. An Annual Wellness Visit at our facility is not a regular office visit. It is a special office visit where the goal is to be sure we understand your special needs and assess your health maintenance status to be sure you receive the right care and resources. Please complete this questionnaire before your visit so we can make the most of this visit. Please understand that this is NOT to address new problems nor to provide routine care for chronic problems, provide medication refills, or to check routine lab studies. Those issues are addressed at a separate regular office visit. We are providing you a list of your medications from our file. Please update the list and bring it to your wellness visit. Please include all of the vitamins, supplements, and other OTC (over the counter) medications that you take. Please update this list as well and bring it to your appointment. Please arrive at least 15 minutes before your scheduled appointment time. Thank you. PATIENT NAME: ____________________________ DOB: ________________ APPOINTMENT DATE AND TIME: ______________________________________ Please circle your answers Home Environment: Private home, Assisted Living, Other: _________________________________ Diet and Nutrition: healthy diet , diet is high in salt , high caloric intake , high carbohydrate meals , ___________________________________________ Fracture Risk: fractures , no history of fractures , no previous musculoskeletal injuries , diet is high in fat, low in fiber , low calcium intake Additional Notes: no recent explained fracture , history of fractures , sudden unexplained fractures , previous musculoskeletal injuries Additional Notes: ____________________________________________________________ no sudden unexplained recent explained fracture , 2 Physical Activity: exercises on a regular basis , physical condition , does not exercise on a regular basis , physical condition , deconditioned due to sedentary lifestyle recent increase in physical activity , good decreased physical activity , poor Additional Notes: __________________________________ 1 Mental Status: never feels sad, empty, or tearful , significant changes in weight , energy , energy , no loss of interest in activities , no sleep disturbances or insomnia , no feelings of worthlessness or guilt , significant changes in weight , sleep disturbances or insomnia , Orientation: loss of interest in activities , agitated , thoughts of suicide , loss of history of mood disorders , no disorientation to date , disorientation to time , disorientation to date , _______________________________________________ no decreased concentrating ability , does not forget words , decreased concentrating ability , words Additional Notes: _________________________ Speech/Motor difficulties: no history of depression , Additional Notes: ____________________________________ no disorientation to time , Concentration and Memory: no loss of no thoughts of suicide , feels sad, empty, or tearful , history of depression no disorientation to place , disorientation to place Additional Notes: no memory lapses or loss , memory lapses or loss , no speech difficulties , no difficulty with fine manipulative tasks , time , no agitation , no history of mood disorders , feelings of worthlessness or guilt , no forgetting no difficulty expressing formulated concepts , no difficulty writing/copying , does not knock things over when trying to pick them up , speech difficulties , no slowed reaction difficulty 3 expressing formulated concepts , difficulty with fine manipulative tasks , slowed reaction time , _________________________________ difficulty writing/copying , knocking things over when trying to pick them up Additional Notes: 1 Hearing: no loss of hearing , fluctuating , loss of hearing in one ear only , getting progressively worse , requires TV, radio at high volume , loss of hearing: in both ears , difficulty hearing over background noise , tone deafness , Additional Notes: _______________________________________________ Vision: no vision problems , worse with distance , images with fatigue , total vision loss , worse both distance and near , blind spot(s) , briefly vision loss , worse near , sudden partial vison loss , increased sensitivity to glare , blurred vision worsening , difficulty seeing in bright light , seeing double slow partial vision loss , worsening depth perception , Additional Notes: ________________________ Activities of Daily Living: able to bathe with limited or no assistance , able to dress with limited or no assistance , to get out of chair or bed with limited or no assistance , toilet with limited or no assistance , able to feed self with limited or no assistance , able to groom with limited or no assistance , unable to bathe without assistance , unable to control urination and bowels , able to control urination and bowels , able to unable to dress without assistance , unable to feed self without assistance , of chair or bed without assistance , unable to groom without assistance , Additional Notes: _________________________________________________________________ able unable to get out unable to toilet without assistance 4 Instrumental Activities of Daily Living: able to do house work with limited or no assistance , shop with limited or no assistance , able to manage medications with limited or no assistance , money with limited or no assistance , able to manage able to prepare meals with limited or no assistance , with limited or no assistance , assistance , able to grocery unable to do house work without assistance , unable to manage medications without assistance , able to use the phone unable to grocery shop without unable to manage money without assistance , unable to prepare meals without assistance , unable to use the phone without assistance Additional Notes: ____________________________________________ Falls Risk Assessment: last visit , fear of falling , no frequent falls while walking , no fall in the past year , no dizziness/vertigo , frequent falls while walking , injury with fall Additional Notes: ___________________ Home Safety: no unsafe flooring hazards , appliances , working smoke/CO detectors , use of seatbelts , no unsafe stairs , no unsafe gas no vision or hearing loss while driving , has hand bars in the bathroom/shower , good lighting in the home , unsafe gas appliances , protective head gear for biking/high velocity , dizziness/vertigo , wears protective head gear for biking/high velocity , practicing 'safer sex' , unsafe flooring hazards , no fall since unsafe stairs , no smoke/CO detectors , does not use seatbelts , vision or hearing loss while driving , no fire arms , fire arms , does not wear not practicing 'safer sex' , does not have hand bars in the bathroom/shower, poor lighting in the home Additional Notes: _____________________________________________ Glaucoma Screening: (checking pressure in the eyes) Glaucoma is a condition with elevated eye pressure I am currently being treated for glaucoma, I had glaucoma screen on _________________, unaware if ever had screened for glaucoma Pain Evaluation: During the past four weeks have you had bodily pain? 5 None mild moderate severe HOSPITALIZATIONS Dates Facility Reason Outcome/ Notes FOR OFFICE USE ONLY o Initial Preventative Physical Exam o Initial annual wellness visit Today’s Date Date of Last Exam o Subsequent annual wellness visit Language or other communication barriers: (Describe) Interpreter or other accommodations provided today: (describe) Reviewed above history and findings o Other