The Trauma Bay Guidebook - Vanderbilt University Medical Center
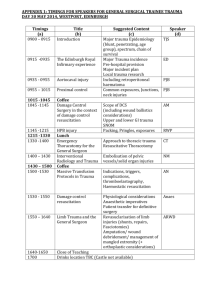
advertisement

The Trauma Bay Guidebook A work product by the staff of the Vanderbilt Adult Emergency Department Kevin High/Editor This guidebook is intended to act as a resource for any and everyone that functions as a practitioner in the trauma bays of the Vanderbilt Adult Emergency Department. This guidebook contains policies, procedures and BMP’s (best management practices). It is thorough but not all inclusive and should not supersede sound clinical judgment. The guidebook is a work in progress and will be amended as needed by the Trauma Program Manager, Emergency Department management and staff. This document is a work product of the leadership/administration of Vanderbilt’s Adult Emergency Department and TWIG (the Trauma Working Interest Group) Authored/Approved 2011 2 Core Requisites for Staff Assigned to the Trauma Bays in the Vanderbilt Adult Emergency Department Introduction The purpose of this document is to clarify and outline the core requisites for being assigned as a PCT, Primary Nurse or Secondary Nurse or Paramedic to the Trauma Bay assignment within the Adult Emergency Department (ED). Vanderbilt Adult ED is a Level I Trauma Center and sees ~2400 Level I trauma patients per year. Each Level I patient receives a templated response from a team of 10+ individuals within the Vanderbilt system. This team is composed of physicians, nurses, respiratory techs, paramedics, PCT’s, radiology techs, service center personnel and social workers. The following pertains to individuals functioning as a PCT, Primary Nurse and Secondary Nurse/Paramedic. Discussion The staff assigned to the aforementioned roles are done so by the charge nurse on duty. Staff have completed an orientation to the trauma bays and each of the respective roles prior to being assigned. 3 Each staff member has a specific role and duties during a trauma including a position at the bedside (see above image) Introduction/Initial Orientation Each role has a different set of requirements and orientation standards; each of these will be covered. Patient Care Tech (PCT) Each PCT must successfully complete their respective core ED orientation before working in the Trauma Bays. The requirements to work as a PCT within the Adult ED is to successfully complete the ED PCT orientation; special attention focusing blood/lab specimen collection, handling of belongings and chest tube set up. Paramedics Individuals working in the paramedic role within the Adult ED work in the secondary role; they must complete their core ED orientation prior to being independently assigned to work in the trauma bays. The requirements to work as a paramedic within the Adult ED are one year experience, current ACLS, PALS, ITLS/PHTLS, BLS and have passed the basic arrhythmia test. Registered Nurses Registered Nurses working in the trauma bay may function in the primary or secondary role; they must complete their core ED orientation and a specific orientation to the trauma bays prior to being independently assigned to work in the trauma bays. The requirements to work as a nurse within the Adult ED are one year experience, current ACLS, PALS, TNCC, BLS and have passed the basic arrhythmia (BA) test. PCT’s Complete standard ED orientation Graduate Nurses Complete standard ED orientation ACLS, TNCC, PALS, CPR, BA current May orient to Trauma after 1 year from date of successful completion of ED orientation Must have completed orientation to Triage! Experienced Nurses Complete standard ED orientation ACLS, TNCC, PALS, CPR, BA current May orient to Trauma after 6 months year from date of successful completion of ED orientation Must have completed orientation to Triage! Paramedics Complete standard ED orientation; (trauma orientation runs concurrently) ACLS, ITLS or PHTLS, PALS, CPR, BA current 4 Working in the Trauma Bay RNs and Paramedics must maintain annual competencies, maintain certifications and be oriented to the triage role. During the Shift The primary nurse is responsible for performing the daily room checklists and confirming that the room(s) they are assigned to are stocked. Checklists are provided for the assigned nurse to utilize in checking the room. The checklists consist of: Large Trauma Bay Cabinet Basic Mayo Stand Set Up x 2 Overall Room Checklist Emergency Box Checklist (T2) Difficult Airway Cart Checklist (T2 and T3) In addition to checking assigned rooms the nurse shall perform the following tasks as needed during the shift: Check utility room for laryngoscopes (require cleaning or soaking) put them in service if possible Update dry erase board outside bays with staff names and roles Check utility room for dirty instrument trays; if present; notify and assure they are picked up by service center Check warmer; ample supply of blankets? IV fluids? Check each trauma bay for errant sharps and medications; dispose of properly Check hall for obstructions (chairs, carts, etc) make sure it is unobstructed Round on triage and other A pod areas; assist staff as needed. 5 Requirements/Components for Orientation to the Trauma Bays in the Vanderbilt Adult Emergency Department Introduction The purpose of this document is to clarify and outline the orientation requirements for the following disciplines undergoing trauma orientation. These individuals consist of the following; Patient Care Techs (PCT), Registered Nurses (Primary Nurse or Secondary Nurse) and Paramedics. This orientation is to be complete prior to assuming a Trauma Bay assignment within the Adult Emergency Department (ED). Vanderbilt Adult ED is a Level I Trauma Center and sees ~2400 Level I trauma patients per year. Each Level I patient receives a templated response from a team of 10+ individuals within the Vanderbilt system. This team is composed of physicians, nurses, respiratory techs, paramedics, PCT’s, radiology techs, service center personnel and social workers. The following pertains to individuals functioning as a PCT, Primary Nurse and Secondary Nurse/Paramedic. Patient Care Tech Complete standard ED orientation and have a minimum of three (3) Level I patient contacts. Paramedics Complete standard ED paramedic orientation; must have 12 Level I patient contacts in the secondary role. Registered Nurses Complete standard ED orientation; must have 20 Level I patient contacts as follows: 2 as scribe; 6 as secondary and 12 as primary. Note: the emphasis is less on hours worked and more on patient contacts. Each orientee should document patient contacts (patient name/stat name and MR number) in their Trauma 101 checklist/worksheet. 6 Orientation Content • Spine Immobilization • Rapid Sequence Intubation (RSI) • Blood Products • Medication Administration • Equipment Knowledge/Setup – Fluid warmer/ rapid infuser – Bair Hugger – Thoracotomy Set Up – Pelvic Binders – Central Line Placement – subclavians and femorals – Diagnostic Peritoneal Lavage – DPL – Burn Sheets – Pleurovac set up – Escharotomy Procedure • Equipment Knowledge/Setup – Storz set up – EZ I/O insertion – internal paddle trays These are core orientation points and each item should be covered in orientation by the orientee and the preceptor/supervising clinician. – hole in the heart kit – chest tube set up – Art line set up – Tracheostomy set up – Cricothyrotomy set up – DPL set up – Hare Splint • Zoll Set Up/Troubleshooting • Difficult Airway Situations/Equipment • Ultrasound • Review Foley Catheter: Do/Don’ts • Review NG/OG Tubes: Do/Don’ts 7 Trauma Bay Nurse’s Five Critical Daily Actions Check utility room for laryngoscopes (require cleaning or soaking) put them in service if possible Check utility room for dirty instrument trays; if present; notify and assure they are picked up by service center Check warmer; ample supply of blankets? IV fluids? Check each trauma bay for errant sharps and medications; dispose of properly Check hall for obstructions (chairs, carts, etc) make sure it is unobstructed Assigned to the trauma bays? Are you feeling bored or under stimulated? Complete each of the above at least once during your shift! 8 Trauma Bay Staff Positions/Roles Respiratory Tech Assists with Airway Mgt Accompanies Patient EM Resident Performs Airway Mgt Controls C-spine HEENT Exam EM Attending Supervises Airway Mgt Primary RN Room Prep Connect Monitors Assist with Procedures Secondary RN or EMT-P Obtain Manual BP Assist with Procedures Accompany Patient Trauma Junior Performs Secondary Exam Performs Procedures PCT Room Prep Labs/Belongings Trauma Senior/R4 Acts as Trauma Team Leader Oversees Resuscitation Trauma Attending Assists/Oversees Resuscitation Scribe RN Documents Resuscitation 9 Ancillary Personnel Ancillary personnel are involved in the resuscitation with limited or no direct patient contact. Radiology Technician-takes and develops plain films as directed by the trauma team leader (must wear PPE) Medical Student-tasks as assigned by the by the trauma team leader (must wear PPE) Service Center Personnel-room prep and equipment management as directed Social Worker-gathers information; assists with patient and family needs ED Registrar-gathers demographic information Environmental Services-room prep and clean up Trauma Resuscitation Team Personnel: Detailed Description of Responsibilities Trauma Team-Leader-the senior (PGY-4) Surgical Resident serves as the trauma team leader and directs the overall resuscitation. The TTL initiates the resuscitation and assumes responsibility for life saving procedures such as assisting with procedures including surgical airway, emergent chest tube placement, and ED thoracotomy. The TTL is responsible for the majority of communication during the resuscitation. Trauma Attending or Fellow-the Trauma Attending or Fellow assumes the overall responsibility for the resuscitation and for supervising the Trauma Team Leader. If the Trauma Attending or Fellow is not present, the ED Attending will assume this role and responsibility. The Trauma Attending/Fellow is the designated trauma triage officer responsible for directing flow of patients to the OR, CT and ICU. It is imperative that the Trauma Attending/Fellow be in close communication with the Trauma Unit Charge Nurse for bed allocation and availability. Primary EM Resident– an Emergency Medicine Resident will perform the primary survey and also complete the neurological/HEENT part of the secondary survey. The EM Resident will perform airway procedures and will be supervised by the EM Attending. The EM resident may also be tasked with insertion of a gastric tube and controlling bleeding from head/scalp lacerations. ED Attending– is responsible for the airway and supervising the Primary EM Resident. In the absence of the Trauma Attending/Fellow the ED Attending will have overall responsibility for supervising the TTL and the resuscitation as a whole. The EDA is also responsible for all ED staffing, equipment and triage into the ED. The EDA may also assume the role of TTL during the resuscitation of multiple patients. Trauma Junior-a Surgery or Emergency Medicine R2 that performs the secondary survey with the exception of the airway/HEENT portion. This individual performs the rectal exam and other procedures as directed by the TTL. Respiratory Therapist-responsible for placing patient on high flow oxygen via mask/or ventilating the patient via ambu bag as directed by the Primary EM resident. The RT will accompany the patient to the Trauma Unit and/or CT scan. 10 Primary Nurse-this role is filled by a RN who places monitoring devices (ECG, Sa02, NIPBP on the patient after the move from the EMS stretcher. The PN will also assure that there is a functioning IV in place and if not initiate one; the PN may be tasked with blood draw, administering drugs, log rolling the patient and packaging the patient for transport. The PN is also responsible for room stocking. Secondary Nurse or Paramedic – The SN or PM will obtain the first manual blood pressure from the left arm and call it out for the TTL and team to hear. This person has the responsibility for coordinating transport outside the trauma bay; at times the secondary person may be accompanied by other ED staff. Scribe Nurse (Scribe) The scribe nurse is primarily responsible for keeping a written record of the resuscitation (the trauma flow sheet) and for coordinating the retrieval of equipment and item requested by the trauma team. (blood products, drugs, etc.) The scribe also initiates videotaping, acts as a conduit for information to the Trauma Unit, OR and assists in crowd control. Patient Care Technician/PCT - The PCT’s primary responsibilities are to ensure that blood is sent for appropriate tests, placing patient on secondary monitor, sorting and performing an inventory of belongings, assisting with transportation and equipment set up. Ancillary Personnel Radiology Technicians (RT) - The RT should be present at all trauma resuscitations and be prepared to perform the standard chest x-ray and pelvis xray as directed by the Trauma Team Leader. ED Social Worker-the ED Social Worker assists as directed by the TTL, Trauma/ED Attending. Trauma Nurse Practitioner(TNP)- The TNP will be available to assist with trauma resuscitations at night and occasionally during the day depending on the acuity and volume of the TNP service. Medical Student (MS)- The role of the MS is commensurate with their abilities as determined by the trauma service. The MS will be assigned tasks by either the TTL. Service Center Personnel -one staff member should remain in the bay to bring additional supplies needed for the resuscitation. ED Registration Personnel- one ED registration person may be present in the bay to gain demographic information. At no time should the gathering of said information interrupt any part of the resuscitation. Registration personnel are not allowed at the patient's bedside during the resuscitation 11 Highly Successful Habits and Qualities of a Trauma Bay Practitioner The following outlines a few of the habits and qualities of someone that is an exceptional trauma team member. They are competent: they know their role, the do’s and don’ts and follow them They communicate well; they are assertive and not aggressive They have an in-depth knowledge base of the room, the trauma system and process They pay attention to detail They have a good work ethic and are adaptable They work hard at everything; not just taking care of Level I patients They anticipate the team’s and the patient’s needs and work to be a step ahead Critical Actions for Primary/Secondary Team Members Ensure/call for a prebrief Have scissors, stethoscope within reach Observe noise discipline; minimize talking during critical procedures; especially airway interventions Communicate well with primary or secondary; specifically on drug dosages and administration Verbally repeat/crosscheck orders for clarification ++++++++++++++++++++++++++++++++++++++++++++++++++ The following is a compilation of best management practices (BMP's) put forth by the TWIG group outlining practices and actions that optimize patient care and flow in the trauma bay. Primary Reduce clutter; both visibly and in cabinets Have all RSI drugs in room, including "T pack" and Vecuronium (Succinylcholine, Rocuronium, Etomidate, Lidocaine, Epi, Atropine and anticipated antibiotics Confirm there are three suction set ups available and ready Retrieve the Storz Blades (both #3 and 4) from T-3 cabinet Place monitors Responsible for completing chart Right arm IV –is it adequate? Obtain a temperature on the patient prior to departure from the bay Verbally repeat orders for clarification Remove straps from board Ultrasound machine in room? Administer drugs as ordered Ensure blood for labs is drawn and given to PCT Call out vitals for the room and for the camera, if conditions warrant OG/NG post-intubation (make sure have it ready always tucked in at bottom of Phillips monitor) Make sure Foley gets placed for burn patients 12 Secondary RN or Paramedic Have manual BP cuffs set up and ready; at least one of each size Remove straps from board OGT with syringe/lube in reach? Ultrasound machine in room? Start IV if needed Ensure blood for labs is drawn and given to PCT Have tetanus in room, give if ordered Obtain blood for labwork Document well; especially events outside trauma bay (CT scan, OR, etc) Give drugs as ordered If meds from Pyxis needed (e.g. Ancef, Gent), get those (if able to leave room) OG/NG post-intubation If EMT-P (and staffing permits), transport pt to CT PCT Have glucometer in room Place Pt ID/Armband-verbally announce with location of armband placement Blue card and sticker on Zoll Have stickers ready at "PCT cart" Warm blankets in room Remove clothes and jewelry Place Zoll monitor at end of bed Attach monitor to patient Complete property record after patient care is completed Place blood in tubes and send to lab Confirm that an O2 tank is on the bed and is full Assist with equipment set up (chest tube set up, etc) Expose patient Remove straps from board Drop box valuable items Confirm patient’s clothing is placed under stretcher prior to transport Assist with splinting extremities Send labs--including type/screen--and click off labs in Wiz Get urine from Foley, if already in place Do property record, , drop valuables 13 Scribe Confirm that blood administration paperwork is done correctly Ensure that order sheet is signed by the physician and that the orders are correctly documented Complete the chart quickly and in a timely manner Make sure the chart is given to the staff member accompanying the patient to the unit, OR or CT scanner Confirm that blood was drawn and sent to lab Do triage, opening note narrative Make sure medication times are documented well Ensure blue card is taped to Zoll monitor Make sure pre-brief done Have chart in room before pt arrival Hit "record" just prior to patient entering room Assist in getting additional meds (e.g. Ancef, Gent) from Accudose Get uncrossmatched blood from blood fridge if ordered, or delegate getting from fridge--check off blood with another licensed staff member Make sure curtains closed Sign EMS run ticket Be assertive; don’t be afraid to speak up; monitor noise discipline 14 Safety and Noise Discipline in the Trauma Bay The issue of patient safety during the trauma resuscitation process is paramount. Medical error can oftent be directly related to human factors issues and poor communication. The use of aviation crew resource management (CRM) techniques are ideal for addressing these issues. Core CRM actions include but are not limited to: Conducting a pre-brief prior to patient arrival that includes team member introduction, summary of known patient information and plan of care. A "time out" prior to procedures; including patient identification, procedure clarity, equipment and staff available. Maintenance of noise discipline; especially during procedures. Minimizing uneccessary talking, pager, radio and phone tones. Constant clarification of patient's condition, plan of care and next steps. Noise/Crowd Control The FAA regulations are clear on noise discipline; referred to as the “Sterile Cockpit Concept*” During critical phases of flight (ground taxi, takeoff, landing and flight below 10K ft) no crew member shall permit activity that will distract crew from performance of duty; including talking and extraneous noise. *FAR 121.542 and 135.100/Federal Aviation Administration Maintaining noise discipline during the resuscitation and especially during critical phases (procedures, etc) is critical and a concept that we adhere to as a team. This aviation practice has a practical place in healthcare. Staff/Personal Safety Everyone in the "blue square" area must wear PPE. Lead aprons are also available in each room. If you use a sharp; you own it. Dispose of your sharps; maintain a high level of situational awareness with regards to sharps. Each patient should receive a "threat assessment" upon entering the bay. Any chemicals, hazardous materials, weapons, etc should be noted, announced to the group and dealt with. Any and everyone involved in the trauma resuscitation process is empowered to speak when and if there is a ongoing or past issue or event that compromises patient or team safety. 15 Special Situations Tips/Tricks and Pearls Prearrival Listen to EMS radio report if possible; it can assist you in preplanning Confirm ultrasound machine in room Have party pack/intubation drugs on hand; even if patient is already intubated by EMS Arrival Keep in mind the airway physician coordinates the move; not EMS Remind EMS to drop rail and not stand between the beds Airway/Intubation If pushing drugs, verbally confirm order with physician Do not push until you ask and physician confirms that they are ready DO NOT push drugs in the arm where an NIBP cuff is attached/located ALWAYS sedative first; then paralytic Know appropriate doses of each; be careful not to underdose paralytic Consider half or one third dose of etomidate in hemodynamically unstable patient Etomidate burns on injection; warn the patient Make sure the patient is on both cardiac monitor and pulse ox prior to pushing drugs Do not perform selleck maneuver or cricoid pressure unless ordered by a physician DO perform "lip traction" (pull out cheek on patient's right) to provide intubator more room Maintain noise discipline during the procedure; don't announce vital signs or ask unnecessary questions Monitoring/Obtaining Blood Pressure When applying monitor electrodes try not to put them on sites where a chest tube or subclavian line my need to be placed later Quickly obtain manual blood pressure; the entire resuscitation momentum hinges on it If unable to hear/auscultate blood pressure after one attempt state "I'm unable to auscultate a BP; will attempt to palpate one" Palpate the blood pressure; if it is measurable announce it to the room If palpated blood pressure is not measurable state "I'm unable to palpate a blood pressure" state whether or not there is a radial pulse present 16 DO not use any of the following verbiage to describe your attempt "I can't get one" or "I don't hear anything" Announce your findings clearly and loudly to the room Anticipated Actions/Procedures/Equipment Any patient with long bone injuries will require splinting; have the disposable yellow splints and/or hare splints in the room With any patient with penetrating thoracoabdominal trauma you should have the thoracotomy set up out on Mayo stands. (thoracotomy tray, internal paddles, finochetto retractor) Transport to the OR Must be done by both RN and Paramedic-no exceptions SBAR handoff on blood products to Anesthesia MD 17 Trauma Bay Daily/Shift Checklist Suction set up Oxygen tank IV NS Setup (time, date, blue cap & pressure bag) Cardiac monitor (leads/electrodes) Ambu Bag (BVM) Airway box o EtC02 detector o Stylets (peds/adult) o Blades (peds/adult) o Handles IV Carts Mayo stands (3) o One (1) Empty o One (1) with Chest Tube Set-Up o One (1) with Central Line Set-Up ED Stretcher (w/ functioning IV pole) Zoll Monitor (w/ cables & battery) Storz Device If you are a nurse assigned to a Manual BP set ups bay or bay(s) you are responsible for checking the equipment and Thermometer items on this list and maintaining IV Pump an acceptable supply of each Warm fluids during your shift. You may use service center staff Level I infuser to augment/supplement stocking Bair Hugger with blanket but you are responsible for assuring that the room is Oxygen Cylinder stocked. Hare Traction Splints Available? 18 Mayo Stand Set Up for Chest Tube Contents Chest tube tray Sterile Gloves (assorted sizes) #10 blade scalpel Suture 2 and 0 silk Fluffs (2) OR/blue towel pack (2) 36fr chest tube Chlorhexidine 3" tape 19 Mayo Stand Set Up for Incoming Level I Patient There should be a minimum of three (3) Mayo stands in the room prior to patient arrival. One should contain a central line set-up, one a chest tube set-up and the other should be empty. 20 Mayo Stand Set Up for Central Line Contents Central line/Cordis kit Sterile Gloves (assorted sizes) Suture 0 silk Fluffs (1) OR/blue towel pack (2) Chlorhexidine 3" tape 21 Resources www.vanderbilttraumabay.com www.vanderbiltem.com www.traumaburn.com 22