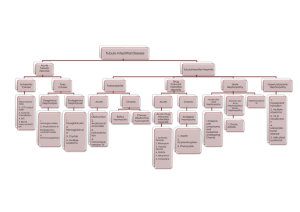
renal - Improving care in ED
advertisement

RENAL 1. Concerning acute tubular necrosis a. Cephalosporins are not a causative agent b. Nephrotoxic causes are associated with a poor prognosis c. Casts are found in the loop of Henle d. Rhabdomyolysis is not a cause e. Ischaemic tubular necrosis is uncommon after haemorrhagic shock 2. Regarding acute tubular necrosis a. It is associated with hyperkalaemia not hypokalaemia in recovery – hyperkalaemia initially (when UO low) b. Non-oliguric has a better recovery <- correct c. It is associated with ischaemic cortical cells - medullary d. 80% are associated with anuria e. ? 3. Ischaemic tubular necrosis is associated with a. Maintenance stage with polyuria – with oliguria b. Predominantly proximal necrosis c. Intact basement membranes - damaged d. Tubular cast obstruction <- correct e. Distal necrosis only 4. Hypertensive renal disease a. 15% is secondary to renal artery stenosis – 2-5% b. 60% of renovascular hypertension is due to fibromuscular hyperplasia – fibroelastic hyperplasia c. malignant hypertension only arises if previous hypertension – not always, but usually d. onion skinning correlates with degree of renal failure <- correct e. glomerulonephritis occurs 1-3 weeks post group B strep infection – group A beta haemolytic 5. The morphology of renal failure includes a. ? b. ? c. ? d. ? e. ? 6. Regarding the hepatorenal syndrome a. It is irreversible – poor prognosis (need liver transplant!) b. One loses the ability to concentrate urine – water retention c. Urine has a high sodium concentration – there is Na retention d. The urine is hyperosmolar <- correct e. The favoured theory of its generation involves increased renal blood flow – decreased renal perfusion pressure followed by renal vasoconstriction 7. Urolithiasis a. Presence of hypercalcaemia implies renal insufficiency b. A patient with leukaemia is likely to make cystine calculi c. Calcium is the major component of 35% of calculi d. Struvite stones are made up of magnesium-ammonium-phosphate e. Hypercalcaemia is found in most patients who make renal calculi 8. In pyelonephritis a. 85% of infections are caused by Gram negative bacteria <- correct b. ureteral obstruction makes haematogenous infection less likely c. ureteral obstruction allows bacteria to ascend the ureter into the pelvis d. infection is less likely during pregnancy e. papillary necrosis and perinephric abscess are common sequelae 9. Acute loss of 30% of renal capacity in a young person a. Worsens with ACE inhibitors b. Can still produce a normal urine output and maintain normal electrolytes c. ? d. ? e. ? 10. Acute nephritic syndrome has all of the following features EXCEPT: a. Proteinuria b. Haematuria c. Hypertension d. Hyaline casts e. Oliguria 11. Regarding nephrotic syndrome, which of the following is TRUE? a. Albumin is lost and other globulins unaffected b. Hypertension c. Alteration in serum mlipid levels d. Sodium and water excretion e. Haematuria 12. Regarding acute glomerulonephritis a. White blood cells dominate the urinary sediment b. Post streptococcal GN usually appears 6-8 weeks after a strep infection c. Patients have a normal or low BP d. Henoch Scheonlein Purpura is most frequent in children and young adults e. Acute GN is not associated with systemic lupus erythematosus 13. With respect to streptococcal infection a. May result in glomerulonephritis 3 weeks post infection (Group A beta haemolytic strep) b. ? c. ? d. ? e. ? 14. Acute glomerulonephritis (acute proliferative = poststrep or postinfectious GN) a. Occurs 1-4 weeks after impetigo <b. Due to toxic effects of streptolysin on basement membrane c. Due to group B alpha haemolytic strep d. Leads to renal failure usually e. ? 15. In chronic renal failure, morphology includes: a. Glomerular hyperplasia with dilation of tubules b. Slowing of filtrate through loop of Henle c. Decreased pressure in glomerulus d. Hyaline connective tissue changes in glomeruli, tubular atrophy <- correct e. ? 16. Renal failure morphology: a. Nephron dilation and hypertrophy b. ? c. ? d. ? e. ? 17. Alkaline urine causes precipitation of a. Magnesium-ammonium-phosphate stones b. ? c. ? d. ? e. ? 18. Nephrotoxic ATN is caused by all EXCEPT: a. Erythromycin <b. Contrast c. Carbon tetrachloride d. Gentamicin e. Lead 19. Renal calculi occur in the presence of a. An alkaline pH of urine – can do… b. Large residual volume of urine – low volumes c. Urinary obstruction – they do if they are causing the obstruction d. Usual concentrations of urinary constituents – require increased concentrations for precipitation e. Deficiency of inhibitors of crystal formation in urine 20. renal calculi a. 50% with high calcium get calcium oxalate stones b. they are bilateral in 80% - unilateral in 80% c. 30% have protease splitting bacteria d. ? e. ? 21. ischaemic acute renal tubular necrosis is characterized by a. occlusion of tubular lumens by casts <- correct b. acute tubular injury is most obvious in the proximal convoluted tubule – multiple points with skip lesions c. absence of eosinophilic hyaline casts – these are common d. large continuous areas of epithelial necrosis – skip lesions e. sparing of the parts of the tubule in the renal medulla – most vulnerable 22. Renal stones a. Are unilateral in 60% of patients – 80% b. Formation is enhanced by a deficiency of inhibitors of crystal formation in urine c. Are least commonly composed of magnesium ammonium phosphate – 15-20% are, cyteine is 1% d. Can be formed by urea splitting organisms such as Proteus and Klebsiella – proteus and some staphlococci e. Formed of calcium are radiolucent 23. Regarding pyelonephritis a. Uncontrolled hypertension is a major predisposing factor b. The microscopic changes in chronic pyelonephritis are pathognomonic c. Staphylococci and streptococcus faecalis are common pathogens d. In the first year of life, it is more common in females e. It is generally a benign and self limited condition 24. Membranous glomerulonephritis a. Is always due to an underlying renal condition - no b. Is idiopathic in 10% of cases – 85% c. Leads to chronic renal failure in 60% of patients – 10 – 40%, but persistent proteinuria in 60% d. Has a typically aggressive disease progression- no e. Is the most common cause of nephrotic syndrome in adults – actually the book list FSGS as the most common cause at 35% c.f. 30%, but nonetheless MGN is a common cause