CLIA references for the Laboratory Test Report for EHR
advertisement
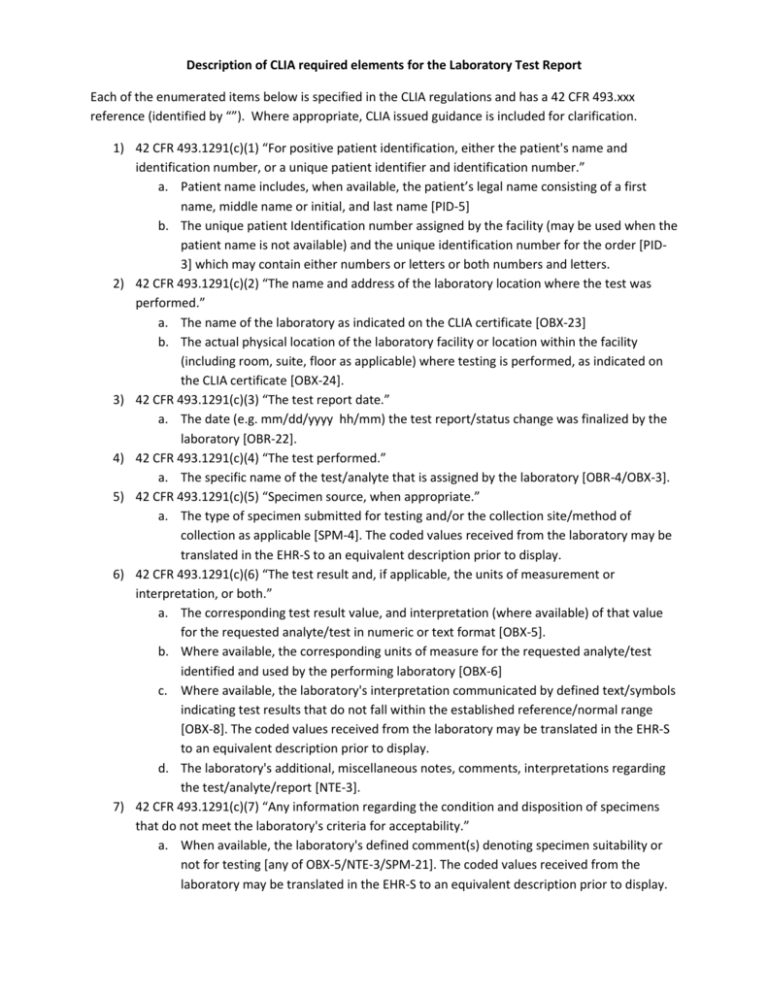
Description of CLIA required elements for the Laboratory Test Report Each of the enumerated items below is specified in the CLIA regulations and has a 42 CFR 493.xxx reference (identified by “”). Where appropriate, CLIA issued guidance is included for clarification. 1) 42 CFR 493.1291(c)(1) “For positive patient identification, either the patient's name and identification number, or a unique patient identifier and identification number.” a. Patient name includes, when available, the patient’s legal name consisting of a first name, middle name or initial, and last name [PID-5] b. The unique patient Identification number assigned by the facility (may be used when the patient name is not available) and the unique identification number for the order [PID3] which may contain either numbers or letters or both numbers and letters. 2) 42 CFR 493.1291(c)(2) “The name and address of the laboratory location where the test was performed.” a. The name of the laboratory as indicated on the CLIA certificate [OBX-23] b. The actual physical location of the laboratory facility or location within the facility (including room, suite, floor as applicable) where testing is performed, as indicated on the CLIA certificate [OBX-24]. 3) 42 CFR 493.1291(c)(3) “The test report date.” a. The date (e.g. mm/dd/yyyy hh/mm) the test report/status change was finalized by the laboratory [OBR-22]. 4) 42 CFR 493.1291(c)(4) “The test performed.” a. The specific name of the test/analyte that is assigned by the laboratory [OBR-4/OBX-3]. 5) 42 CFR 493.1291(c)(5) “Specimen source, when appropriate.” a. The type of specimen submitted for testing and/or the collection site/method of collection as applicable [SPM-4]. The coded values received from the laboratory may be translated in the EHR-S to an equivalent description prior to display. 6) 42 CFR 493.1291(c)(6) “The test result and, if applicable, the units of measurement or interpretation, or both.” a. The corresponding test result value, and interpretation (where available) of that value for the requested analyte/test in numeric or text format [OBX-5]. b. Where available, the corresponding units of measure for the requested analyte/test identified and used by the performing laboratory [OBX-6] c. Where available, the laboratory's interpretation communicated by defined text/symbols indicating test results that do not fall within the established reference/normal range [OBX-8]. The coded values received from the laboratory may be translated in the EHR-S to an equivalent description prior to display. d. The laboratory's additional, miscellaneous notes, comments, interpretations regarding the test/analyte/report [NTE-3]. 7) 42 CFR 493.1291(c)(7) “Any information regarding the condition and disposition of specimens that do not meet the laboratory's criteria for acceptability.” a. When available, the laboratory's defined comment(s) denoting specimen suitability or not for testing [any of OBX-5/NTE-3/SPM-21]. The coded values received from the laboratory may be translated in the EHR-S to an equivalent description prior to display. b. When available, the laboratory's comment(s) denoting the condition of the specimen (hemolysis, lipemia, icterus, clotted, etc.) [any of OBX-5/NTE-3/SPM-24]. The coded values received from the laboratory may be translated in the EHR-S to an equivalent concept prior to display. 8) 42 CFR 493.1291(a) “... patient-specific data are accurately and reliability send [sic] from point of data entry (whether interfaced or entered manually) to final report destination...” a. 42 CFR 493.1241 (c) (3) “The sex and age or date of birth of the patient” i. Administrative Gender should be displayed as either the coded value (e.g. M, F, …) or an appropriate translation (e.g. Female, Male,…) [PID-8] ii. Date of Birth (or Age) should be displayed in either date/time format or in numeric with units (e.g. 15 years) [PID-7] b. 42 CFR 493.1241 (c) (6) “The date and, if appropriate, time of specimen collection” i. The date (e.g. mm/dd/yyyy) and time (e.g. hh/mm) when the specimen to be tested was obtained from the patient [OBR-7] c. 42 CFR 493.1241 (c) (7) “Any additional information relevant and necessary for a specific test to ensure accurate and timely testing and reporting of results, including interpretation, if applicable” i. NTE segments associated with the order and/or results 9) 42 CFR 493.1291(d) “Pertinent “reference intervals” or “normal” values, as determined by the laboratory performing the test, must be available to the authorized person who ordered the test and, if applicable, the individual responsible for using the test results” a. The “reference intervals” or “normal” values that are determined by the performing laboratory and correspond to the particular test/analyte result [OBX-7] 10) 42 CFR 493.1291(k) “When errors in the reported patient test results are detected, the laboratory must do the following... (2) Issue corrected reports...” a. The laboratory's status of the test result/report (preliminary, partial, final, corrected, etc.) [OBX-11/OBR-25]. The coded values received from the laboratory may be translated in the EHR-S to an equivalent concept prior to display. Note: all components of a single ordered test (e.g. CBC or Micro culture) must be included in a single “test report”. This includes all parent-child relationships that are part of a single HL7 R01 result transaction.