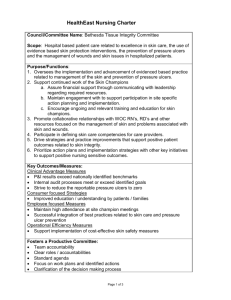
Developing an Evidence-based Multidisciplinary Fall Reduction
advertisement

1 Developing an Evidence-based Interdisciplinary Fall Reduction Program Jennifer Smith NUR 598 June 15, 2012 Naja McKenzie 2 Abstract The purpose of this study is support the hospital’s commitment to providing a safe environment for their patients by preventing falls and reducing fall-related serious injury. The project consists of working with an interdisciplinary team to develop, implement, and evaluate an evidence-based fall risk assessment tool to identify high-risk patients. A fall risk in the hospital setting may increase the length of stay, cost of hospitalization, and utilization of resources. Patients that fall during hospitalization have psychological and physical effects from a fall and have an increased risk of morbidity and mortality (Fonda, Cook, Sandler, Bailey, 2006). A fall risk reduction program that is interdisciplinary will be more effective at reducing the risk of falls. 3 Problem Identification Emerging reimbursement methods such as pay for performance penalizes for negative consequences such as fall-related injuries during hospitalization. Falls that occur in the hospital are a risk management problem and decrease the patient’s satisfaction and perception of the quality of care. The hospital’s current policy and procedure for falls does not meet national standards; the pediatric population is not assessed for their risk for falls. The organization has had an increase in patient falls per patient days and falls that result in moderate to severe injury in 2011. To meet national accreditation standards the organization must review their policy and procedures, develop a strategy to reduce the number of falls and falls with injury, and continually monitor its effectiveness. Solution Description The proposed solution is the development of a fall-risk reduction program that uses evidence-based assessment tools for adult and pediatric patients and interdisciplinary feedback from pharmacy, physical therapy, physicians, and nurses. The Morse Fall Scale will be used to assess adult inpatients and the Humpty Dumpty Scale will be used for pediatric inpatients. A screening process will be used to identify outpatients entering the facility for fall risk and interventions will be developed for those identified atrisk for falls. Care plans will be individualized with interventions based on patients fall risk category with appropriate referrals to interdisciplinary team members. Universal fall precautions will be implemented for all patients and interventions will increase for those identified as moderate, high-risk, and high-risk with mental impairment. The proposed solution is consistent with evidence-based practice; literature review indicates that fall reduction programs are more effective when they involve interdisciplinary teams and consider multifactorial reasons for patient falls. The project is a feasible low cost solution to increase surveillance, optimize the environment, and improve the management of patients at-risk for falls. The 4 program consists of the development of a fall reduction policy, revision of fall-assessment tools, education of staff, and evaluation of outcomes. The fall reduction program is consistent with the organization’s mission statement, “to provide high quality, comprehensive, safe and compassionate health care services” (Samaritan, 2012). The organization’s vision is to be recognized as the preferred provider in the community. The nursing division’s mission supports the organization’s vision to provide high quality, compassionate care supporting the patient’s mind, body, and spirit through human to human caring. Nurse care is patientcentered based on Jean Watson’s Caring Theory. The nursing staff collaborates with other health team members to meet the psychosocial, physical, and spiritual needs of the patient and their families. The nursing division is committed to providing staff with continued competency training and educational programs. Developing an Evidence-based Interdisciplinary Fall Reduction Program Literature review of best practices, fall risk assessment tools, and the importance of an interdisciplinary approach to reducing falls will be conducted and summarized in an annotated bibliography. The current fall reduction policy will be compared with best practices, National Database of Nursing Quality Indicators (NDNQI), and national accreditation standards. Findings will be reviewed with the Director of Nursing (DON) for input and approval of the project. Involving Formal and Informal Leaders The Director of Pharmacy will be involved to explore the possibility of adding a pharmacological review of medications of high-risk patients. The Director of Quality will be consulted to assist with developing a multidisciplinary fall team that will periodically evaluate the effectiveness of the fall reduction program. The Director of Physical Therapy will be asked for input on the development of the policy and the physical therapist’s role in fall reduction. A meeting will be held with Information 5 Services to determine the length of time and process to make changes to the fall assessment tool in the electronic medical record. Best practices will be reviewed with nurse managers of different units and the Nurse Practice Council; feedback will be received on fall reduction strategies that will work for our organization. Policy Development A draft policy will be developed that incorporates evidence-based practice and feedback from other disciplines and reviewed by the DON for suggestions prior to submitting to the Policy and Procedure Committee for approval. The draft policy will include updated nursing care plans and patient/family education materials. The draft policy will be reviewed at the nurse leadership meeting for nurse managers to have a last minute opportunity to provide feedback prior to approval. Once the policy is approved changes will be made to the documentation system. Education Program Following approval of the policy, an educational program will be developed to include: learning objectives, content outline, and Power Point that will be loaded on the computer education module net learning with a post-test to determine competency. The educational program will be reviewed by the Nurse Educators for final approval prior to being placed on net learning. A post-fall analysis will be developed to assist with identifying areas for improvement and assist with evaluating the reason for the fall. Materials will be ordered by the nurse managers such as: yellow star door magnets, gait belts, and bed/chair alarms. Employees will participate in developing a patient education video that will be loaded on the television educational channel. The proposed solution is a feasible cost-effective and necessary to reduce inpatient falls and meet national accreditation standards. The solution is consistent with the hospital’s mission, vision, and values of providing high quality care. Monitoring the implementation plan is important to ensure 6 activities are executed as planned. The DON will assist with ensuring that the implementation phase is carried out as scheduled. Research Support Literature review will consist of: 5 peer reviewed research articles on fall risk assessment tools and interventions, 15 peer reviewed research articles on fall reduction programs and best practices, and 5 peer reviewed research articles on the importance of interdisciplinary feedback in the development of fall reduction programs. A summary of 6 of six of these research studies are as included in this paper. Multidisciplinary Approach to Fall Reduction A three year research study performed 2001-2003 at General Medical Center in Melbourne, Australia indicates incorporating a fall risk program into all levels of the organization. This method is important to the success and sustainability of a fall prevention program. All patients admitted during the time frame were included in the study. A multi-strategy approach including revising the definition of fall, choosing a fall risk assessment tool, developing interventions based on assessment score, implementing practice changes, environmental and equipment changes, and staff education. The result of the study after two years showed a 19% reduction in falls and a 77% reduction in falls that result in serious injury. The study also revealed an increase in staff compliance with the fall risk assessment tool (Fonda et al, 2006). Pharmacological Review of Medications A research study performed in 2005 at Mercy Health Center (MHC) in Oklahoma City supports the importance of pharmacological review to identify patients at high-risk for falling based on medication assessment. Certain medication classifications have adverse effects that cause dizziness, orthostasis, and sedation. Developing a fall prevention program that incorporated a medication review by a clinical pharmacist resulted in a 30% reduction in falls, 48% reduction in injuries from falls and a savings of $217,000 within two years of implementation. 7 MHC developed a Medication Fall Risk Score (MFRS) using Beers criteria and Lexi-Comp’s Drug Information Handbook, and the American Hospital Formulary Service to categorize patients as high, medium, or low-risk for falling based on a medication profile. The medication profile was reviewed by clinical pharmacists and their recommendations were communicated to the prescribing physician in the progress notes and notification sent to the nurses to reinforce the high-risk fall care plan. Patients identified as high-risk for falls without cognitive impairment received medication adverse effects counseling from the pharmacist. JCAHO require patients to be assessed for their risk of falling including review of medication regimen and organizations develop strategies to reduce risks (Beasley & Patatanian, 2009). A retrospective case-crossover design study at Fukuoka Medical center a 600-bed acute care hospital in Japan indicates a strong correlation between certain medication classifications and falls. The study further indicated that newly initiating angiotensin II receptor antagonists, antiparkinsonian agents, antianxiety medications, and hypnotic agents increased the risk of falls. A total of 349 inpatient falls were reviewed for a 30 month timeframe from March, 2003-August, 2005; data collected from incident reports and medical records to assess an association between medication use and risk of falling. The case period was defined as the 3-day period just before the fall. To estimate the odd ratio with respect to medications they used conditional logistic regression analysis. Medications were divided into nine groups to evaluate an association between medication classes and falls. Falls related to medication use were computed using conditional logistic regression analysis and determined to have an odd ratio of 95%. The study concluded that medical professionals should be aware of the possibility that starting new medications may trigger the onset of falls and implement preventative strategies (Shuto, Imakyure, Matsumoto, Egawa, Jiang, Hirakawa, Kataoka, Yanagawa, 2010). 8 Adult Fall Risk Assessment Tools A descriptive and cross sectional study compared the sensitivity, specificity, and feasibility of four fall risk assessment instruments: (1) Hendricks II Fall Risk Model, (2) New York Presbyterian Fall and Injury Risk Assessment, (3) Maine Medical Center, (4) Morse Fall Scale. Data was collected from May-June (2006) on 17 units and 1,546 patients were reviewed with results indicating that the Morse Fall Scale had the highest accuracy rate of 100% (Chapman, Bachand, & Hyrkas, 2011). Pediatric Fall Assessment Tools A case-control study at a pediatric teaching facility was conducted from 2005-2006 to assess the relationship between the Humpty Dumpty Fall Scale (HDFS) and the actual event of a fall. The HDFS assesses pediatric inpatients for risk of falls. The study was developed through literature review and intense discussion among nurses with extensive pediatric and adolescent experience. Chart reviews of 308 patients were done: 153 were children who fell during hospitalization and 153 were children that did not fall. The cases and controls were matched for demographics of age, gender, diagnosis, and unit location. Data was collected from medical, surgical, respiratory, neurology, oncology, and pediatric intensive care. A group of advanced practice nurse practitioners, clinical nurse specialists, directors, and staff nurses conducted the review and completed the HDFS scoring. The reliability in scoring the HDFS was calculated at 70% (Hill-Rodriguez, Messmer, Williams, Zeller, Williams, Wood, & Henry, 2008). Hill-Rodriguez et al. (2008) reported the HDFS to have a sensitivity of 0.85 and specificity of 0.24 with a positive prediction power of 0.63. The number of patients correctly classified was 59.3%. The significant sample size suggests that the HDFS may be the best fall scale available to assess the pediatric population. The odds of high-risk patients falling were twice that of a low-risk patient. Pediatric risk assessment of falls could target children at risk for falls and allow staff to implement appropriate interventions. 9 Evidence-Based Practice A pilot project developed by the interdisciplinary falls team at New York Queens, a 500-bed culturally diverse community academic medical center showed a significant reduction in fall rates. The concept of the fall reduction program was that fall reduction was responsibility of all employees; each team member having different roles and responsibilities. Team building was a priority in reducing the number of falls and included in the educational program. All hospital employees attended a three hour education program taught by a doctorally prepared expert in gerontologic nursing. Each unit had a registered nurse “champion” that provided on-going coaching and mentoring to maintain the sustainability of the program. A reduction in falls was noticed immediately after the education of staff and within six months the fall rate decreased from 11.48 per 1,000 patient days to 3.17 (Wexler, O’Neil, D’Amico, Foster, Cataldo, Brody, Zheng-Bo, 2011). The project was eventually called the “Ruby Red Slipper Program” because patients that were identified as high-risk for falls were given red non-skid socks. Staff input during the development of the program indicated this would be better than signage. Other interventions included improved communication between shifts, ticket-to-ride, and completing a post-fall analysis immediately after the fall. Monthly data was disseminated on each unit for staff to track improvements. Implementation Plan Change Theory Lewin’s Change Theory was chosen to assist with the development of the implementation plan. Kurt Lewin developed a three-step model to assist with organizational change which includes the following steps: unfreezing, movement, and refreezing (Kristsonis, 2004). The first step of the process, unfreezing consists of analyzing the current fall policy and making the employees realize that change needs to occur to align our fall policy with best practices. The second step is movement, which involves persuading 10 employees to agree that the current policy is not meeting best practice standards and involving them in the process by brainstorming and providing feedback during the development of the policy. The third step, refreezing is necessary to sustain changes so the employees do not revert back to old behaviors and practices. This step will be particularly important for the project to maintain the fall reduction program and monitor its effectiveness. Budget The majority of this project will be completed by the nursing project manager on a volunteer basis. Indirect costs include meeting with the DON, Director of Quality, Director of Pharmacy, Director of Physical Therapy, Information Systems, and Nursing Educators. The costs associated with these meetings are approximately $250 dollars. The time spent on clinical informatics making necessary documentation changes in the computer system are $320. A time frame will be allotted to existing committee meetings for the Nurse Practice Council, Nursing Leadership, and Policy & Procedure Committees. Direct costs for this program include printing educational materials for patient/family education which is a JCAHO requirement. Employee’s times associated with the development of a patient/family education video that will be placed on the patient education channel are estimated to be $700. Materials will have to be purchased such as: yellow star magnets, yellow arm bands, gait belts for each room, bed/chair alarms for each room. The initial cost for the materials is estimated to be $7546 for the entire hospital. The bed/chair alarms and gait belts will have to be periodically replaced. Each unit should have enough to have one of each item per room. These items will have to become part of the nursing unit’s annual budget. There is a possibility that pharmacy will need another clinical pharmacist depending on the volume of patients classified as high-risk requiring a medication review. The cost of an additional clinical pharmacist is approximately $117,000 annually. 11 Evaluation Plan The number of falls will be analyzed for three months after the implementation of a new policy with a goal of reducing the number of falls by 25%. At least 50 charts will be audited to analyze correct use of the fall-risk assessment tool, initiation of care plan, and documentation of education with the goal of 95% accuracy. The problem with assessing the effectiveness of a fall program is that the definition of a fall varies depending on the organization (Rutledge, Donaldson, & Pravikoff,, 1998). The Joint Commission on Accreditation (JCAHO) permits an organization to define what they consider a fall. The newly developed policy will use the National Database of Nursing Quality Indicators (NDNQI) definition of a fall: “An unplanned descent to the floor, either with or without injury to patient/resident/client” (ANCC, 2008). The policy will also standardize the level of injury to the NDNQI definitions: (1) none (patient did not sustain and injury from the fall, (2) minor injury (indicates those injuries requiring a simple intervention, (3) moderate (requires sutures or splints, (4) major (requires surgery, casting, and further exam), (5) death (resulting from injuries sustained from the fall). Having standardized reporting will assist with determining the successfulness of the fall reduction program. Outcome Measures The effectiveness of the fall reduction program data will be measured by monitoring data on fall incidence, severity of injury, percentage of repeat fallers, and number of days between major injuries. Fall rates will be analyzed for overall facility using the following formula (number of patient falls/number of patient bed days) x 1000. This method adjusts for fluctuation in census and is the recommended method by the American Nurses Association (ANA). The disadvantage to this method is that it calculates all falls including the number of repeat fallers. The number of repeat falls will be measured to determine what percent of the falls are second, third, fourth, or more falls. The injury rate will be 12 measured by using the following formula (number of injuries/number of falls) x 100. This method is recommended by the Department of Veteran Affairs, calculating the injury rate per 100 falls produces a meaningful rate. The number of days between major injuries will indicate the program’s overall success if the length of time between major injuries increases (Quigley, Neily, Watson, Wright, & Strobel, 2007). Data will be further analyzed by unit to determine opportunities for improvement. The effectiveness of the education program will be monitored by staff completing a post-test. At least 50 charts will be analyzed after implementation to assess for the correct use of the Morse Fall Scale Risk Assessment, appropriate care plans completed, documentation of patient/family education, and use of appropriate interventions such as wrist band/non-skid socks. Evaluation of Data Collection Data will be analyzed by reviewing incident reports and the post-fall analysis. The current computerized incident report system makes it difficult to extract meaningful data. A post-fall analysis was developed to assist with data collection and is to be performed during a post-fall huddle on the unit and handed in with the incident report. The post-fall analysis is a modified version of The Texas Medical Center Council of Nurse Executives Collaborative Patient Fall Prevention Protocol (2009) (see Appendix A Post Fall Analysis). The tool was modified using the Situation, Background, Assessment, Recommendation (SBAR) format. The staff is currently educated on the SBAR format and uses it to assist with communicating with health care providers. According to Throckmorton et al (2009), the concept of post-fall huddles was developed by James Haley for the Veteran’ Administration Hospital with a grant from the Robert Wood Johnson Foundation and has been evaluated to be an effective method to assist staff to determine the root cause of the fall while the information is still fresh in their minds. A data spreadsheet will be developed to monitor data from the post-fall analysis such as: age, primary diagnosis, pre-fall risk score, activity at the time of fall, 13 shift patient fell, day of the week, location of the fall, and length of hospital stay (see Appendix B). This information will also assist with submitting the fall data to the NDNQI database which requires a demographic profile (age, gender, diagnosis). The data gathered from the post-fall analysis will be used to develop a visual presentation of fall data and used to trend over time. This data will allow staff to understand how the data correlates to the fall reduction program and patient outcomes. Fall data will be analyzed on a quarterly basis by an Interdisciplinary Fall Team consisting of quality, pharmacy, nurse leaders, physical therapy, Patient Care Coordinators (PCC), and each inpatient unit will have a designated fall champion. The fall data will be analyzed for trends and opportunities for improvement. Nursing units with a higher than average fall rate will be reviewed for contributing factors and a plan of correction developed by the department manager. Resources Needed for Evaluation The post-fall huddle will require the staff’s time to discuss the potential for the fall and will require the registered nurse additional time to complete the form. An incident report and documentation in the medical record are already required. Some units are already completing a post-fall analysis for their nurse managers, but the form is not organizational specific and there is inconsistent use. Nurse Managers are presently required to review the incident reports and respond in the computerized incident report system Med-QM. The information provided on the post-fall analysis will decrease the amount of time the nurse manager must search through the medical record for necessary information to respond to the incident report. The nurse manager on each unit will turn in a completed data spreadsheet to the PCC group on a monthly basis. The PCC group already meets bi-weekly and the fall data analysis will be added to their agenda. The educational program and post-test will be loaded onto the hospital’s computerized education module. The resources required to monitor the effectiveness of 14 the project are minimal and feasible to implement. Supplying resources to plan, implement, monitor, and evaluate the fall reduction program will align the fall reduction program with national standards. Decision-Making For implementation and evaluation the fall team will use the Plan-Do-Study-Act (PDSA). The PDSA cycle allows the group to assess the outcomes of interventions and formulate changes based on data (Langley, Nolan, Nolan, Norman, & Provost, 1996). JCAHO standards require and organization to have a fall risk reduction program and continually monitor its effectiveness (JCAHO, 2006). Method to Maintain a Successful Project Solution According to Love (2008), theory-driven patient care improves patient safety and the professionalism of nursing. Our nursing division philosophy is grounded on Jean Watson’s Theory of Human Caring with the main concept being patient-centered care. Having a fall risk reduction program that identifies fall risk and patient specific interventions is theory-driven and evidence-based practice. The Rosswurm & Larrabee model will be used to guide nurses through the change in practice and behaviors. According to Pipe (2007), this model is an implementation strategy that has been proven to assist organizations with the successful application of introducing evidence-based practice. The model has six steps to assist with the promotion of change: (1) assess the need for change, (2) link the problem with interventions, (3) synthesize best evidence, (4) design practice change, (5) implement and evaluate the change in practice, (6) integrate and maintain the change in practice. Other important strategies to safeguard a successful project are: extensive education of all disciplines, patient education materials, and having the appropriate safety equipment readily available on the units. All interdisciplinary staff members that have patient contact will be educated on the fall prevention program and their role in preventing falls. There must be least a 25% reduction in falls and 50% 15 reduction in falls with serious for the project to be considered successful and maintained. The interdisciplinary fall team will use the PDSA model to revise the program if the targeted goal is not met. Dissemination of Findings Results of this project will be presented at the Nursing Division’s leadership meeting, the Nurse Practice Council, and Quality Council. Monthly results will also be posted on individual units in a visual display that is easily understood by all staff members. If the project is successful and the data considered reliable an article for publication may be written related to the process of developing a collaborative interdisciplinary fall reduction program. 16 References American Nurses Credentialing Center. (2008). Application manual magnet recognition program Silver Springs, Maryland. Beasley, B., Patatanian, E. (2009). Developing and implementation of a pharmacy fall prevention program. Hospital Pharmacy. 44(12 ), 1098-1102. Chapman, J., Bachand, D., & Hyrkas, K. (2011). Testing the sensitivity and feasibility of four fall risk assessments tools in the clinical setting. Journal of Nursing Management. 19(1),133142. doi:10.1111/j1365-2834.2010.0125x. Fonda, D., Cook, J., Sandler, V., Bailey, M. (2006). Sustained reduction in serious fall related injuries in older people in the hospital. The Medical Journal of Australia, 184(8), 379-382. Hill-Rodriguez, D., Messmer, P.R., Williams, P.D., Zeller, R.A., Williams, A.R., Wood, M., Henry, M. (2008). The humpty dumpty falls scale: A case-control study, JSPN.14(1), 22-31. Joint Commission on Accreditation of Healthcare Organization (2006). Top five sentinel events by setting of care. January 2001 to July 2005. Retrieved from http://www.jointcommission.org. Kim, E., Monrdiffi, S.Z., Bee W., Devi, K., & Evans, D. (2007). Evaluation of three fall risk Assessment tools in an acute care setting, Journal of Advanced Nursing. 60(4), 427-435. doi: 10.1111/j.1365-2648.2007.04419.x Kristsonis, A. (2004). Comparison of change theories. International Journal of Scholarly Academic Intellectual Diversity. 8(1). Love, K. (2008). Interconnectedness in nursing : a concept analysis, Journal of Holistic Medicine. 26(4), 255-265. Pipe, T. (2006, August). Optimizing nursing care by interpreting by integrating theory-driven 17 Evidence based practice. Journal Nursing Quality Care, 22(3), 234-238. Poe, S.S., Cyachm, M.M., Gartrell, D.G., Radzik, B.R., Joy, T.L. (2005). An evidence-based approach to fall risk assessment, prevention, and management. Journal Nursing Care Qualiy, 20(2), 107-116. Quigley, P., Neily, J., Watson, M., Wright., Strobel, K. (February 28, 2007). Measuring fall Program outcomes. Online Journal of Nursing. 12(2). doi: 10.3912.OJIN.Vol12No02PPT01. Rutledge, D.N., Donaldson, N.E., Pravikoff, D.S., (December 15, 1998). Online Journal of Clinical Innovations. 1(9). 1-33. Samaritan Medical Center (2012). Samaritan Medical Center Mission Statement. Retrieved May 15, 2012 from http://www.samaritanhealth.com Shuto, H., Imakyure, O., Matsumoto, J., Egawa, T., Jiang, Y.,Hirakawa,M., Kataoka,Y., Yanagawa, T. (2010). Medication use as a risk factor for inpatient falls in an acute care hospital: A case-crossover study. British Journal of Clinical Pharmacology, 69(5), 535-542, doi:10.1111/j.1365-2125.2010.03613x. Wexler, S.S., O’Neill-D’Amico, C., Foster, N., Cataldo, K.A., Brody, P., Zheng-Bo, H. (2011). The ruby red slipper program: An interdisciplinary fall management program in a community academic medical center. MedSurg Nursing, 20(3), 129-133. Appendix A 18 Post-Fall Analysis Situation 1. Time of day fall occurred:__________ Day of the week:___________ Length of hospital stay:________________(# of days admitted) 2. Staffing: (Circle) Full staff Shift understaffed (explain):________________________________ Some unavailable due to ___________________(e.g., breaks, emergency on unit) 3. Where did the fall occur? (Circle) Patient room Bathroom Hallway Radiology or Test/Treatment Environment 4. If fall occurred in patient room, circle items that were out of the patient’s reach: Call light Phone Kleenex Food tray Waste basket Assistive device (cane, walker, glasses, hearing aid) Other:____________________________________________________________________ 5. Hazardous foot wear: Yes No 6. Trip Hazards? (Circle) 19 Clothing Obstructed path to bathroom Tubing/cords None Other:___________________________________________________________________ 7. Evidence of slippery floor? Yes No 8. Was lighting adequate in the room? Yes No 9. Was there an equipment malfunction?(If marked yes equipment must be taken out of service and work order placed) Yes No Activity 10. What do we think this person was doing at the time of the fall? (Circle all that apply) Getting up on own Ambulating Trying to go to the bathroom Standing Up Reaching for something Toileting Leaning on something Sleeping Chair Wheelchair Other:_________________________________________________________________ Ask the person: “What happened this time that was different From all the other times you have done this activity?:________________________________________________________________ Background 20 11. Patient’s Primary Diagnosis :(Circle most applicable) Neurological Respiratory Hematology/Oncology Gastrointestinal Infectious Disease Renal Metabolic/Endocrine Cardiac Ear/Nose/Throat Unknown Orthopedic Psychiatric 12. Fall risk score:__________________________________________ Attach medication administration record for the 12 hours prior to the fall. Assessment 13. Glucose result:______________________ 14. Level of injury: (Circle one) None (indicates patient did not sustain an injury) Minor injury (indicates those injuries requiring a simple intervention) Moderate injury (indicates injuries requiring sutures or splints) Major Injury (indicates injuries that require surgery, casting, or further examination) Death (that results from injuries sustained from the fall) 15. If patient has a bed alarm what zone was it set:______________ 16. Fall categorized as: (Circle one) Accidental Anticipated physiological Unanticipated physiological Recommendation 21 What can we do to prevent this from happening again? (Circle all that apply) Increased rounding Non-slip footwear Oxygen tubing/IV tubing management Hip protectors Toileting plan Pharmacy review of meds Clear pathway to bathroom Patient/family education Remove clutter from the room Have items close to patient OT evaluation PT evaluation Alarm Improved positioning Other:___________________________________________________________________ Post-fall checklist Perform post-fall assessment and documentation to include: mental status, vital signs including pulse oximetry, blood glucose, description of injuries noted from fall. Notify physician, nursing supervisor, and family Perform post-fall monitoring, including neurological checks if evidence/suspicion of head injury Revise the plan of care to make patient high risk for falls to include prevention strategies based on post-fall huddle findings. Document interventions to prevent patient from falling again Communicate fall and increased risk to next shift, other healthcare team members, family if applicable Place falling star magnet on the door frame Re-educate patient/family on fall risk and document in medical record Complete this form and an incident report and give to the nursing supervisor Print MAR for 12 hours prior to fall and attach 22 Appendix B Patient ID # Patient age Date of fall Shift of fall Day of week of fall Location Activity Preof fall at time fall of fall Morse Fall Scale Length Level of Stay of Injury 23 Key Shift: 7a-7p= A, 7p-7a=P Activity at time of fall: Ambulating=1, Getting OOB=2, Standing up=3, Sitting down=4, Toileting=5, Sleeping=6, Chair=7, Wheelchair=8 Primary Diagnosis: Neurologic=1, Hematology/Oncology=2, GI=3, Infectious disease=4, Respiratory=5, Cardiac=6, ENT=7, Renal=8, Orthopedic=9, Metabolic/endocrine=10, Psychiatric=11, Unknown/other=12 Level of Injury: None=1, Minor=2, Moderate=3, Major=4, Death=5 Location of fall: Patient room=1, Hallway=2, Bathroom=3, Radiology/T&T=4 24 .