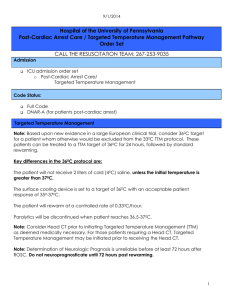
Post-Cardiac Arrest Care / Induced Hypothermia Pathway Order set
advertisement
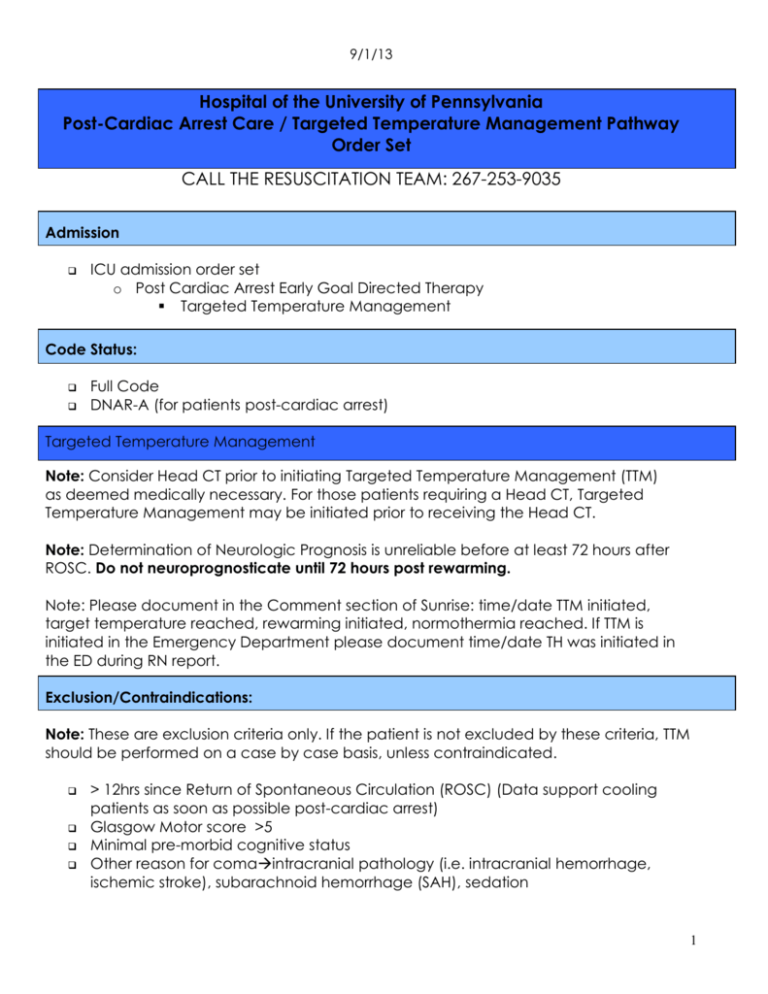
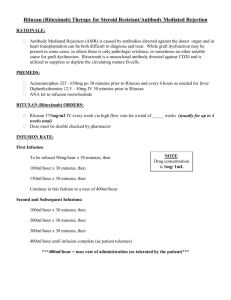
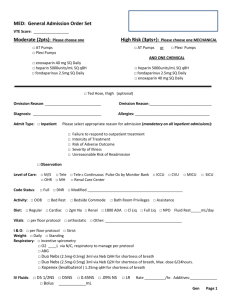
9/1/13 Hospital of the University of Pennsylvania Post-Cardiac Arrest Care / Targeted Temperature Management Pathway Order Set CALL THE RESUSCITATION TEAM: 267-253-9035 Admission ICU admission order set o Post Cardiac Arrest Early Goal Directed Therapy Targeted Temperature Management Code Status: Full Code DNAR-A (for patients post-cardiac arrest) Targeted Temperature Management Note: Consider Head CT prior to initiating Targeted Temperature Management (TTM) as deemed medically necessary. For those patients requiring a Head CT, Targeted Temperature Management may be initiated prior to receiving the Head CT. Note: Determination of Neurologic Prognosis is unreliable before at least 72 hours after ROSC. Do not neuroprognosticate until 72 hours post rewarming. Note: Please document in the Comment section of Sunrise: time/date TTM initiated, target temperature reached, rewarming initiated, normothermia reached. If TTM is initiated in the Emergency Department please document time/date TH was initiated in the ED during RN report. Exclusion/Contraindications: Note: These are exclusion criteria only. If the patient is not excluded by these criteria, TTM should be performed on a case by case basis, unless contraindicated. > 12hrs since Return of Spontaneous Circulation (ROSC) (Data support cooling patients as soon as possible post-cardiac arrest) Glasgow Motor score >5 Minimal pre-morbid cognitive status Other reason for comaintracranial pathology (i.e. intracranial hemorrhage, ischemic stroke), subarachnoid hemorrhage (SAH), sedation 1 9/1/13 Sepsis as etiology for arrest DNAR B & C/DNAI status (for TTM only) Uncontrollable bleeding Significant trauma, especially intra-abdominal such as splenic or liver laceration (due to increased risk of bleeding) Equipment List Arterial line kits (both radial and femoral) PreSEP central venous catheter Two one liter bags of 0.9% NaCl at 4 degrees Celsius Gaymar III external cooling system o One Gaymar torso and two thigh cooling pads Temperature probe foley catheter with appropriate adapter for cooling device or alternative temperature monitoring device Neuromuscular blockade equipment o Peripheral Nerve Stimulator (See TTM specific TOF policy) o Consider use of BIS monitor and sensor for monitoring sedation Fluid warmer if needed Sedation/Anesthetic/Neuromuscular Blocker (NMB) Should administer one or more of the following: Fentanyl Injection 50 mcg IV every hour as needed for pain. If using BIS monitor, titrate to 40-60. Fentanyl IV infusion NSS (8000mcg/250mL). Administer per ICU protocol (Critical Care Nursing Policy CCC-05-05). If using BIS monitor, titrate to 40-60. Propofol IV infusion (1000mg/100ml). If using BIS monitor, titrate meds to keep BIS 4060. Administer per ICU protocol. Max rate of 80 mcg/kg/min. Note: Propofol interferes with measurement of aPTTs. Please consider this when ordering propofol on patients already on heparin and use Factor Xa levels to monitor anticoagulation Lorazepam IV infusion (2mg/ml). Administer per ICU protocol. If using BIS monitor, titrate to 40-60. Lorazepam Injection 1 mg IV every 2 hours as needed for agitation. If using BIS monitor, titrate to 40-60. Pancuronium IV infusion NSS (100mg/250 ml) Administer per ICU protocol (Critical Care Nursing Policy BCC-03-26; Use TTM TOF protocol for titration). Initiate pancuronium before initiating cooling. Dosing recommendations: 0.1 mg/kg loading dose followed by a continuous infusion of 0.33-2 mcg/kg/minute. *Do not use in patients with renal and/or hepatic insufficiency. Cisatracurium IV infusion (200mg/250ml). Administer per ICU protocol (Critical Care Nursing Policy BCC-03-26; Use TTM TOF protocol for titration). Initiate cisatracurium 2 9/1/13 before initiating cooling. Dosing recommendation: 0.1-0.2 mg/kg loading dose followed by a continuous infusion of 0.5-10 mcg/kg/min. Can be used in patients with renal insufficiency defined as a creatinine clearance <10 ml/min and/or hepatic insufficiency defined as total bilirubin >3mg/dl associated with liver disease or dysfunction. Ophthalmic Lubricant Ointment 3.5gm – Dose 1 application both eyes every 2 hours for: Eye Lubrication Prophylaxis. Nursing Cooling o Infuse 2 liters 0.9% NaCl at 4 C over 30 minutes if no evidence of Pulmonary Edema; See Critical Care Nursing Policy: Post cardiac arrest therapeutic hypothermia (TTM) policy BCC-04-05 o Insert intra-vesicular (bladder) catheter with temperature probe - Bard Temperature Sensing Foley 400 Series (product #90911616 – no minimum urine output required for use). If bladder temperature is not available or inaccurate consider alternative site (i.e. esophageal probe). NOTE: If bladder pressure is being measured it is recommended that an esophageal probe be used for temperature monitoring. o Goal temperature of 32-34º C as soon as possible (within 4 hours) If using BLUE-faced Gaymar III set to Automatic mode, set point 33º Rapid mode, for 24 hours from time target temperature reached. If using GRAY-faced Gaymar III set to Automatic mode, Rapid cooling, set point 34ºC. Once the patient reaches 34ºC set to Gradual mode at 33ºC Note: Please document in the Comment section of Sunrise: time/date TTM initiated, target temperature reached. If TTM is initiated in the Emergency Department please document time/date TH was initiated in the ED during RN report. Re-warming o Initiate 24 hrs after target temperature was reached per RN policy o Caution: check blood sugar prior to rewarming. Monitor for hypoglycemia during the rewarming phase. o Rewarm to 37° C o If using BLUE-faced Gaymar III with Automatic re-warming algorithm, set to Automatic mode, set point 37º Moderate mode. The moderate mode will increase the set point automatically 0.33° every hour (~12 hours). 3 9/1/13 o If using GRAY-faced Gaymar III with Manual re-warming, set to Manual mode and manually increase the blanket temperature 0.33ºC every 1 hour until the patient temperature reaches 36ºC. o Hold all K+ containing fluids if K+ > 3.5 immediately before and during rewarming o Change IV fluids to 0.9% NaCl, titrate to CVP >8 mmHg, maintaining a MAP > 80 mmHg, and no evidence of shock (by exam, urine output, lactate, and ScvO2) o Stop NMB infusion after core temperature reaches 36° C o Meperidine 12.5-25 mg q4-6 hrs IVP (but not to exceed 100 mg/day) can be used to treat shivering once NMBs have been stopped (if renal failure or oliguria is not present and patient not taking an MAO inhibitor or SSRI). Warning: Should NOT be given at all in late term pregnancy or for prolonged use at any time during pregnancy. Caution: there is a potential interaction between Meperidine and Buspirone although no known cases of an interaction have been documented in the literature. o Maintain active normothermia for 48 hours: keep cooling wraps on the patient for 48 hours after rewarming and administer acetaminophen around the clock for the same 48 hour time period. Monitor skin breakdown closely during this time. Note: Acetaminophen should not be administered in patients with fulminant hepatic failure. Use caution in patients with chronic liver disease or acute liver injury. Consider decreased dosing in this patient population, not to exceed 2 grams daily. Note: Please document in the Comment section of Sunrise: time/date rewarming initiated and normothermia reached. Post Cardiac Arrest Early Goal Directed Therapy IV Fluids Note: If Acute Coronary Syndrome suspected, first transfuse blood to Hgb ≥10. Patient with MAP < 80 mmHg: 0.9% NaCl IV x 2 liters – titrate to CVP >8 mmHg, until MAP > 80 mmHg and ScvO2 greater than or equal to 65%, unless signs of pulmonary edema If K less than 5, switch to Lactated Ringers (provided no contraindications, i.e. advanced liver disease, increased potassium) after 2 liters 0.9% NaCl infused (This includes the 2 L cold saline for initiation of TTM) - titrate to CVP >8 mmHg, until MAP 4 9/1/13 > 80 mmHg and ScvO2 greater than or equal to 65% unless signs of pulmonary edema If ScvO2 < 65% and/or any signs of shock, with no pulmonary edema: continue with 0.9% NaCl boluses up to a total of 2 liters and titrate to CVP >8 mmHg and Scv02 greater than or equal to 65%. Note: If showing signs of pulmonary edema consider stopping fluid resuscitation. If no signs of pulmonary edema and additional resuscitation needed, continue with Lactated Ringers if K+ less than 5.0 mEq/l Note: Consider monitoring Intra-abdominal pressure if > 5 liters of IVF given in 24 hours Vasoactive Agents -If hemodynamically unstable, STAT echocardiogram to determine Ejection Fraction Hypotension, Ejection Fraction greater than or equal to 50% o Norepinephrine infusion: Begin at 2-4 mcg/min, titrate to maintain MAP >7080 mmHg Hypotension, Ejection Fraction less than 50% o Norepinephrine infusion: Begin at 2-4 mcg/min, titrate to maintain MAP >7080 mmHg; (max infusion rate 60 mcg/min) o Begin Dobutamine infusion at 2.5 mcg/kg/min to maintain a MAP of >70-80 mmHg and/or ScvO2 >65%; (max infusion rate 20 mcg/kg/min). o Begin Epinephrine infusion at 2 mcg/min to maintain ScvO2>65% (max infusion rate of 20 mcg/min). Note: If the above therapies fail and hypotension severe, consider Intra-aortic balloon pump ScvO2 (by co-oximetry) < 65% with CVP 15-20 mm Hg or CHF o If MAP is < 60 mmHg, begin norepinephrine infusion: Begin at 2-4 mcg/min, titrate to maintain MAP >70-80 mmHg. o Begin Dobutamine infusion at 2.5 mcg/kg/min to maintain ScvO2 >65% (max infusion rate 20 mcg/kg/min) o Consider transfusing Packed Red Blood Cells to keep Hemoglobin greater than or equal to 10 g/dL once CHF clears Hypertension Begin Nitroglycerin infusion at 10 mcg/min (max 200 mcg/min) for MAP >100 mmHg - titrate to MAP goal Hypertension with tachycardia or acute ischemia/MI without LV dysfunction: Initiate Esmolol and titrate to HR <100. Initiate 50 mcg/kg/min, increase by 50 mcg/kg/min increments to max rate of 300 mcg/kg/min 5 9/1/13 Initial Laboratories Beta HCG on all women of childbearing age ABG with Ionized Calcium and Magnesium CBC/ platelets / PT / PTT/INR, Fibrinogen Electrolyte “panel 7”, plus iCa / Mg / Phos , Cl-, Glucose Amylase, Lipase Liver Function Panel Lactate, CPK-MB, CK, Troponin Cortisol level (If Indicated) Pan-culture - Blood Culture, Urine Culture, Urinalysis, Sputum Culture (if appropriate) Toxicology screen if appropriate Co-oximetry on Central Venous blood Serial Laboratories: Note: For ABG and Co-oximetry Panel: Do not temperature correct. ABG q 6 hrs and prn Co-ox (Central Venous) q 1-2 hrs for first 6hrs – then q 6 hrs - until re-warming process complete if continuous Sv02 catheter not used Glucose, K+, and lactate q 6 hrs - until re-warming process complete Repeat CPK-MB, CK, Troponin q 6 hrs - until re-warming process complete CBC/ PT / PTT/INR, fibrinogen, P7 / Ca / Mg / Phos q 6 hrs Monitoring: Continuous EEG monitoring - page EEG fellow at 215-404-6771 before midnight if possible; EEG must be hooked up within 6-12 hours of TH initiation. EEG should not be discontinued until the patient is re-warmed and paralytics are discontinued. For issues or concerns, if you cannot get a hold of the EEG fellow, please page the Neurology resident on-call. 6 9/1/13 See EEG “quick sheet” in the appendices. This is for educational purposes only. Core Temperature - continuous CVP q 1hour with Vital Signs during active cooling/re-warming; q 4 hours during maintenance Check patient skin (especially under the wraps) q 4 hours When clinically appropriate, consider SSEP ordered on day 3 (72 hours postROSC) - Place order for Somatosensory Evoked Potential in Sunrise with a note that states “post-cardiac arrest” or for questions call the lab at 215-662-2661. Nutrition – NPO Insert OG tube, keep Head of Bed (HOB) greater than 30 degrees at all times and follow Gastric Residuals per ICU protocol X-ray to confirm placement of OGT Electrolytes Potassium Chloride (40 mEq in 100ml) 40 mEq in normal saline – 100 ml IV piggyback Every 6 hours PRN Hypokalemia less than 3.4. Note: For patients with renal insufficiency, call MD for adjusted dosing. -For potassium >3.5 mmol/L while rewarming Do Not Replete -For potassium 3.0-3.5 mmol/L: 40 meq/100 mLs SWFI (infuse over 2 hrs) -For potassium 2.5-3.0 mmol/L: 60 meq/150 mls NaCl 0.9% (infuse over 3hrs) -For potassium <2.5 mmol/L: 80 meq/L – Infuse each 40meQ/100 mLs SWFI over 2 hours Magnesium Sulfate Injection 1 gm Intravenous in D5W – 100 ml IV piggyback Every 6 hours PRN Hypomagnesemia (less than 1.8 mg/dL) Calcium Chloride Injection 1 gm in D5W – 100 ml Intravenous piggyback Every 4 hours As needed for ionized calcium levels less than 0.9. If repleting, check ionized calcium levels every 4 hours Sodium Phosphorus Infusion 7 9/1/13 10 mMol(s) in sodium chloride 0.9% - 500ml IV piggyback every 6 hours PRN Hypophosphatemia less than 2.5 mg/dL. -For phosphate levels > 2.5 mg/dL – No Replacement Needed -For phosphate levels 2.0-2.5 mg/dl – Infuse Sodium Phosphate 10 mmol/100 mLs sodium chloride and infuse over 4 hours -For phosphate levels <2.0 mg/dl – Infuse Sodium Phosphate 20 mmol/250 mLs sodium chloride and infuse over 6 hours Blood Products Education: if significant bleeding ensues while hypothermic, coagulopathy should be corrected aggressively. In the absence of overt bleeding, the decision to correct coagulopathy is up to clinical judgment after weighing the risks and benefits of blood product replacement in each individual case. Note: PRBC: Transfuse 1-2 PRBC to Hgb > or = 10 for patients with ACS or shock with ScvO2 less than 65, after correction of low CVP and MAP. Platelet count < 20K or <50K with active bleeding: Platelets 6 units With active bleeding - INR > 1.5: FFP _____2 units ____4 units PRBC for ACS or any evidence of shock despite CVP>8-12 mm: ____1 unit ____ 2 units PRBC for Hgb < 7: _____1 unit ____2 units PRBC for Hgb < 10 if active bleeding: _____1 unit ______2 units PRBC Pre-medications for PRBC & Platelets (unless hypothermic) Choose appropriate Acetaminophen and Diphenhydramine Dose and Route: Acetaminophen Liquid 160 mg/5ml - Give 650mg Orogastric Tube Once – Total Per Dose 650 mg Acetaminophen Supp 650 mg – Total Per Dose 650 mg Diphenhydramine 25 mg IV Once – Total Per Dose 25 mg Diphenhydramine Liquid 25mg/10ml - Give 25 mg Orogastric Tube Once – Total Per Dose 25 mg Insulin Therapy Initiate per HUP/ICU Insulin Infusion Protocol for two consecutive blood glucoses > 150 mg/dL Caution: check blood sugar prior to rewarming. Monitor for hypoglycemia during the rewarming phase 8 9/1/13 Respiratory If ALI/ARDS use Low Stretch protocol Arterial pH Goal: 7.30 – 7.45. FiO2 Goal is < .70. Wean FiO2 and maintain for SaO2>92% or <95% or PaO2> 85 mmHg and <110mmHg Ventilator Modes – Low stretch protocol: Use patient height to calculate Tidal Volume (TV) per Predicted Body Weight (PBW) and gradually reduce TV to 6 ml/Kg/PBW; monitor and maintain plateau pressure ≤30 cm H20 Radiology CXR now Repeat CXR in AM and after 72 hours Head CT to rule out intracranial hemorrhage, or other causes of coma, if clinically appropriate Cardiology Call Cardiology for: o hemodynamic instability, indeterminate ECG or suspected Non-STEMI, or arrhythmia (use Cardiology Consult pager) o Acute STEMI (Use STEMI Activation Cell Phone) ECG STAT ECG q 8 hours x 2 Echo -Consider early Echo if requested by Cardiology Consult, or in the case of any of the following: -Ongoing hypotension with possible cardiac etiology -Ongoing arrhythmias -Indeterminate ECG Or, obtain routine Echocardiogram within first 24-48 hours of protocol Repeat echocardiogram 24-48 hours Aspirin: _300___mg per rectum OR _325__mg OG STAT Once for Acute Coronary Syndrome, unless contraindicated (i.e. allergy or active bleed) DVT Prophylaxis Heparin 5000 units SubQ q8 hrs Intermittent Compression Stockings 9 9/1/13 GI Prophylaxis ranitidine oral liquid 15 mg/ml solution – 150 mg orogastric tube ranitidine IVPB, 50 mg IV piggyback Shivering Meperidine 12.5-25 mg q4-6 hrs IVP (not to exceed 100 mg) can be used to treat shivering once NMBs have been stopped (if renal failure or oliguria isn’t present and patient not taking an MAO inhibitor, or SSRI). Warning: Should NOT be given at all in late term pregnancy or for prolonged use at any time during pregnancy. Caution: there is a potential interaction between Meperidine and Buspirone although no known cases of an interaction have been documented in the literature. Consults Cardiology consult for: - hemodynamic instability, indeterminate ECG or suspected Non-STEMI, or arrhythmia (use Cardiology Consult pager) - Acute STEMI (Use STEMI Activation Cell Phone) Neurology for all post cardiac arrest patients Nutrition Support Services on day 3 Maternal-Fetal Medicine if + HCG (while initiating hypothermia) Resuscitation consult team – 267.253.9035 Utilize Nursing Policy BCC-03-26 Neuromuscular Blockade (NMB) Therapy for guidance on use of peripheral nerve stimulator and train-of-four (TOF) monitoring. Use algorithm below for NMB dose titration in Targeted Temperature Management. 10 9/1/13 Therapeutic goal: Prevention of shivering. Patients may initiate breaths on ventilator without shivering occurring. NOTE: Lower doses of NMBs are effective to prevent shivering. Consider increased doses of NMB to paralyze diaphragm when there is need to decrease oxygen consumption, decrease plateau pressures or hypoxemia is present. Determine baseline TOF Administer loading dose Begin infusion Recheck Train of Four in 1 Hour TOF 0/4 Decrease dose of infusion by 10% Recheck in 1hr TOF 1-2/4 Therapeutic goal met: No change TOF 3-4/4 or 1-4/4 and shivering Therapeutic goal NOT met: Administer ordered bolus dose infusion by 25%; Recheck in 1hr TOF 0/4 Decrease dose of infusion by 10% Recheck in 1hr* TOF 1-2/4 Therapeutic goal met: No change TOF 1-4/4 and shivering Therapeutic goal NOT met: TOF 3-4/4 or 1-4/4 and shivering Therapeutic goal NOT met: Administer ordered bolus dose infusion by 25% Recheck in 1hr Administer ordered bolus dose infusion by 25% Recheck in 1hr *Continue to decrease dose by 10% until evidence of shivering is present or minimum recommended dose in dosing range is reached. Do not discontinue drug. 11 9/1/13 12 9/1/13 13 9/1/13 14 9/1/13 15 9/1/13 16 9/1/13 17 9/1/13 18