Belatacept Conversion Protocol
advertisement
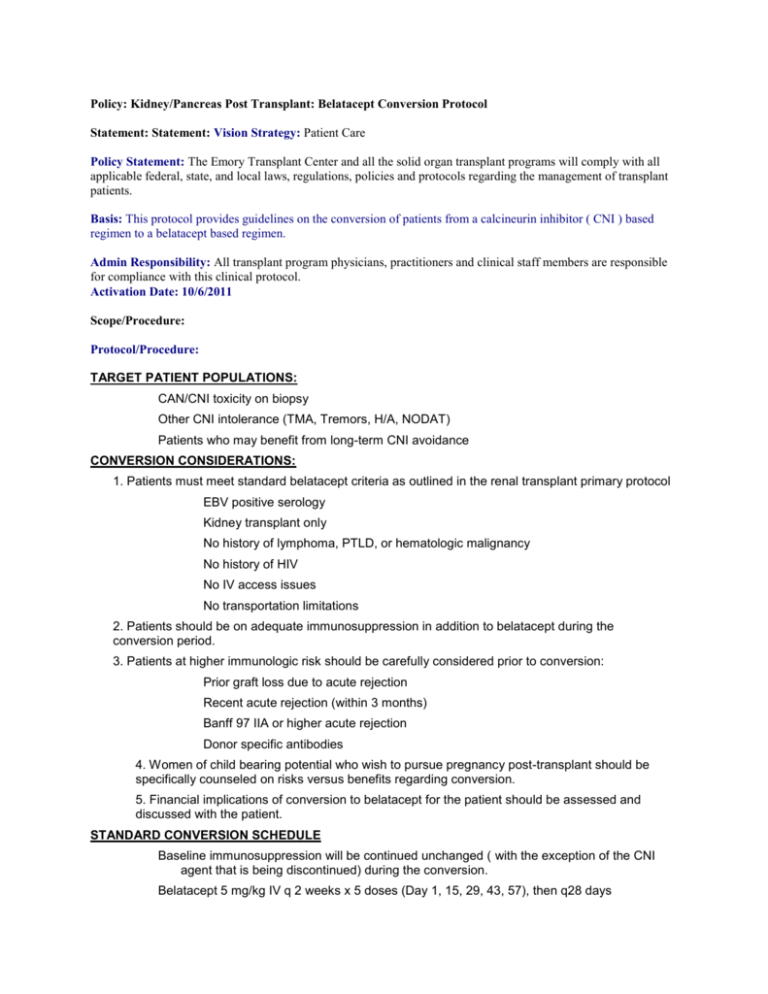
Policy: Kidney/Pancreas Post Transplant: Belatacept Conversion Protocol Statement: Statement: Vision Strategy: Patient Care Policy Statement: The Emory Transplant Center and all the solid organ transplant programs will comply with all applicable federal, state, and local laws, regulations, policies and protocols regarding the management of transplant patients. Basis: This protocol provides guidelines on the conversion of patients from a calcineurin inhibitor ( CNI ) based regimen to a belatacept based regimen. Admin Responsibility: All transplant program physicians, practitioners and clinical staff members are responsible for compliance with this clinical protocol. Activation Date: 10/6/2011 Scope/Procedure: Protocol/Procedure: TARGET PATIENT POPULATIONS: CAN/CNI toxicity on biopsy Other CNI intolerance (TMA, Tremors, H/A, NODAT) Patients who may benefit from long-term CNI avoidance CONVERSION CONSIDERATIONS: 1. Patients must meet standard belatacept criteria as outlined in the renal transplant primary protocol EBV positive serology Kidney transplant only No history of lymphoma, PTLD, or hematologic malignancy No history of HIV No IV access issues No transportation limitations 2. Patients should be on adequate immunosuppression in addition to belatacept during the conversion period. 3. Patients at higher immunologic risk should be carefully considered prior to conversion: Prior graft loss due to acute rejection Recent acute rejection (within 3 months) Banff 97 IIA or higher acute rejection Donor specific antibodies 4. Women of child bearing potential who wish to pursue pregnancy post-transplant should be specifically counseled on risks versus benefits regarding conversion. 5. Financial implications of conversion to belatacept for the patient should be assessed and discussed with the patient. STANDARD CONVERSION SCHEDULE Baseline immunosuppression will be continued unchanged ( with the exception of the CNI agent that is being discontinued) during the conversion. Belatacept 5 mg/kg IV q 2 weeks x 5 doses (Day 1, 15, 29, 43, 57), then q28 days CNI dose reduction at Day 15, discontinuation at Day 29 Day 1: Belatacept 5mg/kg IV over 30 min Continue CNI at current dose (baseline) Baseline labs Provide infusion schedule and CNI withdrawal plan to patient Day 15: Belatacept 5mg/kg IV over 30 min Decrease CNI by 40-60% of baseline dose Labs Day 29: Belatacept 5mg/kg IV over 30 min Discontinue CNI Labs Day 43: Belatacept 5mg/kg IV over 30 min Labs Day 57: Belatacept 5mg/kg IV over 30 min Labs Continue belatacept 5mg/kg IV every 28 days thereafter RAPID CONVERSION SCHEDULE Baseline immunosuppression will be continued unchanged ( with the exception of the CNI agent that is being discontinued) during the conversion. Consider rapid conversion in patients with evidence of TMA or acute CNI toxicity. Belatacept 10 mg/kg IV x 1 dose (Day 1), then belatacept 5 mg/kg IV q 2 weeks x 4 doses (Day 15, 29, 43, 57), then q 28 days CNI dose reduction at Day 1, discontinuation at Day 15 Day 1: Belatacept 10mg/kg IV over 30 min Decrease CNI by 40-60% of baseline dose Baseline labs Provide infusion schedule and CNI withdrawal plan to patient Day 15: Belatacept 5mg/kg IV over 30 min Discontinue CNI Labs Day 29: Belatacept 5mg/kg IV over 30 min Labs Day 43: Belatacept 5mg/kg IV over 30 min Labs Day 57: Belatacept 5mg/kg IV over 30 min Labs DOSING OF BELATACEPT FOR CONVERSION Available as lyophilized powder 250mg vial size Rounding doses to minimize wastage and reduce errors Administration Over 30 minutes via peripheral IV through a low protein binding filter (pore size of .2-1.2 um) Admixed doses may be stored refrigerated for up to 24hours protected from light Cannot be infused with other agents – no data available REMS requirement Medication Guide must be given to patient before EVERY infusion Patient asked for any signs and symptoms of infection or CNS ADR’s Pre-infusion checklist to be documented in EeMR under Clinical Notes: Transplant Note or Transplant Nursing Note