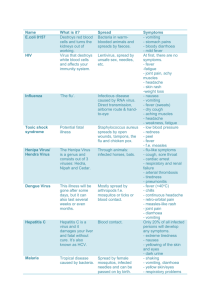
Viral infections fact sheet
advertisement

VIRAL INFECTIONS Herpes Simplex virus (H): Family HSV-1 and -2 Epidemiolgoy 15% women at antenatal clinic have HSV-2, 55% at STD clinics Spread Can be via birth canal; 1+2 both implicated in STD Pathogenesis Incubation 2-12/7 Replicated in skin and mms vesicular lesions; spread to sensory neurons latent infection; reactivation spread of virus from neuron to skin Symptoms May interchange sites; cannot differentiate 1 and 2 clinically; painful, recurrent, preceded by burning/numbness clustered vesicles, blistering, crusting; recurrence precipitated by stress, menstruation, ill health; heal over 2/52; may get 2Y bacterial infection HSV 1 Cold sores; blisters, Gingivostomatitis, tongue to retropharynx, herpetic whitlow; milder and less recurrent; usually not STD HSV 2 Genital herpes: vesicles superficial ulcerations; dysuria, urinary f Neonate: 40% exposed fetuses suffer serious perinatal morbidity; splenomegaly, necrotic foci in lungs, liver, adrenals, CNS Pregnant: trt with acyclovir if severe 1Y genital herpes; complications = prem, abortion, IUGR, neonatal infection; acyclovir can cause fetal renal damage Immunosupp: eczema herpecticum, bronchopneumonia, hepatitis, Kaposi’s sarcoma, encephalitis Other: Keratitis History: sexual contact Examintion: look for evidence of other STD’s Investigations Immunofluorescence: 80% sens, high spec Viral culture: 70% sens for vesicle fluid, 25% sens for crusted lesions; 100% spec PCR: high sens and spec Treatment STD counseling; mng partners; mng other STD’s 1Y genital: antivirals decr duration of shedding, decr time to crusting and healing, decr duration of constitutional Sx, decr local pain; always trt 1Y illness; acyclovir 400mg PO TDS for 5/7 (4-10x more sens to acyclovir than VZV) Recurrent genital: recommended if start within 72hrs Sx onset; same as above Long term suppression: if >6 episodes/yr; decr recurrence by 70-80%; still can be infective; acyclovir 200mg BD for 6/12 If disseminated: requires strict isolation Gingivostomatitis: topical trt doesn’t change natural history of disease; PO hastens time to healing Keratitis: 3% acyclovir ointment 5x/day for 2/52; see ophthalmology within 24hrs Neonatal / herpes encephalitis: acyclovir 10mg/kg IV TDS for 2/52 Family Herpes virus 3 Epidemiology 90% population have prev VZV infection Shingles: annual incidence 1:100; affects up to 50% patients >85yrs Spread Aerosol; epidemic Pathogenesis Infects mms, skin, neurons chickenpox latent infection in dorsal sensory ganglia reactivates (due to decr cell mediated immunity) travels to dermatomes shingles Symptoms Chickenpox (varicella zoster); mild in children, severe in adults and immunocompromised; rash 2 weeks after resp infection; may rarely cause interstitial pneumonia, encephalitis, transverse myelitis necrotising visceral lesions; Macule vesicle rupture crust heal with no scars unless bacterial superinfection Shingles (herpes zoster): usually occurs only once in immunosuppressed / elderly; rarely geniculate nucleus invovled --> Ramsay-Hunt syndrome, with facial paralysis; prodrome (pain, burning, headache, malaise) precedes rash by 2-3/7 dermatomal rash, vesicles at 3-5/7, crusts at 7-10/7, heals in 2-4/52 Herpes zoster opthalmicus: sight threatening Post-herpetic neuralgia: 10% incidence; precipitated by touch; lasts 3/12 (longer if >60yrs, triG nerve, severe, immunosupp, DM) Investigations Swab lesion if uncertain diagnosis Treatment Chickenpox: can give vaccine / Ig to exposed contacts; no different in pregnancy; highest risk if fetus infected 13-20/40 (only occurs in 2% non-immune women) IUGR, cutaneous scarring, limb hypoplasia, cerebral cortical atrophy; if immunocomp, 5-20% risk of death Antivirals if: immunocomp; causes decr pain and fever, decr risk of dissemination and decr time to healing; given 10mg/kg acyclovir TDS for 7-10/7 Shingles: isolate from high risk patients until lesions dry (eg. <1yrs, immunosupp, preg); saline baths TDS; analgesia Antivirals if: ophthalmic, immunocomp, >50yrs, <72hrs since onset; decr no vesicles, decr time to resolution, decr duration post-herpetic neuralgia; acyclovir 800mg 5x/day 1/52 Steroids: may help analgesia; give if >50yrs; 50mg pred OD 1/52 then taper HZV opthalmicus: give acyclovir 800mg 5x/day PO 1/52; may supplement with TOP; will decr complication rate and acute pain; see ophthalmologist within 24hrs Post-herpetic neuralgia: analgesia; amitryptiline 10-25mg PO nocte, gabapentin 300mg OD, opioids, pain centre referral Family Herpes virus 4 Spread Saliva Pathogenesis In nasopharyngeal and oropharyngeal lymphoid tissues esp tonsils infection of B cells; Infects >90% humans Symptoms Symptoms primarily due to immune response In infants and children: asymptomatic / non-specific Infectious mononucleosis – benign, self-limited; lymphoproliferative disorder; >50% have fever, LN’s and pharyngitis; 70-90% get morbilliform rash with amoxycillin; Splenomegaly (>10%; may get rupture), hepatomegaly (>10%), meningoencephalitis / GBS, pneumonitis, palatal petechaie, myocarditis, pancytopenia --> resolves in 4-6/52; Hairy leukoplakia, neoplasms (eg. Burkitt lymphoma (>90%), nasopharyngeal Ca (nearly 100% 2Y to EBV), VZV (H): EBV = GLANDULAR FEVER / IMN (G) Hodgkin’s disease (in 40-60%)) Investigations Heterophile ab tests – Monospot (85% sens); false –ive early EBV specific ab tests – IgM/G; 97% sens FBC: incr WBC, incr peri mononuclear cells, atypical lymphocytes LFTs – incr AST/ALT Treatment Supportive Family Herpes virus 5 Spread Transplacental; breast milk; saliva; veneral, resp secretions and fecal-oral in teenagers (infected people secrete virus in body secretions for months); organ transplants and blood transfusions Pathogenesis Infects and latent in WBC; can be reactivated; asymptomatic excretion persists for years Symptoms Usually asymptomatic in healthy / glandular fever-like illness (fever, atypical lymphocytosis, lympadenopathy, Hepatomegaly, abnormal LFT’s) Serious in neonates and immunocompromised Congenital – 95% asymptomatic; may get cytomegalic inclusion disease (IUGR, jaundice, hepatosplenomegaly, anaemia, bleeding, thrombocytopenia, encephalitis, hearing loss, pneumonitis, hepatitis); similar to toxoplasmosis Perinatal – usually asymptomatic; pneumonitis, FTT, rash, hepatitis In immunosuppressed –reactivation of latent virus; pneumonitis, colitis, retinitis, renal dysfunction Investigations Antibodies; urine culture Treatment Supportive If life / sight-threatening – ganciclovir (may be used as prophylaxis in advanced HIV) Prophylactic acyclovir in post-tranplant Family Toxoplasma gondii; obligatory intracellular protozoan Spread Transplacental; undercooked meat; contaminated soil (cats) RF: immunocompromise, congenital transmission Pathogenesis Tissue cysts form in cat’s intestines; oocytes shed in cat’s faeces Symptoms Often asymptomatic Congenital: 50% risk of fetal effects in maternal infection; miscarriage, chronic chorioretinitis; severe jaundice, hepatosplenomegaly, thrombocytopenic purpura, seizures, hydrocephalus, mental retardation Acquired: usually asymptomatic / benign; infectious mononucleosis-like; posterior uveitis Immunocompromised: rash, fever, rigors, encephalitis, hepatitis, pneumonia, myocarditis; acute severe infection in 40% AIDS patients Investigations IgM – in first 1-2/52; peak 4-8/52 IgG – slow rise; peak 4-8/52; remain for years Ab’s less useful in immunocompromised CT/MRI – ring enhancing lesions; oedema in basal ganglia / cortico-medullary junction Treatment Treat if: neonate, pregnancy (beware if 1st trim, sulphonamides cause congenital abnormalities, but so does toxoplasmosis), immunocompromised, organ dysfunction, persisitent severe Sx Pyrimethamine 25-50mg/day for 3-4/52 Give folate to prevent haematological toxicity If cerebral in AIDS: sulfadiazine 1 – 1.5g IV Q6hrly + pyrimethamine Disposition Poor prognosis if fetal 1st trimester; good if 3rd trim or post-natal; often fatal in immunocompromised Cytomegalovirus (G) Toxoplasmosis (G) Measles – see paeds Mumps Family Paramyxovirus Spread Resp droplets Pathogenesis Spread to LN’s in lymphoctes blood glands Symptoms Salivary gland pain and swelling; can spread to CNS (aseptic meningitis), testis, ovary, pancreas Investigation Treatment Disposition Poliovirus Family Enterovirus Spread Faecal-oral Pathogenesis Oropharynx multiplies in intestinal mucosa and LN, transient viraemia and fever CNS via blood Symptoms Asymptomatic usually; 1/100 invade CNS motor neuron of SC / brainsteam flaccid paralysis Investigation Treatment Only briefly shed; fecal-oral route Disposition Viral Haemorrhagic Fevers Family Adenavirus, filovirus, flavivirus Spread Insect host Pathogenesis Endothelial cell infection; Neutropenia, low plt, severe plt dysfunction, endothelial dysfunction, incr vascular permeability; necrosis and hameorrhage of organs; DIC Symptoms Fever, haemorrhag,e headache, myalgia, rash shock Investigation Treatment Supportive Disposition HPV Family Papovavirus Spread Skin and genital contact Pathogenesis Infect epithelial cells Symptoms Warts, benign squamous tumours, SCC cervix and anogenital Investigation Treatment Skin and genital contact Disposition Norovirus Family Spread Contact; food; commonest food-bourne viral infection Pathogenesis Symptoms Onset 12-24hrs; D+V; offset 2/7 Investigations Treatment Disposition Rotavirus Family Spread Contact; faecal contamination of food; commonest cause of food poisoning in infants Pathogenesis Symptoms V; watery D; fever Investigations Treatment Disposition VIRAL INFECTIONS Obligate intracellular parasites that depend on host cell's metabolic machinery for replication; nucleic acid genome surrounded by protein coat (capsid) that may be encased in lipid membrane; can be latent (eg. Herpes zoster in dorsal root ganglia); may transform host cell into tumour (eg. HPV) Pathogen Family Genomic Type Presentation Adenovirus Adenoviridae DS DNA URTI, LRTI, conjunctivitis, diarrhoea Rhinovirus Picornaviridae Respiratory Coxsackievirus URTI SS RNA Pleurodynia, herpangina, hand-foot-and-mouth disease, SARS Coronavirus Coronaviridae URTI Influenza A+B Orthomyxoviridae Influenza RSV Paramyxoviridae Bronchiolitis, pneumonia Mumps Paramyxoviridae Mumps, pancreatitis, orchitis Norwalk agent Caliciviridae Gastroenteritis Hep A Picornaviridae Digestive Acute hepatitis SS RNA Hep D Viroid-like Acute/chronic hepatitis Hep C Flaviviridae Hep E Norwalk-lik Rotavirus Reoviridae DS RNA Diarrhoea Hep B Hepadnaviridae DS DNA Acute / chronic hepatitis Enterically transmitted hepatitis Systemic with skin eruption Measles Paramyxoviridae Rubella Togaviridae Parvovirus Parvoviridae Vaccinia Poxviridae VZV HSV 1 Herpesviridae SS RNA SS DNA Measles German measles Erythema infectiosum, asplastic anaemia Smallpox vaccine DS DNA HSV 2 Chickenpox, shingles Cold sore Genital herpes Systemic with haematopoietic disorder CMV EBV HTLV-1 HIV-1 and 2 Herpesviridae DS DNA Retroviridae SS RNA Cytomegalic inclusion disease Infectious mononucleosis Adult T-cell leukaemia, tropical spastic paraparesis AIDS Arboviral and haemorrhagic fevers Dengue virus 1-4 Yellow fever virus Dengue, haemorrhagic fever Togaviridae SS RNA Regional Filoviridae / haemorrhagic fever hantavirus Yellow fever Ebola, Manburg disease Warty Growths Papillomavirus Papovaviridae DS DNA Condyloma, cervical Ca Poliovirus Picornaviridae SS RNA Poliomyelitis JC virus Papovaviridae DS DNA Progressive multifocal leukoencephalopathy Arboviral encephalitis Togaviridae SS RNA CNS