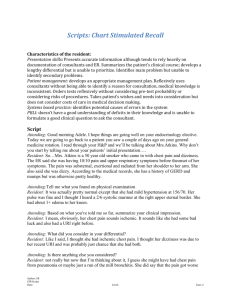
Resident: Hey doc. It`s ok. I have an awesome intern, makes life
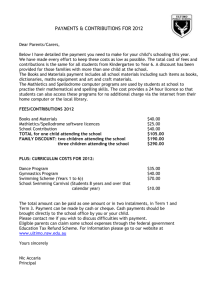
advertisement

Scripts: Chart Stimulated Recall Script Attending:Hi Rich, have a seat. How are you? How are the floors? Resident: Hey doc. It’s ok. I have an awesome intern, makes life easier for me, you know? Attending: Oh, I can understand that. Well, great, let’s get down to it, shall we? (Resident nods). I’ve looked at the H and P that you sent me for this patient. In your own words, could you tell me about this patients’ initial presentation? Resident: Yeah. The patient came to us through the ED. He is a 42 year old, with a history of end stage renal disease, started on HD maybe a year ago. He presented with left sided chest pain which is associated with a cough, and dyspnea on exertion. He developed all these symptoms about a week ago, and they’ve been getting worse, to the extent that he can’t walk more than a quarter block before he has to stop to catch his breath. The pain he says is there all the time, but gets worse with coughing. He has also had subjective fever, with chills and fatigue. He’s been coughing up yellow sputum. He does have a history of CAD, had a CABG some years ago, and has hypertension that’s not well controlled. He doesn’t miss his dialysis sessions, and did get the flu shot this year, but he doesn’t remember about the pneumonia shot. He’s on all the usual meds, the only thing that concerned me was that he wasn’t on aspirin. He’s pretty compliant, but hasn’t really seen a cardiologist in a long time. No sick contacts, and no recent travel. He’s an ex-smoker, quit a long time ago. His weight has been pretty stable, although lately his appetite has been really poor. Attending: And what did you find on physical exam? Resident:On admission, his blood pressure was actually within normal range, which he tells me is unusual for him. His heart rate was in the 80s, his resp rate was a little high, maybe 24. His sats were about 92% on room air, but he was afebrile. His lungs did have some crackles in the left base, but overall his volume status was ok. I didn’t appreciate a JVD, no peripheral edema, he seemed well nourished. In fact, he seemed a little dehydrated to me, with dry mucous membranes. There was no chest wall tenderness. Attending: How would you summarize your initial clinical impression? Resident: I’d say this is a 42year old man with a history of CAD and end stage renal disease who presented with pleuritic chest pain with fever, with a concern for pneumonia. Attending: What did you consider in your differential? Resident: Given the story, I was really worried about a couple of other things – I wanted to make sure there wasn’t an element of heart failure or ACS. I mean, he’s high risk, given his history of CAD, and of course being on dialysis. Also, he wasn’t on aspirin, still not sure why. Attending: What did you do next? Resident: Well, first I wanted to get an EKG and chest xray. The EKG had some evidence of left ventricular hypertrophy, but no new ST changes. The chest xray did show a left lower lobe opacity, with cardiomegaly. The labs were pertinent for an elevated white count with a left shift, Author:SG CSR Script 5 SOB Date:4/13/15 the trops were negative. His BUN and creatinine were both significantly elevated, above his usual baseline. I also ordered an echo for him to evaluate his ejection fraction. We didn’t seem to have one in our system, and I was worried that there may be some heart failure there. I did get blood cultures and sputum cultures, they haven’t grown out yet. I started him on the usual vanc and cefepime. I did give him some fluids because I felt he was a little dry. Attending: Why did you choose the vancomycin and cefepime? Resident: Because he goes to a hemodialysis center, he’s at risk for HCAP, so I wanted to make sure I covered him for MRSA. Attending: Did you consider consulting another service? Resident: Well, nephrology is on board for the dialysis. I didn’t think we needed infectious disease, it seems a pretty straightforward HCAP scenario, you know. Attending: How have you been monitoring his progress? Resident: Well, symptomatically he’s better. The chest pain has improved. I’m weaning him off his oxygen today. Still waiting for that echo. I’ve had PT work with him, and he’s been able to walk independently without getting short of breath. Attending: How will you decide the patient is ready for discharge? Resident: Once he’s off the oxygen. He was also dropping his blood pressures during HD yesterday, and I think that’s to do with his volume depletion. We’ve topped him up now, so as long as his pressures remain good during his next session, I think he’ll be good to go. Attending: What sort of follow-up will you be arranging for him? Resident: He has a good relationship with his PCP. It was the weekend, so I couldn’t touch base with him, but I’ve left a message for him today to let him know what’s happened with the patient, and to clarify his meds and cardiac history. Of course, if the echo shows anything concerning, I’ll have to plan for a cardiology follow-up I suppose. Attending: Were there any patient or family factors that influenced your decision-making? Resident: Yeah, so he has some interesting family dynamics, mainly to do with finances. This has affected his ability to get his meds in the past, but we worked with case management to ensure he has the right coverage. I’m working on getting his meds delivered to him at home, now that he has a permanent address. I think that will help. Attending: What did you learn from taking care of this patient? Resident: I think the most important thing for me was paying attention to his meds, not overlooking the other problems even though his primary problem is perhaps not related. So I’m treating his pneumonia at the moment, but the heart disease is pretty important. Attending: Knowing what you know now, what, if anything, could you do better to improve your own practice? Resident: I wish I had called his PCP earlier on, it might help in understanding his chronic care. Author:SG CSR Script 5 SOB Date:4/13/15 Attending: Based on this patient's experience, what, if anything, can you do to improve the healthcare system for future patients? Resident: Wouldn’t it be nice if we had access to patient records across the systems? I wish I had access to his PCP’s records. Author:SG CSR Script 5 SOB Date:4/13/15