Attending
advertisement

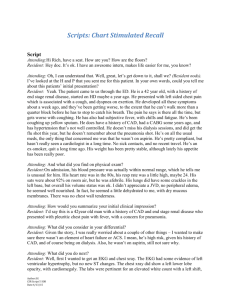
Scripts: Chart Stimulated Recall Characteristics of the resident: Presentation skills: Presents accurate information although tends to rely heavily on documentation of consultants and ER. Summarizes the patient’s clinical course; develops a lengthy differential but is unable to prioritize. Identifies main problem but unable to identify secondary problems. Patient management: develops an appropriate management plan. Reflexively uses consultants without being able to identify a reason for consultation, medical knowledge is inconsistent. Orders tests reflexively without considering pre-test probability or considering risks of procedures. Takes patient’s wishes and needs into consideration but does not consider costs of care in medical decision making. Systems based practice: identifies potential causes of errors in the system PBLI: doesn’t have a good understanding of deficits in their knowledge and is unable to formulate a good clinical question to ask the consultant. Script Attending: Good morning Adele. I hope things are going well on your endocrinology elective. Today we are going to go back to a patient you saw a couple of days ago on your general medicine rotation. I read through your H&P and we’ll be talking about Mrs.Atkins. Why don’t you start by telling me about your patients’ initial presentation…. Resident: So…Mrs. Atkins is a 50 year old smoker who came in with chest pain and dizziness. The ER said she was having 10/10 pain and upper respiratory symptoms before theonset of her symptoms. The pain was substernal, exertional and radiated from her shoulder to her arm. She also said she was dizzy. According to the medical records, she has a history of GERD and mumps but was otherwise pretty healthy. Attending:Tell me what you found on physical examination Resident: It was actually pretty normal except that she had mild hypertension at 156/70. Her pulse was fine and I thought I heard a 2/6 systolic murmur at the right upper sternal border. She had about 1+ edema to her knees. Attending: Based on what you've told me so far, summarize your clinical impression. Resident: I mean, obviously, her chest pain sounds ischemic. It sounds like she had some bad luck and also had a URI right before. Attending: What did you consider in your differential? Resident: Like I said, I thought she had ischemic chest pain. I thought her dizziness was due to her recent URI and was probably just chance that she had both. Attending: Is there anything else you considered? Resident: not really but now that I’m thinking about it, I guess she might have had chest pain from pneumonia or maybe just a run of the mill bronchitis. She did say that the pain got worse Author: SR CSR Script Date: Level: Case: 2 with coughing but it also got worse with exertion which makes me think it is probably cardiac and that the URI is just incidental. Cardiology thought it might be pericarditis so I guess we should put that in the differential too. Attending: What did you do next? Resident: We started the chest pain protocol and ordered some labs and a chest x-ray. Attending: Based on the history and physical findings, what investigations did you order? Resident: You know, the chest pain protocol automatically gets an EKG, cardiac enzymes and routine labs. We also got a BNP in case the pain was related to heart failure. I got a chest x-ray too. Attending: Why? Resident: Well all of those are pretty routine tests if you’re worried about ischemia. The trops look for recent myocardial damage and the chest x-ray to rule out pneumonia. Attending: What did you find? Resident: her troponins were elevated at 3 and peaked at 5. Her MB was mildly elevated too. She had ST elevation leads I through 5 and V1, AVF and AVR. We were of course super concerned… Attending: Did you consider consulting another service? Resident: Yeah, of course. We got cardiology involved… Attending: Tell me more about why cardiology. Resident: (looks surprised at question):…well of course ‘cause her troponins came back positive and her EKG was totally messed up which made me worried that she was having a severe MI. I wanted cardiology to cath her. They thought this might be pericarditis but I was still concerned that there might be some underlying ischemia too. I was still concerned that the exertional chest pain and elevated troponins were related to ischemia. Attending: So what did you do? Resident: Inititally we got her started on aspirin, heparin and a statin and kept her NPO for a possible cath. I also put her on lasix since her BNP was high and she had some volume overload on her CXR. We started Lisinopril too. I didn’t give her a beta blocker since her heart rate was already low at 60. Cardiology said this wasn’t an ACS and that her symptoms were pericarditis so they told us to stop all of those medicines and start an NSAID. They didn’t think she needed a cath and told us to get an ECHO instead. They asked us to be careful with diuretics in case she had tamponade which they thought was less likely since she looked so stable. Her dizziness was really bad so I also gave her some meclizine Attending: What happened next? Resident: Her ECHO didn’t show an effusion so we were relieved by that. Her pain got a lot better with NSAIDs and her dizziness also went away with the meclizine. Attending: How did you monitor their progress? Author: SR CSR Script Date: Level: Case: 2 Resident: We rechecked her EKG and troponins and made sure her pain was getting better. Attending: How did you decide the patient was ready for discharge? Resident: Well her pain got a lot better and she was no longer dizzy so we figured she could go home. Attending: What did you decide was appropriate post-discharge follow-up? Resident: We got her an appointment with her PCP and she’s scheduled to see him in a couple of weeks. Cards also wanted to see her again so I set that up too. Attending: What steps did you take to assist in transitioning the patient to outpatient care? Resident: I sent her PCP a message through our EMR. Attending: Describe any patient or family factors that influenced your decision-making. Resident: Her family never came to visit us so we thought she was just fine so those factors never came into play. Attending: What did you learn from taking care of this patient? Resident: I think I kinda missed the boat on this patient by not thinking about pericarditis. So I read about that more. Attending: Knowing what you know now, what, if anything, could you do better to improve your own practice? Resident: I’m not sure. I think I just need to read more. Attending: Based on this patient's experience, what, if anything, can you do to improve the healthcare system for future patients? Resident: It really seemed like the system worked pretty well for her. Attending: Okay. Why don’t we stop there. Let’s debrief… Author: SR CSR Script Date: Level: Case: 2