Pathological role of Pin1 in the rheumatoid arthritis and neointima
advertisement
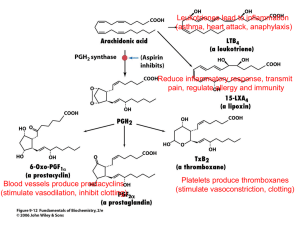
Pathological role of Pin1 in the rheumatoid arthritis and neointima formation Keon Wook Kang, Ph.D. (College of Pharmacy, Seoul National University) Rheumatoid arthritis (RA) is an autoimmune disease characterized by chronic inflammation in joints and subsequent destruction of cartilage and bone. Inflammatory mediators such as prostaglandins and pro-inflammatory cytokines contribute to RA progress. Pin1, a peptidyl prolyl isomerase, plays important pathophysiological roles in several diseases, including cancer and neurodegeneration. We found that both Pin1 and cyclooxygenase-2 (COX-2) were highly expressed in ankle tissues of Type II collagen-induced RA mice. HTB-94 cells overexpressing Pin1 and primary cultured human chondrocytes showed increased basal expression of pro-inflammatory proteins (COX-2, inducible nitric oxide synthase, tumor necrosis factor- and interleukin-1). Site-directed mutagenesis revealed that Pin1-mediated transcriptional activation of COX-2 was coordinately regulated by nuclear factor-B (NF-B), cyclic AMP response element binding protein (CREB), and CCAAT-enhancer binding protein (C/EBP). Gel shift, reporter gene, and Western blot analyses confirmed that NF-B, CREB and C/EBP were consistently activated in chondrocytes overexpressing Pin1. Treatment of RA mice with juglone, a chemical inhibitor of Pin1, significantly reduced RA progress and COX-2 expression in the ankle tissues. Moreover, juglone dose-dependently decreased the basal COX-2 expression in primary cultured chondrocytes from RA patients. These results demonstrate that Pin1 induction during RA progress stimulates pro-inflammatory protein expression by activating NF-B, CREB, and C/EBP. Abnormal proliferation of vascular smooth muscle cells (VSMCs) contributes to intima formation after stenting and balloon angioplasty. Because Pin1 overexpression is associated with transformation and the uncontrolled cell growth of tumors, we hypothesized that Pin1 also functions as a chronic stimulator of VSMCs proliferation. Pin1-positive smooth muscle cells were seen in the neointimal region of the femoral artery after guide wire injury. Exposure of VSMCS to platelet derived growth factor (PDGF) increased Pin1 expression in a concentration-dependent manner. Basal cell growth rate and cyclin D1 expression were enhanced in Pin1-overexpressing VSMCs (Pin1-VSMCs). Moreover, PDGF-induced production of reactive oxygen species (ROS) in Pin1-VSMCs was higher than in control VSMCs. In Pin1-VSMC, heme oxygenase-1 (HO-1) induction in response to nitric oxide donor was suppressed compared to control-VSMCs. Nuclear translocation of nuclear factor E2-related factor-2 (Nrf2) was also diminished in Pin1-VSMCs. Vice versa, activity of the inducible minimal antioxidant response element (ARE) was potentiated in Pin1-null mouse embryonic fibroblast (MEF), compared to Pin1-wild type MEF cells. Moreover, Nrf2 ubiquitination was stimulated by Pin1 overexpression. Intraperitoneal injection of juglone (a Pin1 inhibitor) for 3 weeks (1 mg/kg, two times a week), significantly suppressed neointimal formation induced by wire injury. Pin1 induction during neointimal formation may be associated with ROS-mediated VSMCs proliferation via down-regulation of Nrf2/AREdependent HO-1 expression. Considering the results of these two independent experiments, Pin1 may function as novel therapeutic targets for RA and chronic vascular diseases.