Immunopharmacology
advertisement

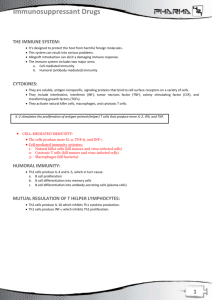
Immunopharmacology Drug Classes 1. Immunosuppressant a. Glucocorticoids i. Agents 1. Corticosteroids a. Prednisolone – oral b. Methylprednisolone – parenteral b. Interleukin Synthesis Inhibitors i. Agents 1. Calcineurin Inhibitors a. Cyclosporine b. Tacrolimus 2. mTOR (Mammalian Target of Rapamycin) Inhibitor a. Sirolimus/Rapamune c. Immunosuppressive Antiproliferative/Antimetabolite Agents i. Agents 1. Antimetabolites a. Purine Analogue i. Azathioprine/6-Mercaptopurine 2. Antiproliferative/Alkylating Agent a. Nitrogen Mustard i. Cyclophosphamide 3. Inosine Monophosphate (IMP) Dehydrogenase Inhibitor a. Mycophenolate Mofetil d. Immunosuppressive Antibodies i. Murine (Rat) Monoclonal Antibody 1. Muromonab-CD3/OKT3 ii. Antilymphocyte Globulin (ALG) iii. Antithymocyte Globulin Rabbit (ATG) iv. IL-2 Receptor Antibodies 1. Basiliximab 2. Daclizumab v. Miscellaneous Antibodies 1. Rh(D) Immune Gobuline a. Given to Rh (-) mother delivering Rh (+) child 2. Rh0 (D) Immune Globulin a. Given to suppress antibody production by Rh(-) mother after delivering Rh(+) baby b. Given within 72 hours after birth of Rh(+) baby i. Prevent hemolytic anemia in future pregnancy 3. Abciximab a. Binds to surface receptor of activated platelets b. Given after Coronary Angioplasty to prevent restenosis 4. Rituximab a. Attacks CD20 on i. Pre-B lymphocytes ii. Mature B lymphocytes 2. Immunostimulants a. Thymic Hormones i. Improve primary immune deficiency in children b. Synthetic Stimulant i. Levamisole 1. Stimulates a. Phagocytosis b. Production of T cells cytokines c. Adjuvant of Bacterial Origin i. Bacillus Calmette-Guerin (BCG) 1. Viable strain of Mycobacterium bovis 2. Enhances macrophages activity 3. Given in a. Cancer of the bladder b. Melanomas 3. Immunomodulators a. Immunostimulatory Cytokines i. Interleukins 1. IL-2 a. Enhance antitumor activity of i. Natural Killer Cell ii. Cytotoxic T cell ii. Colony Stimulating Factor 1. Granulocyte Colony Stimulating Factor (G-CSF) a. Given in neutropenia 2. Granulocyte Macrophage Colony Stimulating Factor (GM-CSF) a. Given to bone marrow transplant patients iii. Interferons 1. Interferon Alpha – produce by Leukocytes a. Antiviral b. Antiproliferative c. Given in i. Malignant melanoma ii. Renal cell carcinoma iii. Hairy cell leukemia iv. Kaposi’s sarcoma 2. Interferon Beta – produce by Fibroblast a. Antiviral b. Antiproliferative c. Given in i. Relapsing type Multiple Sclerosis 3. Interferon Gamma – produce by Lymphocytes a. Stimulates i. Natural Killer Cells ii. Macrophages b. Given in i. Chronic Granulomatous Disease b. Cytokine Inhibitors i. TNF Inhibitors 1. TNF Receptor Analogue a. Etanercept i. Use in Rheumatoid Arthritis 2. Chimeric Human anti-TNF Monoclonal Antibody a. Infliximab 3. Human IL-1 Receptor Antagonist a. Anakinra Agents 1. Prednisolone – oral 2. Methylprednisolone – parenteral Immunosuppressants Glucocorticoid Mechanism of Action 1. Inhibits Phospholipase A2 in which involve in the formation of Arachidonic Acid; precursor of a. Cyclooxygenase, in return will form i. Prostaglandin b. Lypooxygenase, in return will from i. Leukotriene 2. Inhibits Glucocorticoid Response Element (GRE) of DNA Consequences to that 1. Affects macrphages activity by a. ↓macrophage phagocytic activity b. Inhibit function in antigen recognition 2. Depress complement pathway 3. ↓proliferation of lymphocytes (T cells) 4. Inhibit cytotoxic activity of Cytotoxic T cells 5. ↑ in T suppressor a. Differentiation b. Maturation 6. Disrupts cooperation between B cell and T cell Adverse Effects Due to high dose usage of steroid 1. Supression of HypothalmicPituitary Adrenal Axis (HPA) function 2. Osteoporosis 3. Hypertension 4. Weight gain 5. Hyperglyceamia 6. Euphoric personality changes 7. Cataract Agents Cyclosporine 1. Can be given a. Alone b. Combination with i. Azathioprine ii. Prednisolone iii. Other anticancer drugs Drug Drug Interaction Cyclosporine alters the activity of CYP450 enzymes through o Inducing o Inhibiting Tacrolimus Structure similar to that of Macrolide o Erythromycin Used concomitantly with Prednisolone Interleukin Synthesis Inhibitors Calcineurin Inhibitors Pharmacokinetics Mechanism of Action Adverse Effects Absorption Variable degree of oral absorption Can be given orally Distribution Lypophilic cyclic peptide Readily distributed across body compartment Metabolism Extensively undergoes hepatic metabolism Excretion Billiary excretion 1. Calcineurin is a Phosphatase enzyme required to Dephosphorylate cytosolic Nuclear Factor of Activated T cells (NFATc) a. Dephosphorylation of NFATc will allow it to enter nucleus b. This will then a promote reaction that requires for cytokine synthesis 2. Cyclosporine will bind to a binding protein called Immunophilin a. Cyclosporine-Immunophilin complex will further bind to Calcineurin forming another complex of Cyclosporine-Calcineurin complex b. This complex is dysfunctional which therefore inhibits i. Transcription of IL-2 gene ii. Cytokine expression 1. IL-3 2. Interferon Gamma 1. 2. 3. 4. Nephrotoxicity Hepatotoxicity Hirsutism Neurotoxicity Absorption Readilly absorp orally Given o Orally o Parenterally Distribution Primarilly distributed in the Erythrocytes 99% bound to plasma protein o Albumin o α acid glycoprotein Extensively distributed to other tissues Passes breast milk Metabolism Undergoes CYP450 metabolism Excretion Billiary excretion – primary Renal – small fraction 1. Cyclosporine will bind to a binding protein called FK-Binding Protein (FKBP-12) a. Tacrolimus – FKBP-12 complex will further bind to Calcineurin forming another complex of Tacrolimus-Calcineurin complex b. This complex is dysfunctional which therefore inhibits i. Transcription of IL-2 gene ii. Cytokine expression 1. IL-3 2. Interferon Gamma 1. Nephrotoxicity 2. Nuerotoxicity a. Tremor b. Headache c. Motor disturbances d. Seizures 3. ↑risk of lymphomas 4. Hypersensitivity reaction 5. Hyperglyceamia 6. GI upsets 7. Hypertension Agents Sirolimus/Rapamune Structurally similar to that of Macrolide o Erythromycin Properties of Sirolimus 1. Selective blockade of cytokine signal transduction 2. Inhibitor of T cells a. Division b. Proliferation 3. Potent and effective immunosuppressor 4. Potent synergy with other immunosuppressor Interleukin Synthesis Inhibitors mTOR (Mammalian Target of Rapamycin) Inhibitor Pharmacokinetics Mechanism of Action Absorption Low absorption after oral admin Distribution Widely distributed across body compartments 92% bound to plasma protein o Albumin Long half life of 60 hours Metabolism Undergoes CYP450 metabolism Excretion Renal clearence 1. mTOR is a protein kinase 2. It plays an important role in IL-2 receptor responses 3. When IL-2 binds to its receptor on the T cells, mTOR will be activated a. mTOR will initiate a cascade effect including Cyclin Dependent Kinases which will then promote T cell i. Proliferation ii. Differentiation 4. Sirolimus will binds to Immunophilin and this Sirolimus-Immunophilin complex will inhibit the mTOR actvitiy resulting in a. IL-2 dependent cell cycle b. Harrasting the cell progression from G1-S phase Consequences to that ↓lymphocytes proliferation and differentiation Inhibits antibody production ↓mesenchymal cell proliferation o Vascular smooth muscle cells o Endothelial cells o Fibroblasts Adverse Effects 1. 2. 3. 4. Thrombocytopenia Hyperlipidaemia Rash ↑possibility to develop renal failure in combination with Cyclosporine Agents Mycophenolate Mofetil Immunosuppressive Antiproliferative/Antimetabolite Agents Inosine Monophosphate (IMP) Dehydrogenase Inhibitor Pharmacokinetics Mechanism of Action Derivative of Mycophenolic Acid Derived from a fungus o Penicillium stoloniferum Agents Muromonab-CD3 (OKT3) Produced through Hybridoma technology (hybridization technology) Directed against CD3 of T cells As it is originated from rat, body tends to produce antiMuromonab antibodies against it. Absorption Readily absorb after oral admin Distribution May displace drug from plasma proteins Metabolism Undergoes CYP450 metabolism Excretion Renal clearence 1. Inhibits the Inosine Monophosphate (IMP) Dehydrogenase enzyme 2. This enzyme involves in the de novo synthesis of Purine 3. Inhibition of this will lead to a. Suppressing proliferation of i. T cells ii. B cells b. Supressing macrophages activity Immunosuppressive Antibodies Murine (Rat) Monoclonal Antibody Pharmacokinetics Mechanism of Action Absorption 1. Muromonab will bind to Can not be absorped orally CD3 protein on the T cells Given only through IV 2. This will inhibit lymphocyte admin function as access to Metabolism antigen recogition site is Undergoes extensive blocked CYP450 metabolism 3. Subsequently depletes Excretion circulating T cells, thus Billiary excretion reducing T cells involvement in immune response Adverse Effects 1. Diarrhea 2. Leukopenia 3. Cytomegalovirus infection 4. ↑incidence of lymphoma and other malignancies Adverse Effects 1. Hypersensitivity reactions a. Chills b. Fever c. Thrombocytopenia d. Erythema 2. Anaphylactic shock 3. CNS effects a. Seizures b. Encephalopathy Due to its extensive side effects (considering its foreign in nature), it is seldom being used compared to Basiliximab and Daclizumab Immunosuppressive Antibodies Thymoglobulin Mechanism of Action Agents Antithymocyte Globulin Rabbit 1. Antibody binds to surface of the circulating T cells Antibodies derived from rabbit Due to its foreigness, body produces anti-ATG antibodies to fight against it. Agents Basiliximab (Simulect®) Chimeric murine monoclonal antibodies Given only through IV Serum half life of about 7 days Daclizumab (Zenapax®) Humanized monoclonal antibodies Fromed by spilicing the murine complimentary portions of light and heavy chain o Fused it with Human Fab framework o Then associates with Human IgG Fc segment 2. This will then leads to a. Complement mediated destruction b. Antibody depedent cytotoxicity c. Apoptosis d. Opsonisation 3. Antibody bounded T cells will be destroyed in the a. Liver b. Spleen IL-2 Receptor Antibodies Mechanism of Action 1. Binds to IL-2 receptor alpha subunit on activated T cell 2. This will then block further activation of other T cells leading to inhibition of clonal expansion of T cells Advantages of Chimeric Vs Humanized 1. ↓immunogenecity (foreigness) without sacrificing affinity 2. Allow complement fixation to occur by using Human Fc region instead of murine 3. Humanization of Fab region my reduce affinity as it wont attack self antigen a. Baciliximab has ↑affinity to IL-2 receptor compared to Daclizumab Adverse Effects 1. 2. 3. 4. Chills Fever Leukopenia Thrombocytopenia Adverse Effects 1. GIT upsets 2. No antibodies production against Basiliximab 3. Very well tolerated