Katkish Lauren Abstract 2015
advertisement
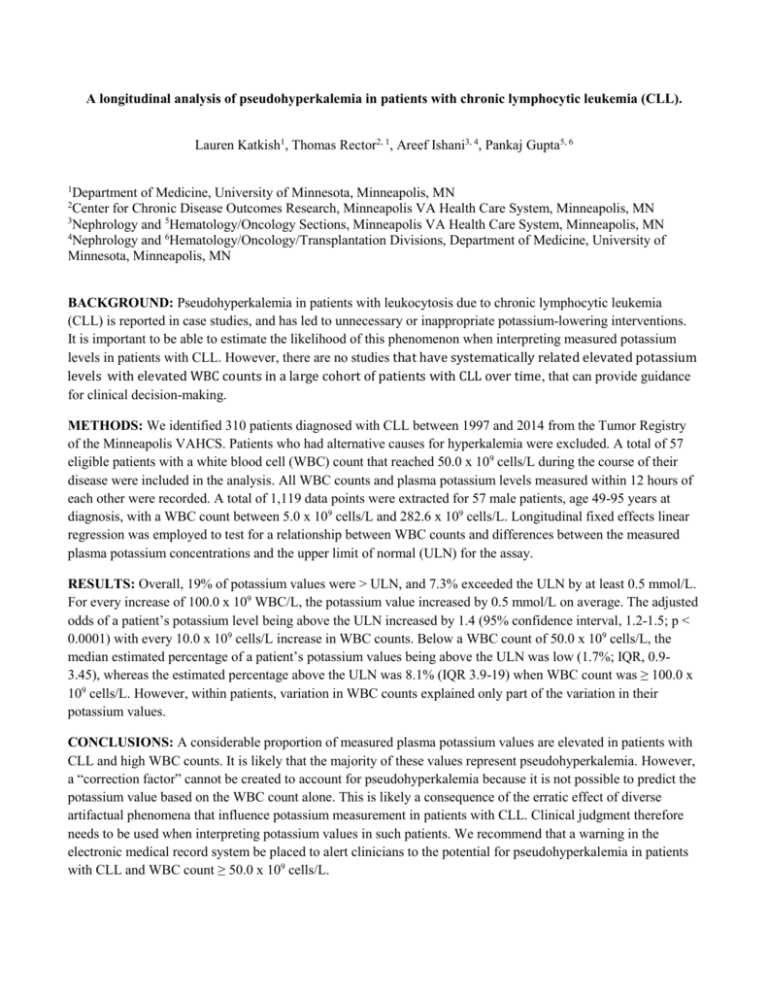
A longitudinal analysis of pseudohyperkalemia in patients with chronic lymphocytic leukemia (CLL). Lauren Katkish1, Thomas Rector2, 1, Areef Ishani3, 4, Pankaj Gupta5, 6 1 Department of Medicine, University of Minnesota, Minneapolis, MN Center for Chronic Disease Outcomes Research, Minneapolis VA Health Care System, Minneapolis, MN 3 Nephrology and 5Hematology/Oncology Sections, Minneapolis VA Health Care System, Minneapolis, MN 4 Nephrology and 6Hematology/Oncology/Transplantation Divisions, Department of Medicine, University of Minnesota, Minneapolis, MN 2 BACKGROUND: Pseudohyperkalemia in patients with leukocytosis due to chronic lymphocytic leukemia (CLL) is reported in case studies, and has led to unnecessary or inappropriate potassium-lowering interventions. It is important to be able to estimate the likelihood of this phenomenon when interpreting measured potassium levels in patients with CLL. However, there are no studies that have systematically related elevated potassium levels with elevated WBC counts in a large cohort of patients with CLL over time, that can provide guidance for clinical decision-making. METHODS: We identified 310 patients diagnosed with CLL between 1997 and 2014 from the Tumor Registry of the Minneapolis VAHCS. Patients who had alternative causes for hyperkalemia were excluded. A total of 57 eligible patients with a white blood cell (WBC) count that reached 50.0 x 109 cells/L during the course of their disease were included in the analysis. All WBC counts and plasma potassium levels measured within 12 hours of each other were recorded. A total of 1,119 data points were extracted for 57 male patients, age 49-95 years at diagnosis, with a WBC count between 5.0 x 109 cells/L and 282.6 x 109 cells/L. Longitudinal fixed effects linear regression was employed to test for a relationship between WBC counts and differences between the measured plasma potassium concentrations and the upper limit of normal (ULN) for the assay. RESULTS: Overall, 19% of potassium values were > ULN, and 7.3% exceeded the ULN by at least 0.5 mmol/L. For every increase of 100.0 x 109 WBC/L, the potassium value increased by 0.5 mmol/L on average. The adjusted odds of a patient’s potassium level being above the ULN increased by 1.4 (95% confidence interval, 1.2-1.5; p < 0.0001) with every 10.0 x 109 cells/L increase in WBC counts. Below a WBC count of 50.0 x 109 cells/L, the median estimated percentage of a patient’s potassium values being above the ULN was low (1.7%; IQR, 0.93.45), whereas the estimated percentage above the ULN was 8.1% (IQR 3.9-19) when WBC count was ≥ 100.0 x 109 cells/L. However, within patients, variation in WBC counts explained only part of the variation in their potassium values. CONCLUSIONS: A considerable proportion of measured plasma potassium values are elevated in patients with CLL and high WBC counts. It is likely that the majority of these values represent pseudohyperkalemia. However, a “correction factor” cannot be created to account for pseudohyperkalemia because it is not possible to predict the potassium value based on the WBC count alone. This is likely a consequence of the erratic effect of diverse artifactual phenomena that influence potassium measurement in patients with CLL. Clinical judgment therefore needs to be used when interpreting potassium values in such patients. We recommend that a warning in the electronic medical record system be placed to alert clinicians to the potential for pseudohyperkalemia in patients with CLL and WBC count ≥ 50.0 x 109 cells/L.