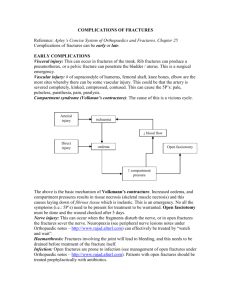
File - Nanik Hatsakorzian`s E
advertisement

Nanik Hatsakorzian Pharm.D/MPH candidate 2014 Touro University- College of Pharmacy- CA Osteoporosis quick reference Calcium intake - Women ≥ 51 yo = 1200 mg per day - Men 50-70 yo = 1000 mg per day - Men ≥71 yo =1200 mg per day - Excess calcium supplement intake >1200 mg have limited potential for benfit and may increase the risk of developing kidney stones, cardiovascular disease and stroke. In addition, there is no evidence that calcium intake in excess of these amounts confers additional bone strength. - Average daily dietary calcium intake in adults age 50 and older is 600-700 mg per day. Increasing dietary calcium is the first-line approach, but calcium supplements should be used wen an adequate dietary intake cannot be achieved. - In general 8oz of milk or 6oz of yogurt will have ~300 mg of calcium. 1 oz of cheese have ~200 mg of calcium and anything that is calcium fortified will be within the range of 80-1000 mg per serving Vitamin D intake - Men and women 50+ = 800-1000 IU per day - Vitamin D2 is derived from plant sources, and supplementations with vitamin D2 or D3 can be used. - Vitamin D fortified milk will have ~400 IU per quart. - Serum 25(OH)D levels should be maintained at ~30 ng/ml - In 2010 FDA increased the safe upper limit for Vit D intake for general adult population to 4000 IU per day. Who is indicated for BMD testing? - Regardless of clinical risk factors, women > 65 and men >70 - Younger menopausal women, in menopausal transition, and men age 50-69 with clinical risk factors - Adults who have fractures after age of 50 - Adults with a condition (e.g., rheumatoid arthritis) or taking a medication (prednisone >5 mg of daily dose or equivalent for ≥ 3 months) that is associated with low bone mass or bone loss. When should vertebral imaging be performed? - All women ≥70 yo and men ≥ 80 yo - All women 65-69 and all men 75-79 if BMD T-score is -1.5 or below - In postmenopausal women 50 to 64 and men 50-69 with specific risk factors: o Low trauma fracture o Historical height loss of 1.5 inches or more (4cm) o Prospective height loss of 0.8 inches or more (2cm) o Recent or ongoing long-term glucocorticoid treatment FDA approved drugs for osteoporosis Bisphosphonates: - Alendronate (Fosamax, Fosamax +D, Binosto) o Prevention dose is 5 mg daily or 35 mg weekly o Treatment dose is 10 mg daily (2800 IU vit D3) or 70 mg weekly (5600 IU vit D3) - - - o Reduces incidences of spine and hip fractures ~50% over 3 years in patients with and without hx of vertebral fracture o Use is not recommended in patient’s with CrCl <35 Ibandronate (Boniva) o Treatment for postmenopausal osteoporosis is 150 mg monthly tablet or 3 mg IV injection Q3 months. Serum creatinine should be check prior to each injection. o Reduces risk of vertebral fractures by ~50% in 3 years, but not non-vertebral fractures. Risedronate (Actonel, Atelvia) o 35mg weekly tablet contain 6 tablets of 500 mg of calcium carbonate o Reduces risk of vertebral fractures by ~ 41-49% over 3 years, and non-vertebral fractures by ~36% Zolendronic acid (Reclast) o 5mg IV over 15 minutes every year for treatment and every two years for prevention. o Reduces risk of vertebral fractures by 70%, hip fractures by 41%, and non-vertebral fractures by ~25% over 3 years o Pre-treatment with acetaminophen might be necessary to prevent acute phase reaction (arthralgia, headache, myalgia, fever) Bisphosphonate consultation points: - Take on empty stomach first thing in the morning with 8 oz of plain water o Delayed release Atelvia should be taken immediately after breakfast with 4oz of plain water - Wait at least 30 minutes before eating (60 minutes for ibandronate) while remaining upright (sitting or standing) for at least an hour. - All bisphosphonates effect renal function and contraindicated with creatinine clearance below 35 ml/min or evidence of acute renal impairment. - Main side effects of bisphosphonates include: Hypocalcemia (hypocalcemia should be corrected prior to initiation of bisphosphonate agent), osteonecrosis of the jaw ONJ (risk factors include invasive dental procedures, dental implants, ill fitting dentures, and bad oral hygiene. Stopping bisphosphonates prior to dental procedures to reduce the risks of ONJ has been inconclusive due to long duration of action). Other side effects include: GERD, abdominal pain, erosive esophagitis, N/D, and flatulence. Calcitonin - Miacalcin, Fortical o Salmon calcitonin approved for treatment of osteoporosis in women with at least 5 years of postmenopausal. 200 IU single daily intranasal spray o Reduces vertebral fractures ~ 30% in patients with prior vertebral fracture, but doesn’t reduce occurrence of non-vertebral fractures o Calcitonin is also FDA approved for hypercalcemia, and symptomatic Paget’s disease treatments (treatment duration is 3 months not to exceed 6 months in certain situations due to increase risk of cancer) o No dosage adjustment is necessary for renal or hepatic impairments o It is also known to help reduce bone pain as well. o MoA: Peptide sequence similar to human calcitonin; functionally antagonizes the effects of parathyroid hormone. Directly inhibits osteoclastic bone resorption; promotes the renal excretion of calcium, phosphate, sodium, magnesium, and potassium by decreasing tubular reabsorption; increases the jejunal secretion of water, sodium, potassium, and chloride o On March 2013, FDA announced that risks of inhalable osteoporosis drug outweigh its benefits when used to treat brittle bones due to slightly higher rate of cancer. “The potential for a cancer risk with calcitonin salmon therapy cannot be ignored. The majority of all calcitonin salmon trials showed an increased risk estimate.” FDA panel was nearly unanimous that any future calcitonin drugs should be required to show real effectiveness in preventing bone fractures. Estrogen Therapy/Hormone Therapy (ET/HT) - Estrogen (climara, estrace, Estraderm, estratab, ortho-Est, Premarin, Vivelle) - Hormone therapy (Prempro, Femhrt, Activella, Premphase) o FDA approved for osteoporosis prevention, relief of vasomotor symptoms and vulvovaginal atrophy associated with menopause. o Women with intact uterus (hysterectomy) not performed should have formulations with progestin to protect the uterine lining. o Reduces vertebral fractures ~34% and other osteoporotic fractures by ~23% over 5 years of use. o Bone loss can be rapid upon stopping, consider initiating alternative agents to maintain BMD o Studies show increased risk of MI, stroke, invasive breast cancer, pulmonary emboli and deep vein thrombosis during five years of Prempro treatment, but no increase in the abovementioned if treatment started within 10 years of menopause. o Studies also show no increase in breast cancer incidence over 7.1 years of treatment with estrogen only. o Lowest effective dose and shortest duration should be considered when using ET/HT to treat menopausal symptoms o ET/HT is not considered first line if it is used solely for osteoporosis prevention Estrogen agonist/antagonist - Raloxifene (Evista) o FDA approved for both prevention and treatment of osteoporosis in menopausal women as well as reduction in risk of invasive breast cancer in postmenopausal women with osteoporosis. o Reduces vertebral fractures ~ 30% in patients with prior vertebral fracture and 55% in patients with no hx of vertebral fractures, but reduction of non-vertebral fractures has not been demonstrated. Evista does not reduce risk of coronary heart disease. o It can increase hot flashes, and risks of DVT o Pregnancy category X Parathyroid Hormone - PTH (1-34), Teriparatide (Forteo) o FDA approved for treatment of osteoporosis in postmenopausal women and men at high risk of fractures or on glucocorticoid therapy. As well as in men with primary or hypogonadal osteoporosis with high risk of fractures. o Anabolic agent, 20 mcg daily SQ injections. Forteo can be used for maximum of two years o Bone loss can be rapid upon stopping, consider initiating alternative agents to maintain BMD o Contraindicated in patients with: Increased risk of osteosarcoma Paget’s disease Prior radiation therapy of skeleton, bone metastases, hypercalcemia History of skeletal malignancies Receptor Activator of Nuclear Factor Kappa-B Ligand (RANKL) inhibitor - Denosumab (Prolia) o FDA approved for postmenopausal women with high risk of fracture and bone loss due to breast cancer, in addition to men with high risks of fractures and bone loss due to prostate cancer treatment o Administered by healthcare professionals only, 60 mg SQ Q6 months o Reduces vertebral fractures ~ 68%, hip fractures by ~40%, and 20% in non-vertebral fractures over 3 years. o Bone loss can be rapid upon stopping, consider initiating alternative agents to maintain BMD o Major side effect is hypocalcemia. Hypocalcemia should be corrected prior to Prolia administration o DDI with cytarabine Reference: National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. 2013. http://www.nof.org/files/nof/public/content/resource/913/files/580.pdf