State Hospital Association Project Coordinators* Operational Manual
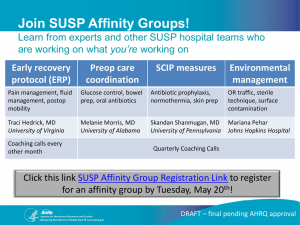
advertisement

CUSP for Safe Surgery (SUSP) Operations Manual for Coordinating Entities Armstrong Institute for Patient Safety and Quality Table of Contents A Message from SUSP National Project Team .............................................................................................. 3 A Few Thoughts Before We Get Started ....................................................................................................... 4 SUSP Project Overview ................................................................................................................................. 4 SUSP is Different from other Surgical Quality Initiatives .......................................................................... 5 Your Responsibilities as a Coordinating Entity.............................................................................................. 5 Recruit Hospital Teams ............................................................................................................................. 6 Tip: What to Do if Hospitals Do Not Want to Participate ..................................................................... 6 Coach Hospital Teams with NPT Support ................................................................................................. 7 Get Familiar with the SUSP Approach ................................................................................................... 7 Facilitate SUSP Coaching Calls with SUSP “State Coach” and “State Coordinator” .............................. 7 Send Weekly Updates and Project Call Slides to Hospital Teams ......................................................... 7 Enable SSI and Safety Culture Data Reporting .......................................................................................... 8 SSI Data ................................................................................................................................................. 8 Safety Culture Data ............................................................................................................................... 9 Share Your Experiences with Other CEs and the NPT ............................................................................... 9 Concluding Thoughts .................................................................................................................................. 10 Coordinating Entity Checklist ...................................................................................................................... 11 Page 2 A Message from SUSP National Project Team Dear colleagues, It is an honor to work with you on SUSP, a national effort to reduce preventable harm in surgical patients. This effort is informed by the tremendous learning we did together in the national On the CUSP: Stop BSI program; a program that reduced central line-associated blood stream infections (CLABSI) state by state, in over 1100 hospitals. It is one of the few national success stories for reducing a preventable harm. And we will use a similar approach in SUSP: It will be led by clinicians, informed by science, and guided by valid measures. It will work by leveraging the wisdom and passion of front-line clinicians for reducing harm. It will be driven by the intrinsic motivation of clinicians rather than external motivation by regulators or economic incentives. Yet it will not be easy. It is difficult to implement improvement programs in operating rooms. Surgical teams have exceedingly complex social and political structures – enmeshed in a rich and noble history, full of traditions and hierarchy, comprised of many sub teams. The science for how to prevent harm in surgical patients is less mature than it is for preventing CLABSI. The measures are noisy. Yet the need could not be greater. Quick fixes have not been effective; preventable harm in surgical patients continues seemingly unabated. Real improvement must be driven by peer norms, involve culture change and use of evidence-based practices. It will require us to learn together. The SUSP collaborative unites these components. We hope you join us on this important journey. Best regards, Peter J. Pronovost, MD, PhD Director, Armstrong Institute for Patient Safety and Quality Senior Vice President, Patient Safety and Quality Johns Hopkins Medicine Page 3 A Few Thoughts Before We Get Started The SUSP National Project Team (NPT) strives to make this project impactful for you and your hospital teams in a time when you are more overextended than ever before. We know, for example, that you don’t have time to read a lengthy manual, so we’ve tried to keep this one concise. We’ve organized this manual to introduce you to SUSP concepts and clarify your roles and responsibilities. We’ll also refer to tools and resources you can find on the SUSP website. You can use a checklist at the very end of the document to keep your work on track. We strongly encourage you to become familiar with (and ‘bookmark’) the SUSP website! This manual is a work in progress. If you have questions or ideas about how to improve it, please contact the SUSP helpdesk at SUSP@jhmi.edu. We value your experience, perspective and input. Let the journey begin. SUSP Project Overview Our shared SUSP project goals are to: 1. Achieve significant reductions in surgical site infection (SSI) and other surgical complication rates; 2. Improve safety culture, teamwork and communication by implementing the Comprehensive Unitbased Safety Program (CUSP) in the perioperative area. The Agency for Healthcare Research & Quality (AHRQ) has funded SUSP through August 2015. Participation is open to any hospital in any state, as well as hospitals in the District of Columbia and Puerto Rico. Hospitals may participate through their state hospital association, state patient safety agency, Hospital Engagement Network (HEN) or other convening group. We will work with individual hospitals that are not part of a larger “coordinating entity” to explore how to facilitate their involvement. What’s a Coordinating Entity? SUSP and your Hospital Engagement Network The Center for Medicare and Medicaid Innovation (CMMI) HENs coordinate a range of collaborative improvement activities with hospitals, including efforts to reduce SSI. Both CMMI and AHRQ agree that CMMI-funded HENs can use the AHRQ-funded SUSP project to fulfill their responsibility to reduce preventable harm from SSI. Therefore state hospital associations or HENs may function as SUSP Coordinating Entities (CEs). The Johns Hopkins Armstrong Institute for Patient Safety and Quality (AI) is the primary lead for this project. The AI team includes experts from the national CLABSI project and similar large-scale initiatives, including Drs. Peter Pronovost and Sean Berenholtz, and Johns Hopkins surgeon Dr. Elizabeth Wick. AI has partnered with the following organizations and experts to guide this important work: American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP), Page 4 The World Health Organization Patient Safety Programme Dr. Charles Bosk, Professor of Sociology and Medical Ethics from the University of Pennsylvania SUSP is Different from other Surgical Quality Initiatives By enabling SUSP efforts in your state or HEN, you lead the national effort to reduce surgical complications. However, SUSP is not a checklist or a prescription for success. Only hospital teams understand local obstacles and opportunities for improvement. SUSP provides a structure for hospital teams to identify and address local defects in care, implement evidence-based practice, and collaborate with other hospital teams and surgical quality experts. Success requires creative energy, persistence, leadership and teamwork. Take a look at the resources below to learn more about SUSP methods. SUSP Content Length Identifies project goals and methods Clarifies participation requirements and timeline The first project call for hospital teams identifies the goals and conceptual model of the SUSP project. Describes SUSP project “asks” that will help ensure hospital team success. 15 pages Describes the five steps of CUSP that hospital teams will implement to improve their perioperative safety culture. 14 pages Describes a three-pronged approach hospital teams can use to close the gap between evidence-based guidelines and bedside practice. 7 pages Identifies learning goals, materials, and deliverables for each month of the project. It refers to forms and tools that you can find on the project website. 51 min SUSP Recruitment Call Recording 1 hour 49 min SUSP Kickoff Call Recording CUSP for Safe Surgery Manual Surgical Complication Prevention Toolkit Manual SUSP Project Management Guide: Onboarding Phase Overview Your Responsibilities as a Coordinating Entity As a CE, you have four key responsibilities: Key Coordinating Entity Responsibilities 1. Recruit hospital teams. 2. Coach hospital teams with NPT support. 3. Enable safety culture and SSI data reporting. Page 5 4. Share your experiences with other CEs and the NPT. We’ll describe these responsibilities in more detail, below. Recruit Hospital Teams The NPT designed SUSP as a large-scale collaborative to facilitate learning and accelerate improvement. We ask that you set a goal to recruit at least ten hospitals in your state or Hospital Engagement Network (HEN). All hospitals in every state, the District of Columbia, and Puerto Rico are encouraged to join the effort. There are no fees to participate. Hospitals actively participate in SUSP for a minimum of 24 months, but may choose to extend their participation through the life of the collaboration. Hospital teams joining in cohort 5 will participate until the contract ends in August 2015, for a total of 18 months. Tip: What to Do if Hospitals Do Not Want to Participate You may encounter recruitment challenges. The following are some typical reasons for resisting participation, and examples of responses you can provide. Reason # 1: “We are already using a bundle to reduce SSI and our SCIP measures are nearly perfect.” Your Response: Your hospital has done great work with SCIP, but what are your SSI rates? Patient outcomes are even more important than process measures. Even if your SCIP compliance is high, there are likely ways your hospital can improve care. Reason #2: “We are an academic medical center and our patients are too sick.” Your Response: SUSP is not a one-size-fits-all project. Your hospital will create an improvement team to work on the problems that your own frontline staff identify. Similar approaches have reduced harm in hospitals across the country, including academic centers with high acuity. Reason #3: “This project is not a priority for us.” Your Response: Hospital-acquired infection prevention is a national priority. Surgical complications kill about 150,000 people per year in the United States. HHS has created a national strategy to reduce SSI and CMS requires hospitals to publically report infection rates from colorectal surgery. If your hospital’s rates are high, you may benefit from participation. If they are low, this is an opportunity to share what you know with a national audience. Page 6 The NPT will send you recruitment materials, including a SUSP Recruitment Call invitation, to circulate to hospitals. We will work with you to ensure that we’ve received all necessary documents from your participating hospitals prior to the SUSP Kickoff Call that marks the start of each cohort. Coach Hospital Teams with NPT Support Hospital leaders and frontline staff can improve patient safety and eliminate preventable harm through technical and adaptive work. Technical work focuses on procedural aspects of care that can be explicitly defined, such as surgical skin preparation procedures. Adaptive work focuses on the attitudes, beliefs and behaviors of the people who deliver care. Adaptive work is nebulous and difficult. Hospital teams may be tempted to focus on technical work, and leave adaptive problems unaddressed. Yet many change efforts fail because adaptive work is neglected. For example, an evidence-based procedural checklist (technical work) will only impact outcomes if staff understand, value, and prioritize use of the checklist (adaptive work). Get Familiar with the SUSP Approach As a CE, you are well positioned to support hospital teams and reinforce key project concepts, like the importance of embedding adaptive work through the Comprehensive Unit-based Safety Program (CUSP) in the technical work of surgical care. In addition to the resources on page 5, take a look at this article, authored by members of the NPT, to learn how a surgical team at the Johns Hopkins Hospital applied CUSP to reduce SSI rates that were high despite near perfect compliance with Surgical Care Improvement Project (SCIP) measures. Once you’re familiar with the SUSP approach, you can become the first point of contact for hospital teams with questions or concerns about the project. Facilitate SUSP Coaching Calls with SUSP “State Coach” and “State Coordinator” We believe that hospital teams will learn as much (if not more) from each other than they will from us. One of your most important responsibilities as a CE is to convene your participating SUSP hospitals for monthly coaching calls. Coaching calls provide SUSP hospitals an opportunity to ask questions, share challenges and triumphs, and review their aggregated SSI data reports. You may already host coaching calls for hospitals participating in other improvement initiatives. We defer to you regarding best use of your resources, i.e. whether it makes sense to consolidate existing coaching calls or hold separate calls for SUSP. When you’ve selected a date and time for regular coaching calls, contact us at SUSP@jhmi.edu and we’ll connect you with a “state coach” and “state coordinator” from the NPT. Your coach and coordinator are your main point of contact to the NPT. They will help you facilitate calls, reinforce key concepts or action items, and support hospital teams’ progress. Send Weekly Updates and Project Call Slides to Hospital Teams We know you’re very busy, and you don’t have time to weed through an endless stream of emails. The NPT consolidates most SUSP-related communications into a “weekly update” – a simple table of Page 7 notifications, updates and reminders we circulate via email each Friday afternoon. Please forward these updates to your hospital teams to keep them in the loop. In addition to weekly updates, we’ll send you project call slides the week prior to each call. We ask that you forward these along as well. Enable SSI and Safety Culture Data Reporting Prefer webinars to manuals? Listen to an archived webinar about how you and your hospital teams will use the SUSP website to put SSI and safety culture data in the hands of frontline staff (where it can really make a difference)! SSI Data Often, frontline staff and senior leadership are unaware of hospital performance at the unit level. SSI data transfer gives you and your hospital teams access to timely data reports with comparators and trend lines so you all know whether SUSP interventions are really working. Hospital teams can elect to have existing SSI data transferred into the SUSP website from either the National Healthcare Safety Network (NHSN) or ACS NSQIP databases, or both. Hospital teams also have the option to manually enter SSI data into the project database. SSI data transfer is a multistep process, and your role will vary depending upon the data source (NHSN or NSQIP) hospital teams choose to use for the project. Important Note: Regardless of data source, we must receive hospital teams’ enrollment documents, including the SUSP Team Registration Form and Data Use Agreement (DUA). We will need your help to nudge teams to provide us with these documents. Without them, hospital teams cannot create realtime SSI data reports that provide them with crucial performance feedback. Please refer to the table below for a list of SSI data transfer steps. Notably, for hospitals using NHSN data, you will be responsible for exporting SSI data files from NHSN and uploading them into the SUSP website each month. We have developed training resources to familiarize you with this process, and, as always, are here to support your efforts. Who’s Responsible? Hospital Team Hospital using NHSN data 1. Return SUSP Team Registration Form and DUA to NPT (susp@jhmi.edu) and Coordinating Entity Hospital using NSQIP data 1. Return SUSP Team Registration Form and DUA to NPT (susp@jhmi.edu) and Coordinating Entity a. NSQIP sends Addendum DUA to hospital team b. Hospital team returns Addendum DUA to NSQIP NPT 2. Sign DUA and return fully executed DUA to Coordinating Entity 2. Sign DUA and return fully executed DUA to Coordinating Entity 3. Register hospital team in the SUSP SSI data registry 3. Register hospital team in the SUSP SSI data registry Page 8 Who’s Responsible? Hospital using NHSN data 4. Contact CE to walk through steps 5 – 7 Coordinating Entity Hospital using NSQIP data 4. Transfer NSQIP SSI data into the SUSP SSI data registry 5. Create SUSP hospital group in NHSN, if necessary, and ask SUSP hospitals to confer rights 6. Export hospitals’ SSI data from NHSN 7. Upload NHSN SSI data into the SUSP SSI data registry Manual NHSN Unadjusted SSI Exporting and Uploading Data Manual Safety Culture Data Teams that collect data about their local safety culture and use a debriefing process to discuss results together have demonstrated greater reductions in infection rates than teams that don’t. As a CE, while you are not directly responsible for safety culture data collection at the hospital team level, we ask that you monitor your hospital teams’ progress through the safety culture data collection and debriefing process. Hospital teams can use the SUSP website to administer AHRQ’s Hospital Survey on Patient Safety (HSOPS) to their frontline staff or upload previously collected HSOPS data during a 45-day “survey open period.” Once the survey period ends, the hospital team’s survey coordinator can use the SUSP website to download a comprehensive, intuitive report of safety culture in his or her work area. Hospital teams can use these reports during safety culture debriefings. Hospital teams that use a safety culture survey other than HSOPS can participate in SUSP. Though they may not upload safety culture data in the SUSP website, we ask that they complete the safety culture debriefing process with their frontline staff. You can use the SUSP website to track whether hospital teams have administered HSOPS or uploaded previously collected data. We’ll walk you through this process during the second project call, “How to Use the SUSP Website: A Training Call for SUSP Facilitators.” We ask that you monitor hospital teams’ progress on a weekly basis during the survey open period, and give them a nudge if they need to submit their safety culture data. Share Your Experiences with Other CEs and the NPT We believe that SUSP project success depends upon your engagement, and our ability to support your efforts as you support hospital teams. We want to stay connected with you and connect you to each other. The NPT hosts monthly CE calls that enable us to collectively discuss our challenges and successes, and learn from one another. We invite you to share stories, ask questions, and provide any Page 9 feedback you may have about the project. We’ll send you a calendar invitation for these calls occurring on the third Friday every month at 3pm EST. Concluding Thoughts We are honored to work with you to achieve and demonstrate success at improving safety culture and reducing surgical complications. This project is a team effort, and we will partner with you every step of the way as you support and enable your hospital teams. We anticipate long-term success to be greatly dependent on strong hospital association engagement and energized hospital leadership and unit teams. We are confident that with your help this project will yield powerful stories, meaningful data, and safer care for surgical patients. Page 10 Coordinating Entity Checklist (for Cohort 5) SUSP Phase Recruitment March-April 2014 Onboarding May-October 2014 Check when done Action By March 21, 2014: Sign and return Coordinating Entity Participating Agreement to the SUSP helpdesk SUSP@jhmi.edu Forward recruitment material (e-mail from the Armstrong Institute) to your hospitals. Remind hospitals to attend SUSP recruitment calls on March 3 or March 5. If hospitals are interested in participating, remind SUSP project leads weekly to submit enrollment forms to the SUSP helpdesk (SUSP@jhmi.edu). By April 7, 2014: Send calendar invites for the cohort 5 kickoff webinar to all participating hospitals. By April 21, 2014: Forward SUSP kickoff packet to participating hospitals. Send calendar invites for Onboarding Phase project calls to all participating hospitals. Refer to onboarding phase project management guide in kickoff packet material. Beginning in April, participate in the monthly CE coaching calls Beginning May 2, 2014: Forward SUSP weekly update to all participating hospitals. Forward project call slides to all participating hospitals at least one day before scheduled project call By May 12, 2014: Schedule and send calendar invites for monthly coaching calls with all participating hospitals. May 12, 2014: Cohort 5 HSOPS surveys opens. By May 9, 2014: Send all participating hospitals HSOPS manuals located on our SUSP website Remind teams to collect new HSOPS surveys, or upload previously collected HSOPS results. Monitor team’s HSOPS progress on a weekly basis. Join the project call on May 12 or May 16 to learn how to navigate your hospital’s HSOPS networks. By September 30, 2014: Have all participating NHSN hospitals join and confer rights to your NHSN group. Refer to manual on website. https://armstrongresearch.hopkinsmedicine.org/susp/resources.aspx By October 31, 2014: Export and upload all participating NHSN hospitals’ SSI data into the SUSP online data portal. Refer to manual on website. The NPT will send out a CE checklist for the Implementation and Sustainability phases in the fall of 2014. Page 11