CUSP for Safe Surgery: The Surgical Unit
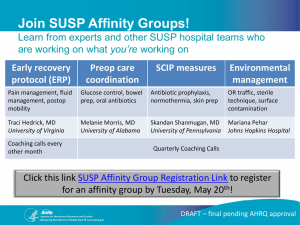
advertisement

CUSP for Safe Surgery: The Surgical Unit-Based Safety Program March 3 & 5, 2014 Sean Berenholtz, MD, MHS, FCCM Some quick administrative announcements • You need to dial into the conference line to hear audio – Dial in Number: 1-800-311-9401 – Passcode: 83762 • A copy of these slides can be found on our SUSP recruitment website • A recording of this webinar will be available on the recruitment website by March 6, 2014. 2 Learning Objectives • Identify SUSP program – Project goals and interventions – Participation requirements and timeline • Describe steps to enroll in SUSP Why is Your SUSP Work Important? • 1 in 25 people will undergo surgery • 7 million (25%) in-patient surgeries followed by complication • 1 million (0.5 – 5%) deaths following surgery • 50% of all hospital adverse events are linked to surgery AND are avoidable http://www.who.int/patientsafety/chall enge/safe.surgery/en/ 4 How is SUSP different than SCIP (Surgical Care Improvement Project Your Team Addresses Local Needs • No single SSI prevention bundle – Frontline staff identifies local defects – Fix defects with executive support • Measure local safety culture using Hospital Survey of Patient Safety (HSOPS) Questions? Email the SUSP help desk! SUSP@jhmi.edu 6 SUSP Project Overview SUSP Project Overview • AHRQ funding project – Individual hospitals participate for 18 months years • Leveraging leaders in field – Armstrong Institute, ACS NSQIP, AHRQ, University of Pennsylvania, WHO • All hospitals in any state, as well as hospitals in the District of Columbia and Puerto Rico are encouraged to participate. 8 Who can join SUSP? • Participation in the program is available to any hospital in any state, as well as hospitals in the District of Columbia and Puerto Rico. • Hospitals may participate through their state hospital association, state patient safety agency, hospital engagement network (HEN) or other convening group. Questions? Email the SUSP help desk! SUSP@jhmi.edu 9 SUSP Enrollment by Coordinating Entity Armstrong Institute for Patient Safety & Quality Arkansas Hospital Association Colorado Hospital Association Connecticut Hospital Association Florida Hospital Association Georgia Hospital Association (HEN) Premier Healthcare Alliance (HEN) Hawaii Safer Care SUSP Collaborative Iowa Healthcare Collaborative (HEN) Maryland Hospital Association Michigan Health & Hospital Association (HEN) Nevada Health Insight (HEN) Tennessee Hospital Association (HEN) 10 Massachusetts Hospital Association SUSP Enrollment by Coordinating Entity and Cohort Coordinating Entity Number of Hospitals Enrolled Arkansas Hospital Association 11 Armstrong Institute 31 Colorado Hospital Association 8 Connecticut Hospital Association 5 Florida Hospital to Association 11 • Click edit Master text styles Georgia Hospital Association 14 – Second Hawaii Safer Care SUSPlevel Collaborative 14 HealthInsight•Nevada 4 Third level Iowa Healthcare Collaborative 13 – Fourth level Maryland Hospital Association 18 » Fifth level Massachusetts Hospital Association 8 Michigan Health & Hospital Association 46 Premier Healthcare Alliance 8 Tennessee Hospital Association 10 Total Enrollment Cohort 1 10 Cohort 2 102 Cohort 3 47 Cohort 4 42 Total 201 11 Our Shared Project Goals • To achieve significant reductions in surgical site infection and surgical complication rates • To achieve significant improvements in safety culture Questions? Email the SUSP help desk! SUSP@jhmi.edu 12 How Are We Achieving Our Goals? Translating Evidence Into Practice (TRiP) 1. Summarize the evidence Reducing Surgical Site Infections Comprehensive Unit based Safety Program (CUSP) • Emerging Evidence 1. Educate staff on science of safety 2. Identify local barriers to implementation • Local Opportunities to Improve 2. Identify defects 3. Measure performance • Collaborative learning 3. Assign executive to adopt unit 4. Learn from one defect per quarter 5. Implement teamwork tools 4. Ensure all patients get the evidence • Engage • Educate • Execute • Evaluate Technical Work Adaptive Work http://www.hopkinsmedicine.org/armstr ong_institute 13 We’re Building on Previous Successes • Michigan Keystone ICU program – Reductions in central line-associated blood stream infections (CLABSI) 1,2 – Reductions in ventilator-associated pneumonias (VAP) 3 • National On the CUSP: Stop BSI program 4 1. N Engl J Med 2006;355:2725-32. 2. BMJ 2010;340:c309. 3. Infect Control Hosp Epidemiol. 2011;32(4): 305-314. 4. www.onthecuspstophai.org 14 Percent of Units with Zero CLABSIs and Achieving Project Goal (<1/1000 CL days) *Data drawn from Interim Project Report – Figure 5 – Cohorts 1 through 3 www.onthecuspstophai.org 15 We Focus on Systems, Not Individuals • Harm is preventable – Many healthcare acquired infection and complications are preventable; should be viewed as defect • Technical and adaptive work – Engaging frontline staff to identify and fix local opportunities to improve • Framing as social problem that can be solved – Clinical communities Questions? Email the SUSP help desk! SUSP@jhmi.edu 16 Wrong-patient, Wrong-site, Wrong-procedure Events Reviewed by The Joint Commission The Joint Commission, Sentinel Event Data; http://www.jointcommission.org/assets/1/18/E vent_Type_Year_1995-2011.pdf;29. 17 How is SUSP Different? • Informed by science • Led by clinicians and supported by management • Guided by measures – local and national Questions? Email the SUSP help desk! SUSP@jhmi.edu 18 SUSP Interventions No single SSI prevention bundle • Deeper dive into SCIP measures to identify local defects • Emerging evidence – Abx redosing and weight based dosing – Maintenance of normogylcemia – Mechanical bowel preparation with oral abx – Standardization of skin preparation • Capitalize on frontline wisdom – CUSP/Staff Safety Assessment 20 Auditing tools • Antibiotic – Selection, dosing, redosing • Normothermia • Glucose Control • Skin Prep • SSI investigation • Others Questions? Email the SUSP help desk! SUSP@jhmi.edu 21 Comprehensive Unit-based Safety Program (CUSP) 1. Educate staff on science of safety 2. Identify defects 3. Assign executive to adopt unit 4. Learn from one defect per quarter 5. Implement teamwork tools Questions? Email the SUSP help desk! SUSP@jhmi.edu Briefings and Debriefings • Reductions in communication breakdowns and OR delays 1 • Reductions in procedure and miscommunicationrelated disruptions and nursing time spent in core 2 • Improved communication and teamwork, feasible given current workload 3 • Reductions in rate of any complications, SSI and Arch Surg. 2008;143(11): 1068-1072. mortality 4 1 2J Am Coll Surg. 2009;208:1115-1123. 3 Jt Comm J Qual Saf. 2009;35(8):391-397. 23 4 N Engl J Med. 2009;360:491-9. What data will teams need to collect?* • Monthly NHSN and/or NSQIP SSI data by surgical specialty area – Numerator and denominator • Annual teamwork/culture data using the AHRQ Hospital Survey of Patient Safety (HSOPS) • Will work with CEs to ensure data reporting meets their needs *If data is already collected/available (ie: ACS NSQIP or NHSN), we will work with your team to import if you desire Questions? Email the SUSP help desk! SUSP@jhmi.edu 24 Surgical Site Infection Data Entry: NSQIP • Target audience: Coordinating Entities and hospital administrators • Data transferred directly from NSQIP • Unadjusted data transferred on a monthly basis • Adjusted data (Odds) transferred every 6 months Questions? Email the SUSP help desk! SUSP@jhmi.edu 25 Surgical Site Infection Data Entry: NHSN & Manual Entry • Data transfer process – done by the coordinating entities or hospital administrator • Unadjusted data transferred on a monthly basis • Adjusted data (SIR) transferred every 6 months Questions? Email the SUSP help desk! SUSP@jhmi.edu 26 What do teams need to do? – Attend the Cohort 5 kickoff webinar (~2 hours) • Monday, April 28 @ 10AM (EST) OR • Wednesday, April 30 @ 2PM (EST) – Assemble a multidisciplinary team • Including Preop, OR and Postop staff – Participate in monthly project webinars • All webinars recorded and archived online – Participate in monthly coaching calls – Regularly meet as a team to implement interventions and monitor performance Questions? Email the SUSP help desk! SUSP@jhmi.edu 27 Once enrolled, the SUSP website is your go to place for everything! armstrongresearch.hopkinsmedicine.org • Previously recorded cohort project call webinars • Manuals • Toolkits • Data portal – Who uses the portal? • • • • SUSP project leads HSOPS coordinators SSI data coordinators Coordinating Entities – What’s the portal used for? • • • Data viewing, summation, sharing Hospital Survey of Patient Safety (HSOPS) Sharing of information • Talk with other SUSP hospitals on our social network! 28 CUSP Works in the OR Colorectal NSQIP SSI Rate at Hopkins (Wick 2012) Wick et al. Implementation of a Surgical Comprehensive Unit-Based Safety Program to Reduce Surgical Site Infections. J Am Coll Surg. 2012; 215 (2). 29 Why should you be a part of SUSP? • Improve patient outcomes – ACS NSQIP comparative feedback • Platform that links data collection, reporting, and training with social networking to improve communication and sharing • Finding ‘value’ in our work • Teams own their own data for publication Questions? Email the SUSP help desk! SUSP@jhmi.edu 30 What are current SUSP hospitals saying? 31 Join us on our journey to improve the safety of our patients! How to enroll or recruit hospitals into SUSP • Everything you need is online! – Download ALL enrollment documents online! – Complete the team registration form online! Visit the SUSP recruitment website Have questions? Email the SUSP help desk! SUSP@jhmi.edu 32 State hospital associations: Important due dates and deadlines • By March 21: Complete the Coordinating Entity Participating Agreement and email to SUSP@jhmi.edu or fax to 410-637-4380. • Download the Coordinating Entity Project Manual for guidance on kick-starting your recruiting efforts Everything you need is here: SUSP recruitment website Have questions? Email the SUSP help desk! SUSP@jhmi.edu 33 Hospitals: Important due dates and deadlines • By April 9: Have your hospital leadership complete the Hospital CEO Participating Agreement • By April 16: Complete three additional forms – Online Project Team Registration Form – Data Use Agreement – Clinical Team Participating Agreement • Upload copies of these forms when submitting the Online Project Team Registration Form. You can also return the forms to the SUSP help desk at SUSP@jhmi.edu or by fax: 410-637-4380 Everything you need is here: SUSP recruitment website Have questions? Email the SUSP help desk! SUSP@jhmi.edu 34 Next steps • Visit our recruitment website – CEs: begin recruiting hospitals – Independent hospitals: Return all enrollment forms to SUSP@jhmi.edu no later than April 16. Have questions? Email the SUSP help desk! SUSP@jhmi.edu Questions? Email the SUSP help desk! SUSP@jhmi.edu 35 SUSP from the CE perspective Dana Bonistalli Project Manager, Quality Policy & Advocacy Maryland Hospital Association 18 hospitals enrolled and engaged in SUSP! 36