functions and structure of a medical school
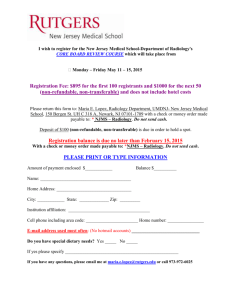
advertisement

BACKGROUND INFORMATION ABOUT THE MEDICAL SCHOOL a. Insert a copy of the medical school’s current entry in the AAMC Directory of American Medical Education and indicate the year of the entry. We have submitted an updated request to be published in the 2013 directory. LCME/CACMS Medical Education Database 2012-2013 I. Institutional Setting Academic Year _2011-2012_ Page |2 Academic Year _2011-2012_ LCME/CACMS Medical Education Database 2012-2013 Page |3 I. Institutional Setting Academic Year _2011-2012_ Page |4 b. Indicate on a separate page any changes in administrative positions or personnel that have taken place since the directory was published. Changes in Administrative Positions: President: Following the resignation of Dr. William Owen as President of UMDNJ, Dr. Denise V. Rodgers was named Interim President by the UMDNJ Board of Trustees. Department and Division or Section Chairs: Basic Sciences: Chair, Cell Biology and MolecularMedicine: Following a national search the interim Chair Dr. Junichi Sadoshima was named the permanent Chair. This appointment is pending approval by the UMDNJ Board of Trustees. Chair, Pathology & Laboratory Medicine: Following the resignation of Dr. Stanley Cohen as Chair (to assume the role of Director, Center for Biophysical Pathology), Dr. Seena Aisner was named Interim Chair and approved by the UMDNJ Board Trustees. Clinical Sciences: Chair, Anesthesiology: Following a national search the interim Chair Dr. Melissa Davidson was succeeded by Dr. Alex Bekker as Chair of Anesthesiology. This appointment was approved by the UMDNJ Board of Trustees. Chair, Family Medicine: Following the resignation of the Interim Chair, Dr. Robin Schroeder, Dr. Chantal Brazeau assumed role of Interim Chair. Medicine: Chair, Medicine: Following a national search, the Interim Chair Dr. Bunyad Haider was succeeded by Dr. Marc Klapholz as Chair of Medicine. This appointment was approved by the UMDNJ Board of Trustees. Division Chiefs: Following the retirement of the Dr. Haggerty, Dr. Ana Natale-Pereira assumed the role of Chief, Academic Medicine, Geriatrics and Community Programs. The Division of Pulmonary and Critical Care now includes Allergy, Immunology and Rheumatology with Dr. Andrew Berman as Chief. Chair, Neurological Surgery: Following a national search after the resignation of Dr. Peter Carmel as Chair (to assume the Presidency of the American Medical Association and the role of Director at NJMS Neurologic Institute of New Jersey), Dr. Charles Prestigiacomo was named Chair of Neurological Surgery. This appointment was approved by the UMDNJ Board of Trustees. Ophthalmology and Visual Science: The Division of Ophthalmic Pathology was eliminated. Dr. Monique Roy, assumed the role of the new Division of Retinal Degenerative and Retinal Vascular Disease. Orthopaedics: Academic Year _2011-2012_ Page |5 Following the resignation of Dr. John Capo, Dr. Virak Tan assumed the role of Chief, Hand Injuries and Disorders. Chair, Otolaryngology-Head & Neck Surgery: Following a national search initiated after the designation of Otolaryngology-Head & Neck Surgery as a new department at NJMS, Dr. Soly Baredes was named Chair following his tenure as Interim Chair. This appointment was approved by the UMDNJ Board of Trustees. Pediatrics: Division Chiefs: Dr. Claire K. McMahon assumed the role of Chief, Cardiology. Dr. Jose R. Antillon, former Chief is scheduled to retire. Dr. Brenda Harris assumed the role of Chief of the Division of Child Development. Dr. Noah Kondamudi replaced Dr. Robert Barricella as Chief, Emergency Medicine. Chair, Physical Medicine & Rehabilitation: Following the retirement of Dr. Joel DeLisa as Chair, Dr. Patrick Foye was named Interim Chair. Chair, Psychiatry Following a national search, the Interim Chair Dr. Giovanni Caracci will be succeeded by Dr. Petros Levounis as Chair of Psychiatry who will join NJMS in March 2013. This appointment is pending UMDNJ Board of Trustees approval. Surgery: Dr. Alicia Mohr was named Interim Chief, Critical Care. Chief of the Division of General and Minimally Invasive Surgery is currently vacant. Associate Dean for Education (new): Dr. Sangeeta Lamba assumed the role of Associate Dean. c. Provide a brief history of the medical school, noting any key points in the school’s historical development. (the information below can be found at http://www.umdnj.edu/about/about03_history.htm) The New Jersey Medical School (NJMS), founded in 1954, is the oldest school of medicine in the constellation of health sciences schools which comprise the University of Medicine and Dentistry of New Jersey (UMDNJ). In 1956, eighty students entered the first class of then Seton Hall College of Medicine and Dentistry located in the Jersey City Medical Center. In 1965, the State of New Jersey acquired the Seton Hall College of Medicine and Dentistry, assuming the name of the New Jersey College of Medicine and Dentistry (NJCMD). In 1968 the medical school relocated to Newark to temporary facilities. With its relocation, the 1968 “Newark Agreements”, a historic social contract among federal, state and local governments and the Newark community cleared the way for the construction of a major academic health center in Newark's Central Ward. With it came the commitment to provide healthcare, educational and employment opportunities to its largely disadvantaged and minority residents. At the same time, the New Jersey College of Medicine and Dentistry assumed operation of Newark City Hospital from the city and renamed it the Harrison S. Martland Medical Unit of NJCMD. In 1970 the Medical and Dental Education Act established the College of Medicine and Dentistry (CMDNJ) under one Board of Trustees through the merger of the NJCMD and Rutgers Medical School. The medical school was renamed the New Jersey Medical School (NJMS). The Newark campus, which included the Medical Science Building, the dental school building, the Community Mental Health Center, and the George F. Smith Library of the Health Sciences, was dedicated on May 10, 1976. The School of Health Related Professions (then called CMDNJ-School of Academic Year _2011-2012_ Page |6 Allied Health Professions) established on the Newark campus as a separate school. In 1977, NJMS moved to its current location with the opening of the Medical Science Building (MSB) and in 1979 College Hospital opened replacing Harrison S. Martland. In 1981 the University of Medicine and Dentistry of New Jersey (UMDNJ) was established and included NJMS as one of its schools and College Hospital as its core educational and clinical facility. In 1982, College Hospital became University Hospital, continuing its role as the principal teaching hospital for NJMS. The UMDNJ-New Jersey Medical School Doctors Office Center opened on the Newark campus, with dedication ceremonies on June 10, 1992. The UMDNJ-School of Nursing established as the seventh school of the University in the same year. In 1994, NJMS was the recipient of the Spencer Foreman Award for Outstanding Community Service, presented by the AAMC in recognition of the School’s commitment to health of the communities it serves and became the second school in the US to host a White Coat Ceremony. The University's founding President, Dr. Stanley S. Bergen, Jr., retired and became Founding President Emeritus. The Martland Building renamed the Stanley S. Bergen Building. Dr. Stuart D. Cook named President on November 23, 1998. The University established its eighth school, the UMDNJ-School of Public Health on the Piscataway/New Brunswick campus in collaboration with Rutgers. A new Master of Public Health Program would be offered in 1999 on the Newark campus in collaboration with Rutgers-Newark and NJIT. A ground-breaking ceremony for the New Jersey Medical School International Center for Public Health (ICPH) was held in Newark on September 13, 2000. The Public Health Research Institute (PHRI) relocated from New York into the ICPH building initially as a separate entity in 2002 and was established as a center of UMDNJ–NJMS in 2006. PHRI’s faculty members study a broad range of infectious disease issues. Distributed within the five regional campuses across the state UMDNJ is comprised of the New Jersey Medical School, New Jersey Dental School, School of Health Related Professions, Graduate School of Biomedical Sciences, School of Nursing, Robert Wood Johnson Medical School, School of Osteopathic Medicine and School of Public Health as well as University Hospital and the University Behavioral HealthCare. The University's Board of Trustees approved the Corporate Integrity Agreement (CIA) with the Office of the Inspector General, U.S. Department of Health and Human Services in 2009. CIA marks the last step in a chain of measures implemented in the University's settlement covering two separate cases relating to billing actions taken as far back as 1993. The University is currently in year 4 of this agreement that requires a robust compliance program which includes a Code of Conduct, written policies and procedures, an education and training component, mechanisms for ongoing monitoring and auditing of UMDNJ's operations to assess compliance, mechanisms for employees and agents to report incidents of noncompliance in an anonymous manner, and disciplinary actions. The New Jersey Medical and Health Sciences Education Restructuring Act passed by the New Jersey Senate and General Assembly on June 28, 2012, and signed by Governor Chris Christie on August 22, 2012. On November 19, 2012 the final legislation signed by Governor Christie was approved by both the Rutgers Board of Governors and the Board of Trustees on November 19, 2012. This becomes effective July 1, 2013. This statute transfers all units of UMDNJ, except University Hospital in Newark and the School of Osteopathic Medicine in Stratford, to Rutgers University. This historic legislation will strengthen medical and health sciences education in New Jersey and propel Rutgers, the state's flagship university, into the very top tier of national research universities. The resulting integrated organization builds on the rich histories, talent, and expertise of both institutions and establishes a milestone that begins a promising era for New Jersey. The individuals who have served as Dean, include: Charles L. Brown, MD (1955-59); James E. McCormack, MD (1960-66); Arthur J. Lewis, MD (1966); Desmond Bonnycastle, MD, PhD (acting 1967); Rulon Rawson , MD (1967-72); Harold Kaminetsky, MD (acting dean and dean, 1972-74); Stanley S. Bergen , Jr., MD (acting 1974); Vincent Lanzoni, MD, PhD (1975-87); Stuart D. Cook, MD (acting 1987-89); Ruy V. Lourenço, MD (December 1989-June 2000); Joel A. DeLisa, MD, MS (interim Academic Year _2011-2012_ Page |7 July 2000- December 2000); Russell T. Joffe, MD (January 2001-Sept 2005); and Robert L. Johnson, MD (interim October 2005-2011 and dean 2011-present). Effective July 1, 2013, the majority of schools, institutions, and centers that currently compose UMDNJ will transfer to Rutgers University and will be organized within the newly created Rutgers Biomedical and Health Sciences (RBHS). RBHS will include seven schools from UMDNJ: New Jersey Medical School, New Jersey Dental School, Robert Wood Johnson Medical School, the School of Nursing, the School of Health Related Professions, the School of Public Health, and the Graduate School of Biomedical Sciences, as well as University Behavioral HealthCare. RBHS will also include the following Rutgers units: Ernest Mario School of Pharmacy; the College of Nursing; the Institute for Health, Health Care Policy and Aging Research; and any other schools, institutes, or centers as directed by Rutgers President Robert L. Barchi. The Cancer Institute of New Jersey, one of the nation's 41 National Cancer Institute-designated Comprehensive Cancer Centers and the only one in New Jersey, will also become part of Rutgers University. It will be an independent institute within the university. The Dean of NJMS will report directly to the Chancellor of Rutgers Biomedical and Health Sciences, along with the other deans of the schools of RBHS. C. Complete the following table with data from the previous and current full surveys:* Need the years for both look at previous database. Previous Survey Year Current Survey Year 2004 2011 Entering class size 170 178 Total enrollment 693 751 Residents and fellows 568** 559 ** Full-time basic science faculty 147 97 Full-time clinical faculty 378 546 ($ in Millions) Total revenue from tuition and fees 16,229 23,259 University and government appropriations 77,411 66,789 Research/training grants, direct 69,659 79,197 Indirect cost recoveries 16,944 22,387 Practice plan income 64,897 90,433 Revenue from clinical affiliates 83,139 110,362 Other revenues 8,092 2,815 Gifts and endowment 727 2,969 Total revenues 337,098 398,211 * Indicate the year of the previous survey visit in the table. If the data come from a different year, indicate this year by an asterisk. ** This figure excludes pediatric dental, oral-maxillofacial surgery, and podiatry residents. Academic Year _2011-2012_ Page |8 SECTION I. INSTITUTIONAL SETTING Part A: Key Quantitative Indicators Please provide the following information. For U.S. medical schools, use the school’s copy of the Longitudinal Statistical Summary Report (LSSR) as the data source, unless otherwise indicated. Include data for 2010-2011, if available. a. Number of vacant department chair positions for each of the following academic years # of chair vacancies 2005-06 2006-07 2007-08 3 4 4 2008-09 2009-10 2010-11 2011-12 6 5 10 10 b. Total numbers of students enrolled in medical school-sponsored undergraduate programs; Master’s and doctoral degree programs in the biomedical sciences; other professional degree programs; and certificate programs Undergraduate programs (e.g., BA/BS) Master’s program(s) in biomedical sciences Doctoral program(s) in biomedical sciences Other professional degree program(s) (e.g., MPH, DrPH) Certificate programs 2005-06 2006-07 2007-08 2008-09 2009-10 2010-11 2011-12 157 143 119 148 185 232 187 146 168 160 211 272 315 239 188 175 191 173 196 186 162 20 17 20 20 14 18 17 0 0 12 4 5 4 4 c. Total numbers of residents and clinical fellows on duty in ACGME-accredited programs (for U.S. medical schools) or in RCPSC or CFPC-accredited programs (for Canadian medical schools) that are the responsibility of the medical school faculty Residents Fellows 2005-06 512 67 2006-07 521 68 2007-08 526 71 2008-09 530 69 2009-10 526 68 2010-11 491 65 2011-12 500 59 Academic Year _2011-2012_ Page |9 d. Percentage of graduating medical students who participated in a research project with a faculty member (Source: AAMC Medical School Graduation Questionnaire) % participation 2005-06 75.8 2006-07 77.8 2007-08 68.6 2008-09 78.8 2009-10 71.4 2010-11 60.7 2011-12 73.1 e. Percentage of graduating medical students who participated in a service-learning project. (Source: AAMC Medical School Graduation Questionnaire) % participation 2008-09 0* * No response provided. 2009-10 20.8 2010-11 22.0 2011-12 80.0 Academic Year _2011-2012_ Page |10 SECTION I. INSTITUTIONAL SETTING Part B: Narrative Data and Tables IS-1. An institution that offers a medical education program must engage in a planning process that sets the direction for its program and results in measurable outcomes. To ensure the ongoing vitality and successful adaptation of its medical education program to the rapidly changing environment of academic medicine, the institution needs to establish periodic or cyclical institutional planning processes and activities. Planning efforts that have proven successful typically involve the definition and periodic reassessment of both short-term and long-term goals for the successful accomplishment of institutional missions. By framing goals in terms of measurable outcomes wherever circumstances permit, the institution can more readily track progress toward their achievement. The manner in which the institution engages in planning will vary according to available resources and local circumstances, but it should be able to document its vision, mission, and goals; evidence indicating their achievement; and strategies for periodic or ongoing reassessment of successes and unmet challenges. __________________________________________________________________________________ a. Provide a brief statement of the mission and goals of the medical school. When were these last reviewed and/or revised? Mission, Vision, Values and Goals of New Jersey Medical School Approved by Faculty Council November 13, 2012 The Mission of New Jersey Medical School is to meet the needs of the local and global community through outstanding education, pioneering research, cutting edge clinical care, and public service. New Jersey Medical School’s Vision is that it aspires to optimize health and social well-being by: 1. Preparing humanistic leaders in global healthcare through education of physicians and scientists, building on our strength of diversity, hands-on clinical training, urban healthcare programs and transformative research; 2. Providing cutting edge tertiary and quaternary medical care of distinction, serving patients from New Jersey and beyond; 3. Enhancing our position as the top biomedical research institution in the State of New Jersey; 4. Advancing the health, education and care of the underserved and vulnerable populations by preparing a competent and diverse workforce. New Jersey Medical School Values Integrity Excellence Diversity Humanism Compassion Professionalism Leadership Innovation New Jersey Medical School has committed to 4 Goals that will serve as the focus of its activities and investments over the next 5 years. These include: 1. Deliver outstanding, compassionate, coordinated patient care to meet complex health care needs of our region and beyond. Academic Year _2011-2012_ Page |11 2. Build on our prominence in biomedical research that promotes innovative clinical, population-based and translational research programs 3. Develop innovations in education to prepare students and trainees from diverse backgrounds to be collaborative practitioners of medicine, educators and researchers with a focus on the health of underserved and vulnerable populations. 4. Share our successes internally and externally in ways that build the strength of NJMS and generate pride in our institution. b. Provide an executive summary of the medical school’s current strategic plan, if any. Note if the strategic plan was developed independently of or in collaboration with the parent university or the health system. The New Jersey Medical School Strategic Plan (the Plan) charts the strategic direction of NJMS for a five year period, from December 2012 to December 2017. This document provides the School with a background understanding of the process undertaken in its creation, as well as the “lens” through which the school would continue to conduct self-assessment and examination. The Plan clearly states the Mission, Vision and Values of NJMS, re-committing ourselves to diversity, integrity, excellence, humanism, compassion, professionalism, leadership and innovation. The Plan considers the strengths, challenges, opportunities and threats facing NJMS today, and taking these into account, and outlines NJMS’ future in terms of attainment of the four (4) Goals. These goals serve as the focus of our activities and investments over the next five years: Following each Goal as stated above, a rationale, select supporting strategies and measures of success are articulated. The supporting strategies are designed to be broad institutional activities in support of the goal, and were not designed to be task-lists or project plans to achieve the Goal. This Strategic Plan has received broad NJMS support from the Dean, the Senior Management Team, the Institutional Planning and Development Committee and the Faculty Council. While the Strategic plan was developed independent of the University, the Dean engaged in regular conversations with the UMDNJ President (Interim). We believe that this plan will chart our future for the next five years. c. Date of most recent review and/or revision of the strategic plan: 5/2011 d. How often is the strategic plan reviewed and/or revised? Every five years. Beginning in 5/2011, a new strategic plan initiative was undertaken and approved in November 2012. e. Briefly summarize or outline the planning process for the strategic plan, including the main participants and the names or titles of individuals or groups whose approval is required to finalize and approve it. NJMS Strategic Planning Process Immediately following the March 2011 appointment of Dr. Robert Johnson as permanent Dean following his interim status, Dr. Johnson articulated his vision of a process which would encourage as many individuals as possible to begin thinking about New Jersey Medical School’s collective future. In May of 2011, as part of his inaugural address, Dean Johnson launched his “New Beginnings” strategic planning process. He designated a core team including Dr. Anne Mosenthal and Dr. Vivian Bellofatto as steering committee co-chairs. A Steering Committee consisting of 31 members was formed, and it was their task Academic Year _2011-2012_ Page |12 to “morph” the vision into a process that created a mechanism to look at our School differently than the ways we had been used to. Rather than assess our success in terms of our mission areas: Teaching, Research, Clinical Care and Community Service, we gauged our progress through the following Work Groups: o Integration and Alignment (22 members) o Education (21 members) o Faculty Recruitment, Retention and Leadership (16 members) o Branding and Image (25 members) o Funds Flow and Incentives (17 members) o Integrated Multi-Specialty Faculty Practice (17 members) o 3,000-Foot View (5 members) This approach helped us to think outside the comfort zones of our Mission areas, and assess ourselves in a cross-functional way. As this important work was being done, decisions were being made regarding the future of our parent organization, the University of Medicine and Dentistry of New Jersey, and we had to determine how we would continue our successes in a number of differing, often-times competing scenarios. As we neared the end of our process, the Governor of the State of New Jersey signed legislation which stated that most of the schools of UMDNJ, including NJMS, were to be incorporated into Rutgers University. This restructuring also includes a new governance structure for University Hospital as an independent state entity, which will remain a state hospital and the Principal Teaching Hospital for NJMS. It provides for the possibility of University Hospital’s affiliation with a non-profit health system. While these events have created some transitions within the organization, they provide NJMS with a significant opportunity for culture change, growth and a new direction. The Strategic Planning process established a strategic direction for New Jersey Medical School that guides our actions, activities, and investments over the next five years in ways that strengthen our regional, national, and international reputation as leaders in academic medicine. The Dean’s charge to the steering committee, which originally had 31 members and included representation from the NJMS faculty, staff, administration and student body, University Physician Associates (UPA) a separately incorporated faculty practice plan, University Hospital administration, and Graduate School of Biomedical Sciences faculty and students, is outlined below: Redefinition of the school’s mission and vision while maintaining its core values of discovery, educational excellence, diversity and service to the community; Creation of a sense of optimism and transformation to a stronger, unified organization focused on a common purpose; Wide engagement of diverse groups of faculty, staff and students at all levels, in imagining a new direction for themselves and our institution; Development of an innovative, achievable strategic plan which would position NJMS for success in the rapidly changing University and healthcare environment. To examine the Dean’s charge, the steering committee held a kick-off summit in June 2011 in which the following themes emerged: Educating physicians and scientists to serve a diverse global community, as required by the evolving healthcare environment; Integrating our clinical practice across all departments; Transitioning to a financially strong medical school; Increasing recognition of the talents and missions of NJMS through strengthening our brand; Developing and aligning a unified mission and vision. Academic Year _2011-2012_ Page |13 Following this, the steering committee established Work Groups to design an inclusive and collaborative process involving faculty, academic department chairs, deans, students, faculty practice representatives and hospital leadership to identify and develop: The School’s strengths and weaknesses; Strategic assumptions about our future; The current state of NJMS—our strengths and the challenges we face; and Goals and supporting strategies for our Strategic Plan. In July 2012, the school-wide New Beginnings Strategic Planning Retreat was held. Retreat invitees included representatives from all NJMS constituencies. Specifically, participants included NJMS senior leadership, academic department leadership, clinical and basic science faculty, administrative staff, graduate and medical students representatives, UPA practice plan leadership and affiliate leadership. The retreat included a review of each Work-Group’s final report and recommendations for the key strategies which addressed priorities and common goals. These extensive efforts put forth by the Work Groups and the larger retreat with over 100 participants guided and informed the development of the strategic plan. The final draft of the Strategic Plan was presented and approved by the Institutional Planning and Development Committee, a standing committee of the NJMS Faculty Council, on November 7, 2012. The Strategic Plan was then approved by the NJMS Faculty Council on November 13, 2012. Academic Year _2011-2012_ Page |14 IS-2. A medical education program should be, or be part of, a not-for-profit institution legally authorized under applicable law to provide medical education leading to the M.D. degree. ___________________________________________________________________________________ a. Year of formation: 1954 b. State (province) of organization or incorporation: New Jersey c. Type of entity (check one): X Not-for-profit corporation For-profit corporation Limited liability company Other, describe below If the medical school is part of a for-profit/investor-owned company, provide the name and location of the parent company; a copy of its most recent audited financial statement; and copies of its three most recent Form 10-Ks filed with the Security and Exchange Commission, if publicly traded. Also provide a copy of its most recent annual report. Academic Year _2011-2012_ Page |15 IS-3. If a U.S. medical education program is not a component of a regionally accredited institution, the parent institution for the program must achieve institutional accreditation from the appropriate regional accrediting body. The LCME is recognized by the U.S. Department of Education as an accrediting agency for medical education programs leading to the M.D. degree. Because the LCME is not recognized as an institutional accrediting agency, it lacks standing to accredit stand-alone medical schools as institutions of higher education. Institutional accreditation is granted by regional accrediting agencies and is required to qualify for federal financial assistance programs authorized under Title IV of the Higher Education Act. Some regional accrediting bodies grant "pre-accreditation" as a first step to achieving full accreditation. In such circumstances the attainment of preaccreditation status would meet the requirements of this standard. __________________________________________________________________________________ a. Accredited by the following regional accrediting body (check one): X Middle States Association of Colleges and Schools New England Association of Schools and Colleges North Central Association of Colleges and Schools Northwest Commission on Colleges and Universities Southern Association of Colleges and Schools Western Association of Schools and Colleges b. Current institutional accreditation status: Accredited c. Year of next regional accreditation survey: 2017 UMDNJ submitted its Periodic Review Report in June, 2012 and reaffirmed in November. As discussed previously, the New Jersey Medical and Health Sciences Education Restructuring Act passed by the New Jersey Senate and General Assembly on June 28, 2012, and signed by Governor Chris Christie on August 22, 2012, becomes effective July 1, 2013. This statute transfers all UMDNJ units, except University Hospital in Newark and the School of Osteopathic Medicine in Stratford, to Rutgers University. Rutgers University Periodic Review Report is due June, 2013. The Substantive Change Request was submitted to Middle States in December 2012 from UMDNJ, Rutgers University and Rowan University as three separate requests. Academic Year _2011-2012_ Page |16 IS-4. The manner in which an institution that offers a medical education program is organized, including the responsibilities and privileges of administrative officers, faculty, medical students, and committees must be promulgated in programmatic or institutional bylaws. ___________________________________________________________________________________ a. Provide a copy of the faculty bylaws that apply to the medical school or the URL of the Web site at which they can be viewed. http://njms.umdnj.edu/faculty_org/NJMSBylawsapproved-BOT3211.cfm (See IS Appendix 1) b. Date of the most recent bylaws revision: 3/2011 c. Describe the process for approval of bylaws changes. The New Jersey Medical School has a detailed set of bylaws that are reviewed periodically by the Bylaws committee. Changes approved by this committee are posted on the faculty organization website discussion group and are brought for final discussion by the entire faculty at a faculty organization meeting. Following discussions and a vote, the by-laws are presented to the faculty council of NJMS for approval and then, through the Dean, to the Board of Trustees for final approval. The approved bylaws are found at http://njms.umdnj.edu/faculty_org/NJMSBylawsapprovedBOT3211.cfm d. Briefly describe how the bylaws are made available to the faculty. Upon approval by the University Board of Trustees, they are available on the NJMS website, http://njms.umdnj.edu/faculty_org/index.cfm Academic Year _2011-2012_ Page |17 IS-5. The governing board responsible for oversight of an institution that offers a medical education program must have and follow formal policies and procedures to avoid the impact of conflicts of interest of members in the operation of the institution and its associated clinical facilities and any related enterprises. There must be formal policies and procedures at the institution to avoid the impact of conflicts of interest (e.g., the requirement that a board member recuse him or herself from any discussion and vote relating to a matter where there is the potential for a conflict of interest to exist). The institution also must provide evidence (e.g., from board minutes, annual signed disclosure statements from board members) that these policies and procedures actually are being followed. Some conflicts related to personal or pecuniary interests in the operation of the institution may be so pervasive as to preclude service on the governing board. IS-6. Terms of governing board members of an institution that offers a medical education program should be overlapping and sufficiently long to permit them to gain an understanding of its program. a. Provide the name of the governing board with responsibility for the medical school. Kevin M. Barry, M.D. b. Check all units for which this governing board is directly responsible: X X X X Parent University Health Science Center Medical School Other (describe below) Behavior Health Care Network c. Provide the names and the occupations/affiliations of the current governing board members, along with their dates of initial appointment. If the medical school is, or is part of, a for-profit/investor-owned company, identify any board members who are shareholders/investors in the holding company for the medical school. If the medical school is part of a for-profit/investor-owned company, does it have a subsidiary board whose members are not shareholders/investors in order to reduce opportunities for conflicts of interest? Provide the names and occupations/affiliations of the members of the subsidiary board. Trustee Appointment Reappointment Kevin M. Barry, M.D. Chairperson January 2007 2010 (seat change assumed role as Chair) Mary Ann Christopher, RN, MSN, FAAN Vice Chairperson June 2006 December 2007 Initial Expiration 2010 2007 Affiliation Anesthesia Associates of Morristown 264 South Street Morristown, NJ 07960 Visiting Nurse Service of New York 107 East 70 th Street New York, NY 10021 Academic Year _2011-2012_ Page |18 Kevin M. Covert, Esq. March 2007 2012 Honeywell International 101 Columbia Road AB -2 Morristown, NJ 07962 David Critchley* December 2010 2015 United Union of Roofers, Waterproofers, & Allied Workers 385 Parsippany Road Parsippany, NJ 07054 Michael Critchley, Jr.,* June 2007 2011 Critchley, Kinum &Vazquez, LLC September 2010 2014 Infecdetect LLC 151 Brooks Bend Princeton, NJ 08540 Bradford W. Hildebrandt June 2007 2011 Hildebrandt Consult 25 Angel Place Somerset, NJ 08873 Marilyn Penny Joseph February 2011 2015 Panasonic Corporation of North America One Panasonic Way, 3G-7 Ira P. Monka, DO, MHA, September 2010 2013 The Medical Institute of New Jersey 11 Saddle Road Cedar Knolls, NJ 07927 Mary E. O’Dowd, MPH March 2011 Ex-Officio Commissioner, NJ Department of Health and Senior Services Market Street & John Fitch Plaza CN 360 Trenton, NJ 08625 Esq. Christine Grant, J.D., MBA *Trustees are appointed by the Governor of New Jersey and the Legislature; appointment is ratified by the New Jersey State Senate. These two trustees are distant relatives and were not considered to present a conflict of interest as deemed not to h d. Year of the governing board chair’s initial appointment as chair and length of the board chair’s term(s) of office. Year of initial appointment: September 2010 Length of term(s) of office: Four Years Academic Year _2011-2012_ Page |19 e. Summarize the procedures for the appointment and renewal of governing board members, including the procedures for the chair. Describe the length of members’ terms, the number of times that a member can be reappointed, and the system for staggering of appointments, if appropriate. “The Board shall be composed of 19 voting members. The Governor shall designate one of the voting members as chairman of the Board. The Board shall select such other officers from among its members as shall be deemed necessary. A voting member shall serve for a term of five years and shall serve until his success is appointed and has qualified. In the case of the initial terms of the additional members of the Board appointed pursuant to P.L. 2006, c.95 three members shall serve for a term of five years, three members shall serve for a term of four years, and two members shall serve for a term of three years. Any vacancies in the voting membership of the Board occurring other than by expiration of term, shall be filled in the same manner as the original appointment but for the unexpired term”. Effective July 1, 2013, the majority of schools, institutions, and centers that currently compose UMDNJ will transfer to Rutgers University and will be organized within the newly created Rutgers Biomedical and Health Sciences (RBHS). RBHS will include seven schools from UMDNJ: New Jersey Medical School, New Jersey Dental School, Robert Wood Johnson Medical School, the School of Nursing, the School of Health Related Professions, the School of Public Health, and the Graduate School of Biomedical Sciences, as well as University Behavioral HealthCare. RBHS will also include the following Rutgers units: Ernest Mario School of Pharmacy; the College of Nursing; the Institute for Health, Health Care Policy and Aging Research; and any other schools, institutes, or centers as directed by Rutgers President Robert L. Barchi. The Cancer Institute of New Jersey, one of the nation's 41 National Cancer Institute-designated Comprehensive Cancer Centers and the only one in New Jersey, will also become part of Rutgers University. It will be an independent institute within the university. The UMDNJ Board of Trustees will be dissolved effective July 1, 2013. As per the “New Jersey Medical and Health Sciences Education Restructuring Act,” a new campus advisory board will be formed. (http://ru-umdnjtogether.rutgers.edu/): “21. Notwithstanding the provisions of N.J.S.18A:65-25 or any other section of law to the contrary, the campus advisory board of Rutgers University-Newark shall: a. advise the president and the board of governors of Rutgers, The State University on the selection of the Rutgers University-Newark chancellor; b. propose capital projects and bonding for Rutgers University-Newark to the board of governors of Rutgers University; and c. propose an annual budget for Rutgers University-Newark to the board of governors of Rutgers University.” f. Provide copies of the policies and procedures intended to prevent or address financial and other conflicts of interest among governing board members (including recusal from discussions or decisions if a potential conflict occurs) and describe the strategies for dealing with actual or perceived conflicts of interest if they arise. Provide examples to illustrate that these policies are being followed. Academic Year _2011-2012_ Page |20 UMDNJ Board (Recusals) Example 1: Finance, Investment, and Administration Committee Report, provided by Mr. X Finance, Investment, and Administration Committee Report, provided by Mr. X: Upon recommendation, the Board accepted the Finance, Investment, and Administration Committee Executive Summary. Mr. X submitted to the Board a Resolution for the approval of seven contracts. BE IT RESOLVED, that the University of Medicine and Dentistry of New Jersey Board of Trustees, upon recommendation of the Finance, Investment and Administration Committee, accepts, ratifies and approves the aforementioned contracts and leases. Mr. X recused himself and left the room prior to the vote on the JFK Occupational Health contract. He returned to the room after the vote on this matter was complete. BE IT RESOLVED, that the University of Medicine and Dentistry of New Jersey Board of Trustees, upon recommendation of the Finance, Investment and Administration Committee, accepts, ratifies and approves the aforementioned contract. Example 2: Legal Committee Report, provided by Mr. Y Following the discussion in Executive Session, the Board approved the recommendations of the Legal Committee regarding the following items: Authorization for Claims A, B, C, D and E. Dr. Z recused himself from the authorization for Claim B. During our last accreditation visit in March 2005, we received a citation regarding IS-5. Both the UMDNJ-New Jersey Medical School and Robert Wood Johnson Medical School provided a progress report dated August 24, 2006 to the LCME secretaries detailing the steps put in place to assure compliance with the standard. Executive Order #65, signed by Acting Governor Codey on November 15, 2005, prohibited every president and governing board member of a State University or State College and every member of their immediate family from doing business with the University or College. Every UMDNJ trustee was required to comply and file an Executive Order 65 Disclosure Form. At the time, three members, including the chair, resigned from the board due to actual or perceived conflicts of interest. The progress report was accepted by the LCME committee. The policies and procedures that are currently in place are described under IS-6 and the website and relevant appendices are also included. The New Jersey State Ethics Commission has adopted the Uniform Ethics Code (http://web.njcu.edu/committees/self-study/Uploads/uniformcodeofethicswebcopy.pdf), (See IS Appendix 2), and it requires that members of governing boards of state universities file Conflict Of Interest forms annually (Executive Order 64 can be found at (http://www.state.nj.us/ethics/forms/college/), (See IS Appendix 3) and the statute can be found at http://www.nj.gov/ethics/statutes/conflicts/index.html, (See IS Appendix 4). The Director of Ethics Programs for UMDNJ monitors this process to ensure that the Board of Trustees adheres to the deadline stipulated by the State Ethics Commission. In addition, each Trustee must undergo ethics training (http://www.nj.gov/ethics/training/online/index.html), (See IS Appendix 5) upon appointment to the Board. Thereafter, the entire Board receives an annual ethics briefing and must undergo training as required under the University Corporate Integrity Agreement. The State Ethics Commission reviews the filing by each member of the Board, and if there are any questions or issues, there is further inquiry to the Board member through the University’s Ethics officer to seek resolution. When concerns regarding conflict of interest on the Board have arisen in the past, the Board member is Academic Year _2011-2012_ Page |21 given a choice between recusal and an alternate management plan. The individual may also choose to resign from the Board of Trustees. Academic Year _2011-2012_ Page |22 IS-7. Administrative officers and members of the faculty must be appointed by, or on the authority of, the governing board of the medical education program or its parent institution. Briefly describe the role of the governing board in the appointment of the administrative officers and the faculty of the medical school. The appointment of administrative officers (designated within our system as faculty administrators) and faculty of New Jersey Medical School (NJMS) occurs in a two tiered manner, the first tier occurring within NJMS and the second tier occurring at the University level by or on behalf of the UMDNJ Board of Trustees. The UMDNJ Board of Trustees reserves the power to appoint faculty, and has delegated such responsibility of approval for junior title faculty, voluntary faculty and non-tenured faculty to the Executive Vice President for Academic and Clinical Affairs. All faculty actions that are deliberated and voted upon by the main governing body of NJMS, the Faculty Council, are considered recommendations to the UMDNJ Board of Trustees. Within NJMS, faculty members are appointed through a series of committees, starting at the departmental level. Once a faculty candidate has been tendered an offer, the department conducts a vote of the senior title faculty. If the faculty candidate is a junior titled faculty member, the faculty is presented to the Faculty Council. If the faculty candidate is proposed as a senior title faculty, the faculty candidate is presented to the Faculty Committee on Appointments and Promotions (FCAP). This route for appointment is followed for faculty candidates regardless of the senior faculty vote. FCAP and Faculty Council can serve as both the recommending and the appealing bodies of a senior title faculty departmental vote. The Faculty Council shall be composed of the Dean, the President, the Past President, the President-Elect and the two Vice Presidents of the Faculty Organization; and the chair or acting chair of all academic departments of the UMDNJ-NJMS. In addition, a number of members of the faculty equal to the number of departmental chairs shall serve on the Faculty Council. The at-large membership shall be elected according to NJMS Bylaws Article VII, Title A, Section 2, and are eligible for re-election. Two representatives of the volunteer faculty shall be elected to the Faculty Council by the at-large members. Four students, one from each year, shall be elected to the Faculty Council by each individual class, and one house officer shall be elected by membership of the house officers' organization. Student and house officer members may participate in discussions and balloting on all issues except faculty appointments and promotions. All Chairs of the faculty standing committees shall be ex officio, non-voting members (in the event the chairs are not current members of the Faculty Council). Faculty Council has delegated part of its responsibility for senior title faculty actions to a specific committee, the Faculty Committee on Appointments and Promotions (FCAP). FCAP is composed of senior title faculty with comparable representation of both basic science and clinical departments. Department chairs are not eligible to serve on FCAP. FCAP membership is selected by the Committee on Committees which consists of the Dean, Vice Dean and the Faculty Organization Officers. FCAP is presided over by a chair who is a full professor. FCAP evaluates proposed appointments and promotions for senior title faculty only, irrespective of track. The FCAP vote, which occurs by secret ballot, serves as a recommendation to Faculty Council. Faculty Council retains the discretion to endorse or override the recommendation of FCAP. The second tier of the faculty appointment process occurs at the University level. Senior title faculty who are proposed for tenure or the tenure track are first evaluated by a committee known as the Dean’s Committee and also a pre-committee of the Board of Trustees known as the Academic Affairs Committee. The Dean’s Committee is comprised of all of the Deans of the respective schools of UMDNJ. The Academic Affairs Committee is comprised of three UMDNJ Board of Trustees members who approve actions to be forwarded to the full Board; the meeting is attended by Deans from each of the Academic Year _2011-2012_ Page |23 eight academic schools, the President, the Executive Vice President for Academic and Clinical Affairs, the Vice President for Academic Affairs, and the Vice Presidents for Legal Management and AA/EEO. The UMDNJ Board of Trustees approves all faculty actions for senior title faculty who are proposed either for tenure or tenure track and for administrative appointments. The approval for the remaining faculty appointments have been delegated by the UMDNJ Board of Trustees to the Executive Vice President for Academic and Clinical Affairs for administrative approval. Faculty administrators must have an underlying faculty appointment, on which their administrative appointment rests. The underlying faculty appointment follows the process described above. The Academic Affairs Committee and the full Board of Trustees approve all faculty administrator appointments. Relevant URLs: New Jersey Medical School Bylaws http://njms.umdnj.edu/docs/NJMSBylaws2011.pdf New Jersey Medical School Faculty Committee on Appointments and Promotions Guidelines http://njms.umdnj.edu/faculty_org/documents/FCAPGuidelinesSeptember2009withcorrections4232012.p df (See IS Appendix 6) UMDNJ Bylaws http://www.umdnj.edu/acadweb/Bylw9-99.pdf (See IS Appendix 7) Academic Year _2011-2012_ Page |24 IS-8. The chief official of a medical education program, who usually holds the title "dean," must have ready access to the university president or other official of the parent institution who is charged with final responsibility for the program and to other institutional officials as are necessary to fulfill the responsibilities of the dean's office. IS-9. There must be clear understanding of the authority and responsibility for matters related to the medical education program among the vice president for health affairs, the chief official of the medical education program, the faculty, and the directors of the other components of the medical center and the parent institution. a. Provide the position description for the dean and, if applicable, the vice president for health affairs or equivalent. The Dean of New Jersey Medical School provides entrepreneurial leadership for its academic, research, and clinical programs; provides an opportunity to guide an outstanding medical school within a dedicated health sciences university to its next levels of achievement. The Dean has direct management oversight for University Hospital and driving the development of robust clinical service lines is critical. The chief executive officer of University Hospital reports to the Dean. The Dean establishes and implements the strategic goals of the School and works closely with department chairs and faculty to achieve the School‘s mission in alignment with that of the University. He is expected to strengthen the academic, clinical and research enterprises and work to maximize productivity in all areas. The Dean also leads recruitment for NJMS and retention strategies for NJMS‘s talented faculty, ensures the continued success of the research enterprise, develops shared programs with other UMDNJ Schools, and represent the School within the University, with other higher education institutions, local hospitals, public/private entities, and the community. At the time of his appointment the Dean reported to Dr. Denise V. Rodgers, Executive Vice President for Academic and Clinical Affairs, who assumed the role of Interim President for UMDNJ on January 1, 2012. The Dean must have an appropriate board certification in a recognized specialty and scholarly and professional accomplishments, which qualify for a professorship with tenure, and a national and/or international reputation in a medical sciences discipline. The Dean must have a demonstrated record of: exceptional leadership in a senior level academic position in a complex medical school environment including experience in development and management of clinical, translational, and/or basic science programs; budget and grants management; strategic planning experience; recruitment and retention of strong academic leaders, clinicians, physician-scientists and other researchers; experience in healthcare delivery systems and knowledge of relationships between university and community- based programs and practices; previous success in development and fundraising efforts; experience in the management of faculty practice plans; experience in working with health care and/or faculty associated labor unions; and excellent interpersonal, organizational and administrative skills. Once the decision was made to develop a master clinical services agreement with University Hospital employing the use of consultants, the University made the decision that the Dean would no longer has direct oversight of University Hospital. He continues to have the leadership teams from both NJMS and University Hospital meet on a weekly basis. b. Supply a chart showing the relationships among the members of the medical school and university administrations and the administrations of other schools and colleges, institutes, centers, etc. Include, if appropriate, information about the reporting relationships for the director(s) of any teaching hospitals owned or operated by the medical school or university and of the medical faculty practice plan. If the medical school is part of a for-profit/investor-owned company, the chart should describe the reporting Academic Year _2011-2012_ Page |25 relationship that the dean or other senior academic officers have with the board of directors or officers of the corporation. This information is provided at: http://www.umdnj.edu/oppmweb/university_policies/structure/index.htm The Dean of New Jersey Medical School attends the following regularly scheduled meetings with the President, as well as additional meetings that occur on an ad-hoc basis. 1- One-on-One Meeting with the President: Monthly 2- Meeting with the President and other UMDNJ Deans: Bi-monthly (every other week) 3- Meeting with the President and the University Hospital CEO: Monthly 4- President’s Executive Management Team Meeting: Monthly 5- Attendance at UMDNJ Board of Trustees Meeting: Monthly In addition, the Dean of New Jersey Medical School and the University President (Interim) communicate regularly by telephone at least two to three times per week. Also, the Dean has clear and open lines of communication with the University Vice President for Academic Affairs with regular interaction either by telephone or in person occurring on an ad hoc basis as issues arise. For matters related to the New Jersey Medical School medical education program, the authority and responsibility of the University (parent institution), the Dean of New Jersey Medical School, the Chairs of the New Jersey Medical School Academic Departments and their faculty, and University Hospital are described in the UMDNJ bylaws and the NJMS bylaws. According to the NJMS bylaws, the Committee on Curriculum, Academic Programs and Policies shall be the central integrated body of faculty, students and administrators charged with design, evaluation, revision, approval and oversight of the curriculum and overall educational program. The NJMS Bylaws can be found at the Faculty Organization link, http://njms.umdnj.edu/faculty_org/NJMSBylawsapprovedBOT3211.cfm, page 20:4.6.5. CAP2 shall make recommendations to the Dean and to the Faculty Council regarding implementation of these programs. The Dean or his/her designee, namely the Vice Dean (the position of Senior Associate Dean no longer exists), in concert with the Committee, will have responsibility for the overall leadership, management and implementation of the curriculum. Under the University of Medicine and Dentistry of New Jersey (UMDNJ) bylaws (http://www.umdnj.edu/acadweb/Bylw9-99.pdf) page 3, Section 2, the Dean: 2.1 Under the President and the Senior Vice President for Academic Affairs, the Dean shall be the chief academic and administrative officer of a school of UMDNJ with primary responsibility for implementing the mission of the school. The Dean's duties and powers shall include the following: 2.1.1 primary responsibility for the school's educational, research, health care and service programs, for the development of teaching and research affiliations, for administration of the school, for promotion of the school's development and effectiveness, and for maintaining accreditation with appropriate groups or agencies; 2.1.2 evaluation and final approval of curricula; Effective July 1, 2013, the Dean of NJMS will directly report to the Chancellor of the Rutgers Biomedical and Health Sciences, along with the deans of all the other schools of Rutgers Biomedical and Health Sciences. Academic Year _2011-2012_ Page |26 c. Describe any compensation or other arrangements (including, but not limited to, shareholder status) that the dean or other senior academic officers have which are dependent upon the financial success of the medical education program. Neither the Dean’s compensation nor that of any other senior academic officer is dependent upon the financial success of the medical education program. IS-10. The chief official of a medical education program must be qualified by education and experience to provide leadership in medical education, scholarly activity, and patient care. ___________________________________________________________________________________ Provide a brief resumé of the dean’s academic and administrative experience. Provide the dean’s full curriculum vitae. Academic Year _2011-2012_ Page |27 (See Appendix 8) Robert L. Johnson, MD, FAAP THE SHARON AND JOSEPH L. MUSCARELLE ENDOWED DEAN Robert L. Johnson, MD, FAAP received his M.D. from the College of Medicine & Dentistry of New Jersey in Newark, N.J. and completed a research fellowship in Adolescent Medicine at New York University Medical Center – Bellevue. Dr. Johnson is the Sharon and Joseph L. Muscarelle Endowed Dean, Professor in the Department of Pediatrics and the former Chair; holds a secondary appointment as Professor of Psychiatry and continues to serve as the Director for the Division of Adolescent and Young Adult Medicine at the New Jersey Medical School of the University of Medicine and Dentistry of New Jersey. Dr. Johnson has become a well-recognized spokesperson for adolescent issues. He annually addresses many local, state, national and international audiences and frequently appears on television and radio. He has published widely, and he conducts an active schedule of teaching, research and clinical practice at the New Jersey Medical School. Dr. Johnson’s books include: The Race Trap: Smart Strategies for Effective Racial Communication in Business and in Life, which addresses the pitfalls commonly encountered in communications across the racial divide and Strength for Their Journey: 5 Essential Disciplines African American Parents Must Teach their Children and Teens, a guide for parents of African American teens. Over his academic career, he has received numerous honors and awards. Dr. Johnson has served in numerous capacities at national, regional and state levels. These include: Chair, Newark Ryan White Planning Council; Chair, Male Involvement Advisory Committee, Department of Health & Human Services, Region II; Member of the Division of Behavioral and Social Science and Education National Advisory Board, National Research Council-National Academy of Sciences; Member of Task Force on Community Preventive and Centers for Disease Control and Prevention. Dr. Johnson has served as the Principal Investigator on numerous federal, private and state grants for over 30 years, dedicating his work towards the development of outreach programs to enhance services addressing Adolescent and Young Adult physical and mental health, Sexuality and Sexually Transmitted Infections, Violence, Delinquency, and Substance Abuse. His research programs have received funding awards from a wide-range of sponsorships including the Robert Wood Johnson Foundation, Johnson & Johnson Community Health Care Program, National Institutes of Health and New Jersey Department of Health. Since 1997, Dr. Johnson has been awarded over $52 million dollars of grant funding. His dedication towards clinical outreach programs has addressed health issues affecting minority adolescents and their family members in the Newark Community and beyond. He has pioneered programs such as Peer Outreach Workers Educating Risk-Takers (POWER) with a goal towards the education, promotion, and demonstration of strategic planning for healthy behaviors among teens (13-19) who are at risk for contracting and transmitting sexually transmitted infections, such as HIV. This program has provided modernized and culturally appropriate services and materials through prevention education. Another notable achievement in clinical outreach established by Dr. Johnson is the S.T.A.R.T. (Screening, treatment and Risk Reduction for Teens) Program. As part of the Division of Adolescent and Young Adult Medicine (DAYAM), this program focuses on the treatment of HIV positive adolescents and young adults. Other valuable outreach efforts have included the EMS Youth Trauma Initiative, The Young Fathers Program, and the Youth Violence Prevention Project, all funded by both State and private funding agencies. In addition, he has been instrumental in raising funds that support the infrastructure at New Jersey Medical School, serving as Principal Investigator on two NIH-funded construction grants. Through his efforts, NJMS was awarded a $14.9 million grant to modernize the NJMS Central Research Animal Facility. Academic Year _2011-2012_ Page |28 IS-11. The administration of an institution that offers a medical education program should include such associate or assistant deans, department chairs, leaders of other organizational units, and staff as are necessary to accomplish its mission(s). There should not be excessive turnover or long-standing vacancies in the leadership of the institution. Areas that commonly require administrative support include admissions, student affairs, academic affairs, educational affairs/curriculum, faculty affairs, graduate education, continuing education, relationships with clinical affiliates, research, business and planning, and fund-raising. ___________________________________________________________________________________ a. Attach a chart showing the organizational structure of the dean’s office. b. List the percent of effort contributed by each associate and assistant dean to the administrative support of the medical school and, for each, indicate his or her date of appointment to the administrative position. Indicate if any associate/assistant dean position is being filled on an interim basis. If there are interim appointments for positions in the dean’s office, describe the status of recruitment to fill the positions on a permanent basis. Maria L. Soto-Greene, M.D., Vice Dean (Academic and Diversity Affairs), - 84% (09-2005), Academic Year _2011-2012_ Page |29 includes diversity related activities; formerly Chief of Staff (2004-2005) and Senior Associate Dean for Education (2001-2004) David Alland, M.D. Assistant Dean for Clinical Research - 9% (7-2008) Suzanne Atkin, M.D., Associate Dean for Clinical Affairs, University Hospital - 85% (1-2005) Stephen R. Baker, M.D., Associate Dean for Graduate Medical Education – 35% (6-2001) Melissa Davidson, M.D., Assistant Dean for Graduate Medical Education – 40% (3-2007) Richard Feinberg, PhD, Assistant Dean for Basic Science Education and Faculty Development – 100% (12-2010); formerly the Assistant Dean for Educational Resources and Faculty Development – 100%. Sangetta Lamba, MD, Associate Dean for Education – 90% (2012) Steve Keller. PhD, Director (Interim) of Educational Evaluation and Research - 20% (July 2012), Previous individual left in July 2012. Julie Ferguson, M.P.A., Assistant Dean for Student Affairs/Director, Registrar’s Office – 100% (12-2003) William C. Gause, Ph.D., Senior Associate Dean for Research - 57% (1-2004) Christine M. Gerula, M.D., Assistant Dean for Careers in Medicine – 20% (6/2009) James M. Hill, Ph.D., Associate Dean for Student Affairs100% (8-2010), previously served in an interim capacity from (5/2009-7/2010), prior to this, he was Assistant Dean for Academic Development and Student Affairs George Heinrich, MD, Associate Dean for Admissions –100% (7-2004) Deborah Lazzarino, Ph.D., Assistant Dean for Research Administration – 93% (1-2011) Carol Newlon, PhD, Associate Dean for Faculty Affairs – 35% (7-2011) David L. Roe, M.B.A., Associate Dean and Chief Financial Officer – 100% (6-2002) Gregory J. Rokosz, D.O., J.D., FACEP, Associate Dean for Education at Saint Barnabas Medical Center – 5% (9-08) Joshua Rosenblatt, M.D., Associate Dean for Education at Newark Beth Israel Medical Center – 5% (7-08) Kendell R. Sprott, M.D., J.D., Senior Associate Dean for Clinical Affairs – 55% (6-2008) Andrew Thomas, PhD, Senior Associate Dean, Graduate School of Biomedical Sciences 30% (42009) c. Indicate the term of appointment for department chairs and the number of times that the appointment can be renewed. According to the NJMS bylaws, Section 2, pages 4-5 – Departmental Chairs (http://njms.umdnj.edu/faculty_org/NJMSBylawsapproved-BOT3211.cfm), at least once every five (5) years or at any time during the term of a departmental chair, a review and evaluation of the department and of the stewardship of the chair may be initiated by the Dean. The Dean may also initiate such a review under the following circumstances: if requested by the Faculty Council, or upon petition by over 50% of the departmental faculty of full academic rank. A review of the stewardship of each chair shall, in any event, occur at least ninety days prior to the expiration of the chair's term. A Committee for review shall be appointed by the Dean with the approval of the Faculty Council, and the committee will contain no member of the department concerned. The committee shall take steps to ensure that the faculty and other appropriate constituencies have opportunity for input to the review and evaluation. At the conclusion of the review process, which ordinarily should not exceed sixty days, the recommendations of the review committee are to be submitted to the Dean and through the Dean to the chair and to the members of the department. Departmental members of full academic rank, upon receipt of the report, will meet [within approximately ten (10) working days] and shall, by secret ballot, vote to accept or reject the report and forward the results and recommendations to the Dean. The Dean may reappoint a departmental chair after formal consultation with the department, or may declare the chair vacant. However, chairs serve at the pleasure of the Dean without regard to term or review. In the case of a vacancy, the Dean may appoint an acting (or interim) chair after formal consultation with the members of the department. The interim chair shall serve at the will and pleasure of the Dean. Academic Year _2011-2012_ Page |30 c. Indicate the date of appointment for each currently sitting department chair. Departments with Permanent Chairs NAME DATE Anesthesiology 5/2012 Biochemistry & Molecular Biology 6/1996 Cell Biology & Molecular Medicine 11/2012 Internal Medicine 3/2012 Microbiology & Molecular Genetics 6/2004 Neurosurgery 1/2012 Obstetrics, Gynecology & Women’s Health 11/1985 Ophthalmology & Visual Sciences 1/1994 Orthopaedics 7/2009 Otolaryngology Head and Neck Surgery 10/2012 Pharmacology & Physiology 9/1997 Preventive Medicine & Community Health 1/2001 Radiation Oncology 11/2008 Radiology 11/1990 e. List the departments that are currently without a permanent chair and the date on which the last permanent chair left office. Describe the status and timelines of recruitments to fill vacant chair positions. Departments without Permanent Chairs NAME *Emergency Medicine DATE 3/2008 Search will be relaunched Family Medicine 8/2011 Neurology and Neurosciences 6/2011 Search underway Pathology and Laboratory Medicine 1/2012 Pediatrics 1/2006 Search Concluded Psychiatry 4/2008 (Permanent Chair March 2013) Physical Medicine & Rehabilitation 6/2012 Search on-going Surgery 7/2011 Search underway *Emergency medicine was established as a new department in 2008. The chair serves as the academic chair with a chief of service designated by University Hospital that addresses the dayto-day clinical operations. On two separate occasions, the search committee presented a finalist (2010 and 2011) and an offer was made. Ultimately, one candidate decided to stay with the institution and the other accepted another position. A new search is planned for the summer of 2013. f. Briefly describe how, how often, and by whom the performance of chairs is reviewed. Under the NJMS Bylaws (Article II, Title B, Section 2), the Dean evaluates the department chairs on annual basis. Additionally, a five-year stewardship review is required g. Briefly describe the budgetary authority of department chairs and the sources of funding for departmental budgets. Academic Year _2011-2012_ Page |31 Under a mission-based funding model implemented at NJMS in 2003, academic department chairs have a great responsibility and authority with respect to managing their School allocations. They have a large measure of control over the number of faculty and administrators and they can re-allocate from salary to non-salary or from non-salary to salary upon request. At the same time that NJMS designed and implemented a mission-based funding model, the School ended "use-it-or-lose-it" budgeting at NJMS: once the model determines the allocation to each department, each academic department will retain unspent allocation across fiscal year lines. In addition, under-spending will not trigger a reduction in the allocation in subsequent year(s): the mission-based funding model is driven by measures of output, not measures of expense. The funds that the School allocates to Departments via the mission-based funding model are specifically for School-related effort: the metrics that drive the model’s output are dominated by quantity of funded research; the quantity and quality of the department’s undergraduate medical school teaching program; and service on School committees. The model’s funds are derived from State appropriation, tuition and fees, indirect cost recovery on grants, taxes on the faculty practice, and other revenues including overhead fees on residency and other affiliate relationships. Separate from the School’s mission-based funding formula, the School provides program-specific funds related, for instance, to department chair and other faculty recruitments. The School also distributes a fraction of the indirect cost recovery, by formula, to the academic departments as well as a fraction of the overhead monies derived from the School’s residency programs. Also separate from the School’s funding described above are the funds allocated by University Hospital for clinicians’ salary support. UH allocates a fixed annual sum and the School distributes those funds to the academic departments in support of clinicians’ salaries. In addition to the School and University Hospital funding outlined above, academic departments derive important additional funds from a number of sources, including the directs on sponsored program funding (grants), physician earnings on practice billings and collections, and medical service agreements with other institutions. See also Part A, item (a.) in this section of the database. Academic Year _2011-2012_ Page |32 IS-12. Medical students should have opportunities to learn in academic environments that permit interaction with students enrolled in other health professions, graduate, and professional degree programs and in clinical environments that provide opportunities for interaction with physicians in graduate medical education and continuing medical education programs. These academic, graduate medical education, and continuing medical education programs should contribute to the learning environment of the medical education program. Periodic and formal review of these programs culminating in their accreditation by the appropriate accrediting bodies would provide evidence of their adherence to high standards of quality in education, research, and scholarship. Whenever appropriate, medical students would be able to participate in selected activities associated with these programs in order to facilitate achievement of their personal and professional goals. ___________________________________________________________________________________ Graduate Education a. Indicate the number of students enrolled in Master’s and doctoral programs taught by medical school faculty. Include degree programs in the biomedical sciences and other programs (e.g., biomedical engineering, public health) that are taught by medical school faculty. Newark Campus of the UMDNJ- Graduate School of Biomedical Sciences (GSBS) GSBS has three divisions, one associated with each medical school campus of UMDNJ. Each of the Divisions functions autonomously with its own Executive Council and independent budget. The Newark Division of GSBS is overseen by the Senior Associate Dean for GSBS at NJMS, who reports to the GSBS Dean for academic matters, but also works with the Dean of NJMS on operational and shared resource issues. There is also a Senior Associate Dean for GSBS at NJDS, but all of the Newark GSBS programs are run through the GSBS at NJMS office. The Newark campus of GSBS is in the process of migrating from basic science department-based PhD programs to a smaller number of more broadly based interdisciplinary PhD programs. The latter are designed to increase the involvement of clinical research faculty and facilitate collaborative and translational training opportunities. Because students only started to matriculate into the interdisciplinary programs in the fall of 2011, there are still a significant number of students in the department-based programs. However, with the exception of Biomedical Engineering, these programs have ceased admitting new students and their enrollments will decrease as the enrollment in the interdisciplinary programs increases. Approximately 30 new PhD students matriculate into GSBS-Newark each year. In addition to the PhD programs, GSBS-Newark offers the thesis-based Master of Science and the non-thesis Master of Biomedical Sciences degrees, as well as some graduate certificate programs. There are also a number of dual degrees, the most prominent of which is the MD/PhD, which is described in more detail in IS-14. The MD/PhD program provides one of the most important pathways through which medical students become involved in the institution's research mission and exposed to GSBS students. However, there is also a robust summer research program for medical students and a new MD with Thesis program that provides a year-long research internship. GSBS does not appoint its own primary faculty other then faculty administrators. More than 90% of the graduate faculty members on the Newark campus have their primary appointments in NJMS departments or centers of NJMS and the remainder are in the dental school. Graduate student teaching is a normal expectation of medical school faculty and the number of courses and teaching hours do not interfere with the assigned educational activities in the medical school. Moreover, the efforts of graduate students in faculty laboratories represent an important part of the research enterprise of the medical school. Academic Year _2011-2012_ Page |33 Below is the GSBS enrollment data for the Spring 2012 semester. Please note the exact numbers fluctuate because the PhD and MS students graduate throughout the academic year. Program Departmental Programs Biochemistry & Mol Biology Cell Biol. & Molec. Medicine Pathology and Exper. Immunol. Microbiology & Molec genetics Pharmacology & Physiology Oral Biology Neuroscience Biomedical Engineering Interdisciplinary Programs Biomedical Sciences (Interdisciplinary) Molecular Biology, Genetics & Cancer Cell. Biol., Neuroscience & Physiology Infection, Immiunity & Inflamation Master of Biomedical Sciences Master of Science Certificate-Pharmacological Sciences Certificate- Stem Cell Biology MD/PhD (with NJMS) Total students enrolled Master’s Students Certificate Students Doctoral Students 14 14 15 16 22 8 11 14 1 34 9 7 8 273 85 4 359 4 22 194 Newark Campus of the UMDNJ-School of Public Health (SPH) The Newark Campus of the UMDNJ-SPH offers the MPH degree in the areas of Dental Public Health, Quantitative Methods (Biostatistics and Epidemiology), and Urban Health Administration. Many of the students pursue dual degrees in collaboration with faculty from UMDNJ's New Jersey Medical School (NJMS), New Jersey Dental School (NJDS), Graduate School of Biomedical Sciences (GSBS), and School of Nursing (SN) as well as Rutgers University's College of Nursing. Students pursuing doctoral degrees (both PhD and DrPH) in Epidemiology are mentored by Newark Campus SPH faculty. In addition to degree programs, the Newark campus offers certificate programs in Clinical Epidemiology, General Public Health and Public Policy and Oral Health Services Administration. The majority of the faculty including the Chair at the SPH-Newark Campus Department of Quantitative Methods have their primary appointments at NJMS as well as the Associate Dean of the Newark Campus, who is also the Chair of the Department of Preventive Medicine and Community Health at NJMS. The MD/MPH dual degree program allows students who are attending NJMS to complete an MPH degree while they are enrolled in medical school, taking an extra year of training (for the MPH) usually between their second and third year. Most SPH classes are offered in the evening on the UMDNJ-SPH Newark campus during summer, fall and spring semesters. NJMS students who are not formally enrolled in the dual degree program are also welcome to register for courses as a visiting student. NJMS faculty and staff are encouraged to pursue degrees, an SPH certificate or to register for specific courses of interest on the Newark Campus of the SPH. Academic Year _2011-2012_ Page |34 SPH enrollment data for the 2010-2011 Academic Year, broken down by semester: Program # Students # Students # Students Total for Fall 2011 Spring 2012 Summer 2012 AY 2012 Certificate and Non28 26 15 69 matriculated Students MPH only 62 83 43 188 MS/MPH (with GSBS) 7 7 4 18 MD/MPH (with NJMS) 9 11 2 22 PhD 6 6 0 12 DrPH 1 2 1 4 113 135 65 Total enrolled 233 b. Are there university or medical school policies that require regular review of graduate education (Master’s, doctoral) programs? If so, include a copy of the policy or related documents in the Appendix. The UMDNJ-Graduate School of Biomedical Sciences Academic Program Review which delineates the process for review of the program is discussed under c. can be found in the (See IS Appendix 9). The UMDNJ- School of Public Health is accredited by the Council on Education for Public Health (http://www.ceph.org/pg_about.htm). Both UMDNJ GSBS and SPH are also reviewed as part of the UMDNJ Middle States Accreditation. c. Describe the process used for review of doctoral programs in the biomedical sciences. During the last survey, we received a citation because of “the absence of regular internal or external reviews of the graduate programs in the Graduate School of Biomedical Sciences (GSBS) prevents validated assurance that those programs maintain consistent high standards of educational quality”. In order to address this citation, and to meet the need for rigorous external program evaluation on a regular basis, GSBS initiated a periodic program of Academic Program Review using a self-study mechanism and external experts. The reviews are conducted separately for each campus on a rotating basis, allowing for a new review of each GSBS division every 6 years. GSBS at NJMS was reviewed in 2007, with an overall positive outcome. A copy of the summary report and cover letter from the external reviewers can be found in (See IS Appendix 10). This external review of the GSBS programs was communicated to LCME with a follow up letter from the LCME accepting our process. The following is excerpted from the GSBS Academic Program Review policy, which is attached in its entirety in the (See IS Appendix 9): The major purpose of Graduate Program Review at the UMDNJ-Graduate School of Biomedical Sciences (GSBS) is to ensure that programs are functioning at the highest possible levels of academic quality and are operating in ways that are consistent with the missions of the University and the GSBS. The process of Graduate Program Review serves as a means to inform faculty, administrators, students, and University governance bodies with respect to the relative merits and areas of needed improvement in particular programs. In this sense, Graduate Program Review is a tool for critical reflection and change. Graduate Program Reviews involve a process of self-study complemented by a site visit and critique by external experts. The review process is grounded in both university-wide standards and criteria specific to discipline-based and interdisciplinary programs. Upon acceptance of the self-study by the Dean of the Graduate School, an external review panel is organized. The panel consists of three members, all external to GSBS, at least two of whom are senior faculty members Academic Year _2011-2012_ Page |35 from other universities with recognized expertise in graduate education. The external review panel meets initially with the Dean and Senior Associate Dean of the GSBS division to discuss the self-study and orient the panel to the program. They then meet separately with program directors and key faculty representatives from each program. The review panel also meets with graduate students (as a group with representatives from each program). At the conclusion of the two day visit, the panel submits an interim report during a meeting of the Dean, Senior Associate Dean, Program Directors, Chairs and Student Representatives. The final report (due within two weeks of completion of the site visit) is subsequently sent to the Dean and the Executive Vice President for Academic and Clinical Affairs, together with an action plan for any changes recommended. The UMDNJ- School of Public Health is accredited as a graduate school of public health by the Council on Education for Public Health (CEPH). The last review by CEPH in 2007 resulted in an accreditation term of 7 years. The Council on Education for Public Health (CEPH) is an independent agency recognized by the US Department of Education to accredit schools of public health and public health programs offered in settings other than schools of public health. These schools and programs prepare students for entry into careers in public health. The primary professional degree is the Master of Public Health (MPH) but other master's and doctoral degrees are offered as well. The Council is a private, nonprofit corporation with APHA and ASPH as its two corporate members. The affairs of the corporation are directed by a 10-member board. As an independent body, the board is solely responsible for adopting criteria by which schools and programs are evaluated, for establishing policies and procedures, for making accreditation decisions, and for managing the business of the corporation. Source: http://www.ceph.org/pg_about.htm Graduate Medical Education a. For each clinical facility at which one or more medical students take a required core clerkship rotation (except ambulatory, community-based sites), mark a “+” if residents in an ACGME-accredited program (for U.S. medical schools) or in an RCPSC or CFPC-accredited program (for Canadian medical schools) are involved in medical student education in that clerkship rotation at that site; place a “–” for any clerkship rotation offered at that site in which there are no residents. Clinical Facility Name UMDNJ University Hospital Hackensack University Medical Center St. Barnabas Medical Center Newark Beth Israel Medical Center Veterans Administration Health Care System Mountainside Hospital UMDNJBehavioral Healthcare Family Medicine * Internal Medicine + Obstetrics/ Gynecology + Pediatrics + + + + + + + + + + + + + Psychiatry/ Neurology + Surgery + (Psychiatry) + + + + + + Academic Year _2011-2012_ Page |36 Greystone Park + Psychiatric (Psychiatry) Hospital Medical Center Bergen + Regional (no longer a Medical Center teaching site) Morristown + Hospital * Students learn family medicine in family medicine preceptor ambulatory sites. These preceptors have been long term volunteer faculty who are experienced in clerkship education. b. If the medical curriculum does not include a separate required clerkship rotation in one or more of the above disciplines (e.g., when the curriculum includes an integrated experience for some medical students), describe these students’ interactions with residents, including the residents’ specialties and the settings in which these interactions occur. The Psychiatry/Neurology Clerkship is administered by both departments which have residents in each discipline. Students spend 4 weeks in psychiatry and 4 weeks in neurology, which includes neurosurgery. There is only one final grade issued for this clerkship. c. Provide the number of residents who are the responsibility of the medical school’s faculty, by training program, including those programs at affiliated hospitals at which residents are taught by medical school faculty. (Note: If the medical school operates geographically separate clinical instructional sites/campuses, provide a separate table for each site.) PGY-1 Specialty of Training Program Anesthesiology Diagnostic Radiology Emergency Medicine Internal Medicine Allergy/Immunology Cardiology Dermatology Endocrinology Gastroenterology Geriatrics Hepatology Infectious Disease Interventional Cardiology Nephrology Pulmonary Critical Care Medicine – Pediatrics Neurology Child Neurology Vascular Neurology Neuromuscular Medicine 6 41 Total Residents # Clinical Fellows (In ACGMEApproved Program) #Clinical Fellows (In NonACGME Accredited Programs) 27 18 24 110 3 10 6 2 9 2 3 6 2 6 9 4 4 15 16 3 1 1 Academic Year _2011-2012_ Neurosurgery Neuroendovascular Neuroradiology Obstetrics and Gynecology (OB/GYN) OB/GYN-Maternal Fetal Medicine OB/GYN-Reproductive Endocrinology & Infertility Ophthamology Orthopedics Orthopedics Hand Surgery Orthopedics Musculoskeletal Oncology Orthopedics Trauma and Reconstructive Surgery Otolaryngology Pathology Pediatrics Pediatrics Infectious Disease Pediatrics Medical Genetics Physical Medicine and Rehabilitation (PMR) PM&R-Musculoskeletal Medicine PM&R-Pediatric PM&R-Spinal Cord Injury Preventive Medicine Psychiatry Child Psychiatry Surgery Plastic Surgery Surgical Critical Care-Trauma Urology TOTAL Page |37 2 13 3 6 24 1 3 6 15 29 1 1 1 1 2 4 15 10 13 48 1 1 28 3 1 1 9 18 2 29 4 63 4 2 118 8 509 63 10 NOTE: The table (above) includes housestaff engaged in research or other activities outside of the usual clinical training programs, resulting in higher totals than reported on the LSSR. d. Describe the mechanism(s) used for oversight and coordination of graduate medical education, including the evaluation and allocation of training positions. Note any programs currently on probation, as well as any programs whose size is being substantially expanded or reduced. The UMDNJ-New Jersey Medical School ensures that its ACGME-accredited medical education programs are in substantial compliance with the relevant Program Requirements in the following ways: Every ACGME-accredited program goes through an Internal Review (aka Mid-Cycle Review) at the midpoint of the accreditation cycle in which the program is reviewed according to the ACGME Institutional and Program Requirements. The process includes the program’s completion of the ACGME Program Information Form (PIF) as if it were undergoing a formal ACGME site visit. Following review of the PIF and all supporting documents, the Internal Review Committee conducts separate interviews with representative residents from each level of training; with representative faculty including hospital site director; and with the Program Director (PD) and department chair. A report is generated and reviewed at Academic Year _2011-2012_ Page |38 the GMEC. If the Internal Review Committee finds that a program is NOT in substantial compliance with a particular program requirement or the institutional requirements, the Program Director is instructed to correct the deficiency with the support of the Graduate Medical Education Committee (GMEC). Follow-up of corrective actions is determined by the GMEC and is dependent upon the nature and severity of the deficiencies. Support is provided to the PD by the Designated Institutional Official (DIO) and the Associate Dean for GME (ADGME) in the correction of deficiencies. If necessary, a follow-up focused Internal Review is done by the original Internal Review Committee and again a report is written and presented to the GMEC. Each and every time an ACGME-accredited program completes a Program Information Form (PIF) for submission to the ACGME for an upcoming site visit, the DIO and ADGME review the completed PIF and attachments BEFORE it is sent to the ACGME. The PIF is reviewed for completeness, accuracy, and compliance with the requirements. Dr. Stephen Baker, Associate Dean for Graduate Medical Education and DIO, reviews each ACGME accreditation letter and/or report for each of the ACGME accredited programs as soon as it is received. Dr. Baker meets with the PD in a timely fashion if any citations or concerns are stated in the letter. They discuss and develop a plan to address and correct any deficiencies. The GMEC reviews and discusses each ACGME accreditation letter and determines the plan for followup of corrective actions. The GMEC meets monthly. An annual GME program report is prepared by the Associate Dean for Graduate Medical Education (Designated Institutional Official) and is presented at the University Hospital Medical Staff Executive Committee. This report is distributed to all major participating affiliate training sites. Individual program size is based on the capacity of each program to offer an educational experience for each resident that is consistent with both New Jersey Medical School and accreditation standards. Program directors seeking to increase their total program complement must submit a request to the Associate Dean for Graduate Medical Education that outlines a sound educational rationale and funding source. The request is evaluated by the Associate Dean for Graduate Medical Education and is presented for final approval by the Graduate Medical Education Committee. If a new position is approved and exceeds the maximum program complement established by the accrediting agency (i.e. ACGME) the program submits request for approval to the accrediting agency prior to recruiting for the position. All GME programs are currently accredited. There are no programs on probation. New Jersey Medical School’s sponsorship of the Family Medicine program was transferred to Hoboken University Medical Center in May 2010. NJMS had sponsored this program for over a decade. This program was based at Hoboken and its outpatient center with clinical rotations to other facilities within NJMS. The outstanding receivable was substantial (multimillion dollars) and the financial viability of the hospital was in question (the hospital did in fact declare bankruptcy several months later and was purchased by another hospital system). NJMS leadership, which included the DIO, Dean, Vice Dean, CFO, and Director of Clinical Academic Operations, determined that allowing the residency positions to remain in the match would commit NJMS to a program whose primary site (Hoboken) was in financial jeopardy, leaving NJMS financially, administratively and programmatically vulnerable, which in turn could affect all of the other GME programs. The decision was therefore made to withdraw from the match with the intent to close the program. The DIO maintained communication with the NRMP throughout this process. In May 2010, final steps were taken to transfer sponsorship from NJMS to Hoboken, which included DIO discussions with the ACGME who recommended this transfer in lieu of program termination. Final transfer was accomplished effective July 1, 2010. e. For each accredited institution, provide the following information regarding ACGME/RCPSC/CFPC institutional review of graduate medical education programs sponsored by the medical school or its major teaching hospital(s): Academic Year _2011-2012_ Page |39 Date of Last ACGME/RCPSC/CFPC Institutional Review May 8, 2012 Status Date of Next Review Accredited October 1, 2015 Continuing Medical Education a. If the medical school or its clinical affiliates are accredited by the ACCME/RCPSC to sponsor continuing medical education for physicians, indicate each sponsoring organization’s current accreditation status, the length of accreditation granted, and the year of the next accreditation review. Program Sponsor UMDNJ-Center for Continuing and Outreach Education Length of Accreditation Term Accreditation Status ACCME: Accreditation with Commendation Six years Year of Next Review 2016 b. Describe the opportunities available to medical students for participation in continuing medical education programs. Is student participation in any continuing medical education programs expected or required? Medical students are permitted and expected to attend regularly scheduled series during their clerkship rotations, as well as any continuing education seminar/conference sponsored by an individual department. New Jersey Medical School in conjunction with the Center for Continuing and Outreach Education (CCOE) sponsors the following regularly scheduled series: Advances in Pediatrics Grand Rounds Allergy & Immunology Grand Rounds Anesthesiology Grand Rounds Cardiac Catheterization Clinical Conference Emergency Medicine Grand Rounds & Journal Club Head & Neck Tumor Conference Infectious Disease Case Conference Medical Clinical Pathology Case Conference Medicine Grand Rounds Medicine, Morbidity & Mortality Conference Neurology Chief of Staff Grand Rounds Neurology Grand Rounds OB/GYN Grand Rounds Ophthalmology Grand Rounds Oral & Maxillofacial Surgery Seminar Series Otolaryngology Grand Rounds Plastic Surgery Academic Conference Preventive Medicine & Public Health Grand Rounds Psychiatry Grand Rounds & Case Conferences Surgical Grand Rounds Trauma Grand Rounds Tuberculosis Grand Rounds Urology Grand Rounds Several NJMS departments also collaborate with CCOE to develop half, full, or multi-day continuing education activities that take place both on and off campus, as well as print or web-based enduring materials. These departments include Otolaryngology, Radiology, Neurosurgery, Urology, and Preventive Medicine and Community Health. c. Number of Weekly Offerings. NJMS, in conjunction with CCOE, currently sponsors 23 regularly scheduled series that are certified for AMA PRA Category 1 Credit™. Nineteen are held on a weekly basis, with the remainder occurring monthly, semimonthly, or bimonthly. See also Part A, items (b.) and (c.) in this section of the database. Academic Year _2011-2012_ Page |40 IS-13. A medical education program must be conducted in an environment that fosters the intellectual challenge and spirit of inquiry appropriate to a community of scholars. IS-14. An institution that offers a medical education program should make available sufficient opportunities for medical students to participate in research and other scholarly activities of its faculty and encourage and support medical student participation. The institution is expected to provide an appropriate number and variety of research opportunities to accommodate those medical students desiring to participate. To encourage medical student participation, the institution could, for example, provide information about available opportunities, offer elective credit for research, hold research days, or include research as a required part of the curriculum. Support for medical student participation could include offering or providing information about financial support for student research (e.g., stipends). New Jersey Medical School (NJMS) is dedicated to making significant contributions to the body of biomedical knowledge and serves as a leading research and teaching institution. The mission is to enhance and strengthen research support services for the NJMS scientific community. The goals are to build strong resources for research with a particular emphasis on building translational research programs. Our research enterprise has successfully supported a wide range of sponsored programs, including federal, state and private grant funded research. The Office of Research and Sponsored Programs (ORSP) provides an infrastructure to facilitate research and research related activities for faculty, administration, students and staff at NJMS. ORSP provides investigators with administrative support for intra- and extramural research grant funding and contracts. In addition to individual investigator grant initiatives, faculty receive financial and administrative support to develop multi-investigator training, instrumentation, and center and program project grants, including inter-departmental research teams crossing basic and clinical research programs. To enable the research enterprise, the office works with Legal Management and various biomedical compliance offices to meet federal, state and university policies on all research grants and contracts. ORSP continually provides information to NJMS faculty on new funding initiatives and regulatory policies that could potentially impact their research programs. It is also dedicated to providing mentoring and training opportunities for research faculty, students and administrative staff in support of their research and scholarly endeavors, which includes a formal mentoring program for junior faculty and postdoctoral students. In addition, ORSP has developed a MD with Thesis Program that offers a unique opportunity for NJMS students to conduct original research during their medical school training. To provide continual scholarly interchange, ORSP sponsors and organizes research symposia at the local and national levels. Scholarly achievements are publicized through website postings, newsletters, and news publications. To help sustain the research and training programs, ORSP provides cutting edge research equipment and expertise by supporting research core facilities, as well as aggressively pursuing funding opportunities for new facility construction and the acquisition of shared instrumentation allowing us to stay current with expanding research technologies. For example, we were awarded a $14.9M NIH ARRA construction grant to renovate and build a state of the art animal research facility. This includes the infrastructure for a live animal imaging facility that will support preclinical translational studies. Over the last several years we have also been successful in obtaining a number of NIH Shared Instrumentation Grants, with the equipment housed in our Core facilities. This is an indication of both the high quality of the NIH funded investigators and the Core Facility administrative expertise. NJMS also provides bridge and seed grant programs, partly funded by the Dean’s office, to support both individual and multi-investigator initiatives. These monies, while modest, have been deemed important in assisting research projects that are able to compete for NIH and other outside funding. Academic Year _2011-2012_ Page |41 NJMS investigators have brought in more than $150M in NIH funding, representing an unprecedented growth in our research enterprise. Our research funding encompasses important areas of clinical therapeutic need, such as cardiovascular, infectious, inflammatory, neurological, ophthalmologic diseases and cancer. Many faculty at NJMS are leaders in their field and have published in high impact journals such as the New England Journal of Medicine, Cell and Nature Medicine. The Research Office supports current and new research programs through continued support of the core facilities and participates in the recruitment of new research faculty to improve and expand on our areas of educational, scientific, and medical expertise. Over the last several years, we have invested in additional administrative and infrastructure support that our clinical departments need to build their research enterprise. To address those needs we developed core facility resources and a strategic planning initiative to enhance the support for both young clinical researchers as well as more senior research faculty. For example, we have invested in building a Center for Clinical and Translational Science that lends support to clinical researchers at both an administrative and operational level, from protocol writing, budget and grant proposal development through the patient care record management and regulatory requirements in running clinical trials. This center includes a fully operational Clinical Research Unit as well as an Office of Clinical and Research Administration. In addition, we have developed a core facility service that supports grant management at the departmental level, with both pre award development and post award monitoring, to address the specific needs of clinical departments whose administrators have limited grant experience. Future areas of improvement identified during our strategic planning process included: developing more platforms for information exchange across departments and between clinician and scientists; identifying additional translational research areas for development; building stronger clinical outcomes and implementation research; and enhancing IT support for patient databases to be used in research studies. We have also enhanced our support of several interdepartmental centers that include faculty from both basic and clinical departments. These centers focus on specific research areas of excellence at NJMS and bring together both basic science and clinical researchers in a structured program emphasizing translational research. Finally, it should be noted that the Finance Office distributes department funding using a mission-based model, which factors in research activity and the faculty have access to a research extramural incentive program which provides additional salary support up to a maximum of $15,000 if $30,000 of the investigator’s salary is on a grant. a. If not already described in the response to standard IS-1, briefly summarize institutional goals and priorities relating to research and scholarship. The strategic plan approved on November 13, 2012 by faculty council sets forth the following goal for research: The rational reads as follows: ‘It is through advances in biology that patient care, treatment outcomes and quality of life are improved in our community. Advances are made through research excellence in focused areas of biomedical research. The keys to discovery require multi-disciplinary experimental projects that benefit from the expertise of scientists and clinicians with different expertise and knowledge base. Collaborative biomedical research increases the success for intellectual property development, extramural grant support, reputation of the medical expertise for innovation and excellence in ‘state of the art’ medical education and care. By developing the Institute of Urban Health and Research, it will provide the structural framework and the bridging for the integration of the efforts of our physicians and scientists to improve the quality of life in our community.” Academic Year _2011-2012_ Page |42 Strategic Goal #2: Build on our prominence in biomedical research that promotes innovative, clinical, population-based and translational research programs. Select Supporting Strategies 1. Build on our current strengths to incentive collaborative innovation and interdisciplinary research. 2. Improve research infrastructure and increase investment to further strengthen the institutional biomedical research enterprise and enhance collaborative efforts with biotech and pharmaceutical industries. 3. Establish an Institute of Urban Health and Research focusing on patient-centered outcomes, comparative effectiveness, health services and translational research in diseases and injuries affecting urban populations. 4. Foster collaboration both within the University and with external partners; within the university, provide financial support for physician-scientists development 5. Invest in Information Technology and physical infrastructure on the Newark campus to provide an environment conducive to innovative and productive collaborations. 6. Improve funding for research by expanding the scope and responsibilities of the Center for Clinical and Translational Sciences (CTS) to (1) increasing industry partnerships and (2) increasing relationships with CROs. Measures of Success: Increase publications in high impact journals, increase NIH funding, expanded research contracts with industry and new intellectual property development. Recognition of the NJMS Institute of Urban Health and Research as a state-wide resource for expertise in the areas of patient-centered outcomes, comparative effectiveness, health services delivery and translational research. Increased inter-departmental and inter-school research collaborations resulting in an increase in the number of multi-investigator/multi-site grant awards. Improved information technology resources available for the use of investigators in analyzing, managing and sharing research data. Improved human resources and physical infrastructure in areas where research is conducted. An expanded CTS resulting in increased industry partnerships and relationships with CROs. b. Briefly describe the opportunities available for medical student participation in research, including the time periods when students may do so, the average number of students in the base year who were involved in each type of program (e.g., M.D./Ph.D., M.D./M.S., summer research, year-out research), and the funding sources that are available to support student participation. Note if there is a research requirement for all medical students (e.g., a thesis or required research/scholarly project). New Jersey Medical School has several long- standing programs and one newly initiated program to support medical student participation in research. The programs are described below: MD/PhD Program The Interdisciplinary MD/PhD Program is designed as a seven-year integrated experience. The first two years consist primarily of pre-clinical medical school courses. MD/PhD students attend journal club and other scientific activities during their first two years at NJMS. Laboratory rotations are performed in the summer prior to entering medical school and/or following the first year. Years 3-5 generally involve full time research towards the PhD degree in a chosen laboratory, with a limited number of advanced graduate courses taken with other PhD students during the initial research year. The final two years of the program focuses on clinical experience through completion of the third and fourth year of medical school. Coordination between the clinical and research years is designed to facilitate a smooth transition between aspects of the Program. Academic Year _2011-2012_ Page |43 Requirements for admission to the MD/PhD Program include a strong academic record, letters of recommendation (including at least one from a research mentor), evidence of ability to succeed in a research environment, and competitive MCAT scores (GRE scores are not required). Application is made through AMCAS to New Jersey Medical School. During the NJMS application process, a supplemental application to the MD/PhD Program is required. The MD/PhD Program was co-founded by the New Jersey Medical School (NJMS) and the Graduate School of Biomedical Sciences (GSBS). These schools are strategically located in close proximity to other New York and New Jersey academic and pharmaceutical research institutions, providing a dynamic clinical and research environment. NJMS provides a superb clinical education experience through its facilities at University Hospital and other affiliated hospitals in Essex, Morris and Bergen Counties. In addition, NJMS is associated with a variety of state-of-the-art treatment and research facilities. These include the New Jersey State Trauma Center, the Center for Fertility and Reproductive Medicine, the Center for Human Molecular Genetics, the Global Tuberculosis Center, the Center for Emerging and Re-emerging Pathogens, the Cancer Center and the International Center for Public Health in Science Park. Laboratory experiences in the Program provide a thorough foundation in the theoretical and practical aspects of biomedical research. Research opportunities are available in a wide range of fields including molecular biology, biochemistry, bioinformatics, cell biology, immunology, molecular genetics, microbial pathogenesis, pathology, physiology, pharmacology and neurosciences. The research programs are well supported by numerous core facilities, including animal care, transgenic mice, mass spectrometry, molecular resource, microscopic imaging and computing services, as well as the George F. Smith library. MD/PhD Scholarships are provided to all matriculants in the Program. Scholarships include tuition waivers and a stipend during all years in the Program. The current stipend for students in NJMS years 1 and 2 is $20,000 and 26,500 for NJMS years 3 and 4. MD with Thesis Program The M.D. with Thesis Program is a relatively new program approved for implementation in AY2011-12 by our curriculum committee and subsequently faculty council. It offers a unique opportunity to NJMS medical students to conduct original research of excellent quality during their medical school training. The student is expected to devote one year exclusively to independent research that is laboratory, clinical or population-based. The additional year of research experience provides students the opportunity to study a certain subject in depth. The Program is specifically designed for a rigorous development in scientific thinking, including a thorough understanding of research methodology and scientific writing. The Program is highly suited to students who plan a career in Academic Medicine. The M.D. with Thesis Program is administered through the Office of the Senior Associate Dean for Research in conjunction with the Office of Education. The program is operated by a Committee consisting of representative faculty members from basic and clinical sciences departments and overseen by the Director of Graduate Medical Research Program who also oversees the MD/PhD program reporting to the Senior Associate Dean for GSBS-N. Students selected to the program have to be academically strong with previous research experience. The specific objectives are: training in research skills, critical thinking and formulation of a hypothesis, designing experiments that will allow for testing of the hypothesis, critical evaluation of data, and skills required to communicate scientific findings. The student may receive a stipend during the research year subject to available funding by the research mentor. During the research year the student is enrolled in the NJMS Scholars Program. The student is not charged tuition during the research year; however, student fees are assessed. Each student must remain in good academic standing in order to remain enrolled in the research program. With the permission of their research mentor and the Associate Dean for Students Affairs, students may cross-enroll in courses offered by GSBS-N or UMDNJ-School of Public Health. Participation in the M.D. with Thesis Program and/or cross-enrolled coursework cannot fulfill any requirements for the Doctor of Medicine degree program. Program has hosted two students to date. Scholar’s Program Several opportunities are available to NJMS students to take a year off to perform research. These include fellowships from the Howard Hughes Medical Institute and the National Institutes of Health. Students specifically Academic Year _2011-2012_ Page |44 interested in cardiovascular research have the opportunity to take a research year that is funded by the American Heart Association, Founders Affiliate. The Office of Research and Sponsored Programs (ORSP), Summer Student Research Program (http://njms.umdnj.edu/research/orsp/ssr.cfm) The ORSP Summer Student Research Program began in 1968. The ORSP-SSRP funding source is provided by an annual grant from the UMDNJ Foundation, donations from the NJMS Alumni and Faculty Organization., and research support for targeted students by the Hispanic Center of Excellence. The program provides a unique eight-week research experience for New Jersey Medical School's first and second-year medical students as well as undergraduate students enrolled in our combined BS/MD sevenyear program. Over the eight-week period the participants are exposed to the dynamic nature of biomedical science. During this time they learn about the methodology and results of laboratory/clinical research, sharpen diagnostic skills and learn the value and limits of experimental results. Participation also allows the students to develop a close working relationship with their mentor. Participation in the Summer Student Research Program is often the student's first research experience. It provides an opportunity for each student to evaluate the possibility of an academic career in medicine as well as appreciate the value and importance of biomedical research to tomorrow's physicians. After completing eight weeks of research in the respective laboratories, students present their research projects at the Summer Student Research Poster Symposium held in early August. At the Symposium students are interviewed and required to explain the results displayed in their poster presentation. In the summer of 2011 there were a total of 28 Students in the program and 32 Faculty mentors from across the basic science and clinical departments. Another 6 students were funded by the Hispanic Center of Excellence to conduct research and one who received HCOE funding is already included in the Summer Student Research Program. The overall total for the summer of 2011 who were sponsored by NJMS was 34. Summer Student Research Program participants have presented their research at national student research meetings. Several have received awards for platform or poster presentations of their work. This valuable experience occasionally captivates a student and determines a new career course that includes a lifetime commitment to biomedical research. Cancer Summer Student Research Program (http://njmsuhcc.umdnj.edu/home/index.php/summer-research-program.html) The Cancer Education Summer Student Research Program has been in existence at NJMS since 1969 and is supported through an NCI Cancer Education Program Grant. The summer program also begins the first week in June and ends the last week of July. This program, which has been continuously funded by the NCI for 42 years, provides a unique eight-week research experience for New Jersey Medical School's first and second-year medical students as well as undergraduate students enrolled in our combined BS/MD seven-year program to participate in oncology related summer programs and lectures series. In the summer of 2011 there were a total of 30 Students in the program with 20 Faculty Mentors. Students also have the opportunity to participate in research activities on a volunteer basis throughout the academic school year and via the work-study option. These projects are posted all year round for interested students on the ORSP website as well as the Student Financial Aid website. Department-based research opportunities There are many and varied research opportunities for students at the department level. There are several mechanisms by which students can engage in research beyond the summer programs. Formally, students can register for credit bearing research electives approved by the CAP2 (curriculum committee). Additionally, students may propose a research elective using our independent study mechanism, which allows a student to tailor their research endeavor with a particular faculty investigator. On average, a Academic Year _2011-2012_ Page |45 dozen (12) students utilize this process. The following is a list of research electives by department and the number of students enrolled in each elective in 2011-12. Research in Anesthesia Research in Family Medicine Neurosciences Research Introduction to Women's Health Research Orthopaedics Research Research in Psychiatry Research in Physical Medicine and Rehabilitation Sports Medicine/Musculoskeletal Research Otolaryngology Research Topics in Surgical Research Research in Historical Medicine Research in Urology Translational Experience in Laboratory Medicine (3rd years) Sports Medicine/Musculoskeletal Research (3rd years) 8 7 3 1 3 9 5 3 4 26 36 4 2 2 In addition, students have many informal/extracurricular opportunities to work with individual faculty members on specific projects. Students are welcome to join a basic science or clinical faculty member engaged in scholarly activities. As an example, the table below describes the range of student participation in research for the Department of Medicine. Table 1 2009-2010 26 9 6 8 No. students participating in research projects No. student first-authored publications No. student co-authored publications No. peer-reviewed abstracts presented national/international meetings No. student peer-reviewed abstracts local/regional meetings No. students abstracts presented Department of Medicine Research Day No. students with extramural funding No. students with intramural funding 2010-2011 36 14 3 10 2011-2012 26 10 3 4 TOTAL 88 33 12 22 4 5 3 12 7 9 5 21 2 3 1 6 1 3 4 12 c. Describe how medical students are informed about opportunities for participation in research. All first year students are sent an e-mail informing them about the programs and the availability of projects. Summer Program information is posted to the respective program websites as well as distributed on campus via brochures left in the Office of Research and Sponsored Programs and the Office of Admissions. Projects may include a small stipend and other projects are available through workstudy or volunteerism. Every year by the end of February, new projects are posted for the upcoming prospective Summer Program Participants. Research opportunities are made available to the students at http://njms.umdnj.edu/research/orsp/ssr.cfm. These research opportunities are competitive with a limited number of stipend funded projects. Students are required to complete an application, attach a current CV and include a brief statement indicating any prior research experience and how it relates to the current project. Each year Student Affairs hosts a Academic Year _2011-2012_ Page |46 presentation to students regarding electives and information regarding summer programs is presented. In addition, the Office for Diversity and Community Engagement targets students underrepresented in medicine reinforcing the availability of summer research opportunities sponsored by The Office of Research and Sponsored Programs, the Hispanic Center of Excellence and other external organizations. See also Part A, item (d.) in this section of the database. Academic Year _2011-2012_ Page |47 IS-14-A. An institution that offers a medical education program should make available sufficient opportunities for medical students to participate in service-learning activities and should encourage and support medical student participation. "Service-learning" is defined as a structured learning experience that combines community service with preparation and reflection. Medical students engaged in service-learning provide community service in response to communityidentified concerns and learn about the context in which service is provided, the connection between their service and their academic coursework, and their roles as citizens and professionals. "Sufficient opportunities" means that medical students who wish to participate in a service-learning activity will have the opportunity to do so. To encourage medical student participation, institutions could, for example, develop opportunities in conjunction with relevant communities or partnerships, provide information about available opportunities, offer elective credit for participation, or hold public presentations or public forums. Support for medical student participation could include offering or providing information about financial and social support for medical student service-learning (e.g., stipends, faculty preceptors, community partnerships). ___________________________________________________________________________________ a. Is there a school requirement that medical students participate in a service-learning experience, either as part of a regular course or clerkship rotation or as a selective? If so, describe the opportunities for participation and reflection on the experience NJMS does not require students to participate in service-learning; however, it is strongly encouraged and highly regarded by our students and faculty. The NJMS curriculum committee is currently discussing whether service learning will be a medical education requirement based upon a review of the education wide Goal#4: Commitment to the health of the community and appreciation of social and cultural diversity. b. Briefly describe the opportunities for medical student participation in voluntary service-learning activities. Include the types of service-learning opportunities that are available and the general level of student involvement Service-learning is a key element of the medical education experience at NJMS. Through a rich array of opportunities supported by the medical school, students are able to provide service in response to the needs of the underserved community in Newark, NJ and beyond. Faculty participation guides the connection between the service provided and academic coursework. The service-learning opportunities listed below prepare the NJMS students for continued community service during their professional careers. NJMS also recognizes that it may not capture the full scope of all activities housed within the many student organizations and interest group. The following is a list of service-learning opportunities at NJMS: Community Service Initiatives: Student Health Advocates for Resources and Education (SHARE): o Early Start Mentoring Program - Matches medical student mentors with elementary students. o Voices of SHARE - A noncredit elective that provides engaging lectures on issues pertinent to the Newark community. o Relations in Education and Community Health (REACH) – Fosters education of the community through outreach and health fairs. o Student Sight Savers - A multi-faceted student run organization offered to medical students, which focuses on the field of ophthalmology. o Student Family Health Care Clinic (SFHCC) - One of the oldest institutions at Academic Year _2011-2012_ o o o Page |48 UMDNJ. Established after the 1967 riots to meet the needs of the medically underserved, this student-run clinic offers free, quality health care to the Newark community. Partnership in Newark Advocating Community Leader's Empowerment (PINACLE) Aims to educate and empower members of the Newark community by providing useful information about pressing medical issues and by training religious community leaders in disease prevention and treatment so that they may teach their members. Students Teaching AIDS to Students (STATS) – Community outreach program providing HIV education. New Moms - Pairs medical students with pregnant teens who attend the University Hospital's OB/GYN clinic, and act as mentors, liaisons, and advocates throughout their pregnancy. Students Learning about Medicine (SLAM) - Educates and exposes students at Barringer High School to opportunities in the biomedical sciences. Dr. Richard Pozen and Ann Silver Pozen Community Scholars Program – supports’ and encourages medical student participation in community service projects locally, regionally, and internationally. Since 2008, 35 medical students have been recipients of the Pozen Community Service Scholarship Awards. The Healthcare Foundation Center for Humanism and Medicine at New Jersey Medical School – aims to advance the field of humanism by creating a “network” or nucleus of caring physicians who personify humanism in action. Through a specialized curriculum and through the Scholars’ projects they also influence their peers and instructors. Projects include: o All EARS – students spend time with patients at University Hospital who frequently have no one. They have provided invaluable support to end of life patients. o Apostle’s House - a shelter for women and children located in Newark. A reading room was implemented with everything from fresh paint, books and a computer. o Project H.I.G.H. (Humanism is Good Health) o Vocal Chords A Cappella group outreach to sick patients Mini-Med outreach for residents of The Kintock Group (transitional residence for offenders reentering the community) and The Renaissance House (a residence for troubled adolescents and women suffering from substance abuse) located in Newark. Pre-Medical Honors Program/Mini Medical School – These two programs are designed to acquaint adults and students with issues in contemporary medical practice. Lectures on topics range from the molecular basis of medicine, latest approaches in surgical care and ethical foundation for practice of health care delivery. Student Organizations – Various NJMS student organizations and local chapters of national organizations conduct their own community service and engagement activities. These include, but are not limited to: a. American Medical Association b. American Medical Women’s Association c. American Medical Student Association d. Asian American Physicians of Indian Origin e. Asian Pacific American Medical Student Association f. Student National Medical Association g. Christian Medical and Dental Association h. Muslim Students Association i. Project Pediatrics j. Global Health Alliance k. Jewish Medical Society Academic Year _2011-2012_ l. Page |49 Cross-Cultural and Integrative Medicine Interest Group In addition, there are a number of faculty sponsored activities in which students have participated or are welcome to participate. Select Faculty Sponsored Initiatives provided in Spring 2011: Teaching Internships whereby departmental research students assist in teaching science and math to high school students at Science Park High School. Laboratory Techniques Course developed with science teacher at Science Park HS that allows high school juniors to learn about science in a laboratory (at NJMS) and theoretical (at Science Park HS) setting. Participation in the "Partners in Science Program" run by the Liberty Science Center, offering summer laboratory research internships to high school students. Blood drives (in partnership with Red Cross) Provide autopsy support for community medical examiners Statewide Lead Prevention Consortium Irvington-Newark-East Orange-Paterson Lead Prevention Consortium Newark Department of Health – NJMS Department of Preventive Medicine and Community Health Partnership New Jersey Poison Information and Education System Community Outreach and Public Education in Poison Prevention Newark Collaboration for Childhood Immunization r'Kids Immunization Project in Collaboration with East Orange, Irvington, and Orange Medical Missions (Haiti, India) Telemedicine screening for eye disease Children’s RESPIRA Education Program A psychiatric resident-run free clinic for the community’s indigent population. Liver Disease Early Diagnostic Program, Access to Care For Liver Disease ( Hepatitis B, Hepatitis C and Liver Cancer) Liver Disease Survey Kiosks in Irvington, Newark and Jersey City in multiple language TRAUMA: o Safe Kids Program(Gear Up Games, International Walk to School Day, i.e.) o Photojournalism Project o Pedestrian Safety Program o Outreach with the FBI to run a Community Training Center o Outreach to run New Dimensions in Trauma Nursing and Summer Youth Scholars Program c. Describe how medical students are informed about opportunities to participate in service-learning activities. The SHARE Center student leadership, the umbrella organization for community service for 7 suborganizations, promotes service learning activities throughout the year. Students are made aware of these activities, in person via student organization leaders, postings to bulletin boards located outside the lectures and on B and C levels of the Medical Science Building, electronic monitors, and their website (http://njms.umdnj.edu/community/shareweb/index.cfm). The Office for Diversity and Community Engagement provides guidance, faculty advisors, and infrastructure support permitting program specific continuity across the years. This office also sends announcements throughout the year for the various service learning, research, and scholarship availability. It directly supports student initiated service projects with endowed funds made available by alumni donor, Dr. Richard and Mrs. Sylvia Pozen. In addition, the Office of Student Affairs and the Office of the Vice Dean via the student listserv makes Academic Year _2011-2012_ Page |50 students aware of summer internship positions, summer research and community service learning opportunities as well as scholarship information. Information is sent throughout the year as it becomes available. d. Describe how student participation in service-learning activities is encouraged, supported, and acknowledged. Include information about the sources and levels of funding available for such activities. As previously discussed, NJMS has a long tradition of service dating back to 1967 when the student body launched it first student run clinic, the Student Family Health Care Center (SFHCC). We are quite proud of being the oldest student clinic in the nation. In recent years, students have published their work and/or presented at national meetings including the Society for Student-Run Free Clinic meetings. The Department of Family Medicine provides the faculty leader and administrative support; and for many years provided the clinical space. Moving forward, the Department of Internal Medicine will provide the space which is larger. The funding to support the clinic comes from the Dean ($5,000 annually), the Alumni Office ($5,000), grants (currently a $5,000 grant from the American Psychiatric Foundation to do mental health screening at SFHCC), and fundraising by students. In addition there is funding from a five year grant (2011-2016) from the Health Resources Services Administration entitled: “Teaching innovative primary care practice models in a student-run free clinic). This grant provides nearly $200,000 per year to develop Patient Centered Medical Home and quality assurance activities as well as community outreach and interprofessional collaboration at the clinic. There is institutional in-kind support from the faculty advisors and faculty who volunteer throughout the year to provide clinical supervision at the SFHCC. This includes faculty from the departments of family medicine, medicine and emergency medicine. Additionally, faculty volunteer their effort as advisors to the student led sub-organizations that are part of SHARE as well as supervision and guidance to the many community service projects. Dr. and Mrs. Pozen provided a $1 million dollar endowment to promote service learning opportunities for NJMS students. Given the economy, we typically have $21,000 to fund student initiated service projects either throughout the academic year or in the summer. While the students have typically been rising second years we have also had fourth year students. As a Pozen Scholar, students complete an abstract, poster, and in person presentation during the annual visit with Dr. and Mrs. Pozen. Throughout the years, the Healthcare Foundation Center for Humanism and Medicine, is also an endowed office which support named humanism scholars and associates (other medical students) with limited financial scholarship support for Humanism Fellows and distributed $1,200,000.00 (more recently increasingly funded by the Dean). There is a dedicated program administrator. The Dean’s Commitment for SHARE provides for a maximum of $18,000 for the leaders to participate in developing their skills as future leaders the summer prior to their second year. Academic Year _2011-2012_ NOTE THAT STANDARD IS-15 HAS BEEN DELETED. Page |51 Academic Year _2011-2012_ Page |52 IS-16. An institution that offers a medical education program must have policies and practices to achieve appropriate diversity among its students, faculty, staff, and other members of its academic community, and must engage in ongoing, systematic, and focused efforts to attract and retain students, faculty, staff, and others from demographically diverse backgrounds. The LCME and the CACMS believe that aspiring future physicians will be best prepared for medical practice in a diverse society if they learn in an environment characterized by, and supportive of, diversity and inclusion. Such an environment will facilitate physician training in: Basic principles of culturally competent health care. Recognition of health care disparities and the development of solutions to such burdens. The importance of meeting the health care needs of medically underserved populations. The development of core professional attributes (e.g., altruism, social accountability) needed to provide effective care in a multi-dimensionally diverse society. The institution should articulate its expectations regarding diversity across its academic community in the context of local and national responsibilities, and regularly assess how well such expectations are being achieved. The institution should consider in its planning elements of diversity including, but not limited to, gender, racial, cultural, and economic factors. The institution should establish focused, significant, and sustained programs to recruit and retain suitably diverse students, faculty members, staff, and others. _____________________________________________________________________________________ a. Provide a copy of all current institutional (medical school and/or university) mission statement(s) and policies that are related to assuring a diverse student body, faculty, and staff. i. Describe the process by which these statements and policies were developed, approved, and implemented at the institution. ii. Describe how these statements and policies are made known to current and prospective applicants, students, employees, faculty, and staff. The Newark community, comprised largely of minorities, faces issues related to health disparities, educational attainment and poverty. NJMS’ commitment to minorities and disadvantaged students is closely intertwined with the University’s formal pledge to the city under the 1968 “Newark Agreements”, to provide educational and employment opportunities to its largely disadvantaged residents. This commitment materialized in 1972 with the establishment of the Office of Minority Student Affairs whose primary goal was the development of a competitive undergraduate minority/disadvantaged applicant pool for careers in medicine and other health professions. For four decades, NJMS has worked to build a pipeline sponsoring summer academic enrichment and pre-matriculation programs. Recognizing the importance of developing individuals at a younger age, NJMS’ work with high school students began in 1981. In 1991, coinciding with the award of our first Hispanic Center of Excellence (HCOE) grant, it became apparent that academic intervention should be comprehensive and occur at different stages of a student’s development. NJMS further enhanced its commitment by developing programs to specifically address the needs of Hispanic students at the pre-college, undergraduate, medical school and faculty level. We also began our work in cultural competency leveraging the goals of this federal grant. In 1992, the Office of Minority Affairs became the Office of Special Programs with a broader, more structured approach to the pipeline. This was the impetus for refinement of institutional policies and programs that broadly targeted students who were underrepresented in medicine or economically disadvantaged. With the restructuring of our pipeline programs in 1996 and the implementation of partnerships, a student can go from 6th grade through professional school without interruption of support. Over the years, NJMS has broadened its definition of diversity to include groups who are underrepresented in medicine. While NJMS considers gender, racial, cultural, and economic factors in its planning elements of diversity for its pipeline programs, it is not limited to these factors. The specific groups whose representation in the NJMS student body and faculty identified to add value to the learning environment Academic Year _2011-2012_ Page |53 have been defined as those under-represented in medicine with a focus on our community as well as New Jersey and the nation. These are African-Americans, Hispanics that include Portuguese and Brazilians (based on self-description and their representation in our community), women and those individuals who identify as LGBT. Currently, NJMS is in alignment with the AAMC Group on Diversity and Inclusion’s definition of diversity which states “diversity as a core value embodies inclusiveness, mutual respect, and multiple perspectives and serves as a catalyst for change resulting in health equity. In this context, we are mindful of all aspects of human differences such as socioeconomic status, race, ethnicity, language, nationality, sex, gender identity, sexual orientation, religion, geography, disability and age.” In 2012, the Office of Special Programs was renamed the Office for Diversity and Community Engagement (ODACE) in recognition of the breadth and depth of the programs that also support student run community service initiatives, the many non-credit electives that build on diversity, and the Healthcare Foundation Center for Humanism and Medicine. This commitment to diversity has been embedded through the NJMS strategic plans over the decades. The NJMS Strategic Plan approved in November 2012 continues to have diversity as a core value with defined strategies and measures underscoring the importance and strength that our students and faculty have placed on diversity. This process began in April 2011 with a “New Beginnings” strategic planning steering committee charged by Dr. Robert Johnson, Dean. This committee consisted of faculty, administrators and students. Subcommittees were created that led to broader engagement, which ultimately culminated in a school wide retreat with over 100 individuals in attendance. The process and retreat was facilitated by CFAR, an outside consulting firm. The plan was presented and approved by the NJMS Institutional Planning and Development committee (standing committee of NJMS) and final approval by Faculty Council, the governing body of NJMS. NJMS’ level of commitment to diversity is not only supported by our mission statement but also by our vision and value statements as stated below. Mission The New Jersey Medical School is an academic, biomedical research and healthcare enterprise whose mission is to meet the needs of the local and global community through outstanding education, pioneering research, state-of-the-art clinical care, and public service. Vision: NJMS aspires to optimize health and social well-being by: 1. Preparing humanistic leaders in global healthcare through outstanding education of physicians and scientists, building on our strength of diversity, hands-on clinical training, urban healthcare programs and transformative research. 2. Providing cutting edge tertiary and quaternary medical care of distinction, serving patients from New Jersey and beyond. 3. Enhancing our position as the top biomedical research institution in the State of New Jersey. 4. Advancing the health, education and care of the underserved and vulnerable populations by preparing a competent and diverse workforce. Values: In pursuit of our mission and vision, we value: · Integrity · Excellence · Diversity · Humanism · Compassion · Professionalism · Leadership · Innovation Academic Year _2011-2012_ Page |54 Specifically, Strategic Goal #3 addresses diversity: “Develop innovations in education to prepare students and trainees from diverse backgrounds to be collaborative practitioners of medicine, educators and researchers with a focus on the health of underserved and vulnerable populations.” It recognizes that: “Academic medicine must stay apace with the rapidly changing US healthcare system and address the anticipated physician shortage and increasing complexity of health care needs as highlighted in the Lancet Commission’s: A Global Independent Commission November 2010 publication entitled “Health professionals for a new century: transforming education to strengthen health systems in an independent world”. Select Supporting Strategies: o Supporting programs to develop future talented and diverse students in the sciences through our relationships with K-12 institutions, undergraduate programs and other medical schools. o Recruit, develop and retain a diverse faculty in order to maintain an optimal learning environment. Measures of Success include: o Funding opportunities secured to support our diverse educational mission. o Benchmarks established to ensure diversity among our student body, trainees, and faculty including their advancement and presence in leadership roles. Diversity is also embedded in the mission of our admissions statement and approved by the Admissions Committee in keeping with our strategic plans in the past and present: “to select a talented and diverse class of students who vigorously contribute to and care for the school community and society as a whole. In selecting candidates, a balanced consideration is given to attributes such as academic excellence, life experiences, resilience, personal growth and maturity; as well as various other dimensions such as socioeconomic status, languages spoken, gender, race and ethnicity. Qualities of integrity, humanism, and passion are considered as these factors may influence an applicant's potential to succeed in medical school and are critical to their growth as physician-leaders. We are committed to fostering diversity in the medical profession and actively recruit students with varied backgrounds and experiences. Our focus on cultural competency ensures that students who graduate from NJMS will be well-prepared to take care of an increasingly diverse patient population.” This can be found at: http://njms.umdnj.edu/admissions//prospective/index.cfm The same mission carries through two other key Offices. Our Office for Diversity and Community Engagement whose mission is “to develop individuals underrepresented in medicine and other health professions, as well as to champion cultural competency, community service, and humanism in all aspects of medical education”. It can be found at: http://njms.umdnj.edu/education/odace/index.cfm. The Office of Faculty Affairs assures the extension of this mission into the faculty. It recognizes that diversity enhances our ability as an academic community to foster innovation and excellence. Diversity creates and cultivates the optimal learning environment for our students and trainees and establishes a spirit of inclusiveness. This enhances NJMS’ effort to respond to the need for a diverse healthcare workforce that addresses the diversity of today’s patients (http://njms.umdnj.edu/faculty_affairs/index.cfm). At the resident, student and faculty levels, we have also focused on cultural competency training as part of our curriculum goal #4 (A Commitment to the Health of the Community and Appreciation of Social and Cultural Diversity) and New Jersey licensure requirements (http://www.state.nj.us/lps/ca/bme/press/cultural.htm) and reads as follows: “In 2005 the Legislature enacted law requiring the New Jersey Board of Medical Examiners in consultation with the Commission on Higher Education to prescribe requirements, by regulation, for physician training in cultural competency. (See N.J.S.A. 45:9-7.2 and 7.3) The regulations relating to cultural competency training were adopted in their final form on April 7, 2008. (See N.J.A.C. 13:35-6.25)” Academic Year _2011-2012_ Page |55 “The legislation requires that all medical schools in New Jersey provide instruction to their current and future students in cultural competency. This instruction is required as a condition of receiving a diploma from a college of medicine in New Jersey. New Jersey medical schools are also required to provide cultural competency CME instruction for licensed physicians who were not required to and did not receive cultural competency training in their medical school curriculum. The required curriculum in cultural competency training has become more prevalent in medical schools since 2005. The curriculum required can not be assumed to be included in medical, osteopathic and podiatric schools operating outside of New Jersey. “ Prospective applicants, students, faculty, employees and others are made aware of our commitment to diversity through our website presence including Office of Admissions, Office for Diversity and Community Engagement, and Office of Faculty Affairs. First year students also receive information about our programs and initiatives during orientation. Faculty and residents are recruited annually to participate as role models, mentors and provide clinical shadowing for student participants in our diversity related programs. The latter would not be possible without the endorsement and support received by University Hospital (UH) administration and their employees. This commitment is reflected in a formal partnership agreement between NJMS, UH, undergraduate, pre-college and community based entities. The importance of workforce diversity is introduced to new residents as part of their orientation. Residents are informed about the need for a diverse healthcare workforce that addresses the diversity of today’s patients. b. Describe how the institution defines or characterizes diversity for its students, faculty, and staff. What dimensions of diversity are considered? If different definitions apply to any of these institutional constituencies, provide each relevant definition. In the context of the definition of diversity, describe how institutional policies related to diversity are put into practice in each of the following areas: As stated under IS-16 a.i., the specific groups whose representation in the NJMS student body and faculty identified to add value to the learning environment have been defined as those underrepresented in medicine with a focus on our community as well as New Jersey and the nation. These are AfricanAmericans, Hispanics which includes Portuguese and Brazilians (based on self-description and their representation in our community), women and those individuals who identify as LGBT. We have further subdivided these for ease of tracking and terminology. We use underrepresented in medicine (AfricanAmerican, Hispanic, and Native American) and women. For LGBT, we track activities since we do not require that students self-identify. It is also important to note that many of our pipeline programs serve economically disadvantaged students (New Jersey Educational Opportunity Fund program) and also first generation college and community college students. These are tracked at the undergraduate levels but we have not established a formal mechanism for tracking matriculated students other than if than those who have been in our pipeline. i. Student recruitment, selection, and retention: NJMS has been quite effective in establishing programs to broaden diversity among medical school applicants. As evidenced by the broad range of programs available to our diverse student population, NJMS students have the opportunity to mentor and be role models to the Newark community stimulating interest in a career in healthcare and medicine. Through close partnerships and collaboration between the Offices of Admissions; Diversity and Community Engagement; Education; and Student Affairs, NJMS has gained a greater capacity in understanding and managing diversity assuring that we make admission to NJMS more accessible to potential applicants of diverse backgrounds. We have also launched an extensive network of partnerships. These are presented in greater detail under MS-8. Moreover, NJMS further accomplishes this aim through the holistic review of applicants. Academic Year _2011-2012_ Page |56 Diversity continues to be up-front and center in establishing an applicant pool. The Office of Diversity and Community Engagement is the organizational locus for enrichment programs ranging from precollege through pre-matriculation levels and are described in detail under MS-8. Below is a list of the programs. From 2009-2011 there were a total of 2,500 students who participated in enrichment programs. This total may represent a duplicated count since a student may participate more than once across the various programs. Pre-College Young Explorers - NJMS SMART Initiative ChemPros - NJMS SMART Initiative Biotrek - NJMS SMART Initiative Fantastic Voyage - NJMS SMART Initiative Enviroquest – NJMS SMART Initiative Mission Health - NJMS SMART Initiative Biomedical Apprenticeships - NJMS SMART Initiative NJMS Pre-Medical Honors Program The Public Health Research Institute Summer High School Research Internship Program The Hispanic Center of Excellence Summer Youth Scholars Program (SYSP) Undergraduate Programs AAMC Robert Wood Johnson Foundation Summer Medical & Dental Education Program Northeast Regional Alliance (NERA) MedPrep Scholars Program Hispanic Center of Excellence in partnership with Rutgers University (New Brunswick) Success in the Sciences (SIS) Program Pre-matriculated/Matriculated Programs Freshman Introduction to Resources and Skills Training (F.I.R.S.T) In addition to the aforementioned programs, a number of student organizations are actively engaged in service. These community outreach and education activities target underrepresented minorities and other disadvantaged groups represented in our community. These include activities led by the Healthcare Foundation Center for Humanism and Medicine, the local chapters of national student organizations such as the Student National Medical Association (SNMA), SHARE Center Early Start Mentoring Program, Pozen Scholars program, and the Latino Medical Student Association (LMSA). NJMS continues to rank amongst the most diverse medical schools in the U.S. for students and faculty. Academic Year _2011-2012_ Page |57 The above table was copied from the AAMC Missions Management Tool 2012 prepared for UMDNJNew Jersey Medical School. This provides us with a six (6) year average through 2010. NJMS student body is both cohesive and diverse, valuing its representation of women and non-traditional students and a wide variety of cultural and ethnic backgrounds. NJMS takes pride in the accomplishments of all its students, providing an environment of openness and freedom to express and enjoy their cultural identity and those of fellow students. NJMS has, however, experienced a modest downward trend in its diversity leading to an increased focus on the development of the pipeline, through recruitment and targeted strategies, with a particular focus on women and African-American men. Over the past 5 years, NJMS established and sustained major pipeline programs, increased its partnerships and maintained its longstanding relationships with over 50 community-based organizations, public schools, community colleges, universities and student pre-health organizations. These programs have significantly enhanced the applicant pool, and NJMS has tracked our undergraduate participants. The pipeline programs have been successful in contributing to a more diverse medical student applicant pool for NJMS and other medical schools, both allopathic and osteopathic. Between 2010 and 2012, 448 students participated in undergraduate enrichment program. (See MS-8), 72 have entered medical, osteopathic and/or dental school and Academic Year _2011-2012_ Page |58 a number of them are still in college. In 2012, 56 students from our pipeline programs entered medical school. Our partnership with Rutgers Success in Science is a model collaboration where academic advising and strategic approaches have resulted in more competitive undergraduate applicants. We have developed relationships and/or partnerships with Educational Opportunity Fund Directors (responsible for economically disadvantaged students) and Minority Association of Pre-Health Students (MAPS) chapters in 21 communities and four-year undergraduate institutions through extensive outreach. Our focus on community colleges helps student’s transition to four-year institutions, increasing their competitiveness. The Admissions Office has an Admission Diversity Plan that applies the holistic review process, which seeks to attract well-qualified students from diverse backgrounds who are committed to academic excellence, clinical service and research. NJMS leverages federal and private dollars combined with significant in-kind institutional support for its pipeline programs and recruitment activities, as well as activities related to its partnerships. There are dedicated staff members from NJMS for all such programs. These recruitment efforts have resulted in a total enrollment of African-American and Hispanic students of 129/751 or 17% and women (includes minorities) of 308/751 or 41% in 2011-12. Of the 129 students, 43 or 26% are products of NJMS pipeline programs. While we cannot formally document the number of LGBT students, our work with the NJMS student group reveals a visible upward trend. Our Vice Dean, past chair of the AAMC Group on Diversity and Inclusion, has spearheaded an environment of broader inclusiveness at NJMS. LGBT students are on our admissions committee, in our MD/PhD program, and engaged in increasing LGBT health related topics in our required and non-credit curriculum. In addition, our student organization has been re-invigorated renaming the club, OUT@NJMS. Through our work locally and nationally our LGBT students are invited and plan to network with NY area medical schools on LGBT activities. IN 2011, our LGBT students launched a non-credit elective addressing sexual health in medicine. The non-credit elective format is a commonly accepted and valued method of incorporating topics that students deem important as part of their experience at NJMS. This elective addresses LGBT sexual health topics alongside general sexual health topics, sending the message that both are equally important. Furthermore, to support LGBT students, NJMS has actively sought to have faculty development activities including workshops and grand rounds. Presently, there are ongoing efforts to provide a safe environment where students and faculty are able to “come out”. Our ultimate goal is to make data collection possible which can inform future strategies and programs. Women Applicant to Matriculate Trends table reflects the changes over the past three years among women and underrepresented in medicine (African-American, Hispanic, and American Indian) students, faculty and residents. The self-description for the resident data was changed in 2010, in part accounting for the changes in Hispanics since they now report by race and ethnicity, selecting more than one category. While our current total student enrollment reflects a strong diversity we have experienced a downward trend in the number of African-American (women out number men), and Hispanic matriculants. While women are well represented in the NJMS total student body, we have also witnessed a downward trend. For each targeted group, we have provided our trend data, pipeline activities, and strategies that are in progress or planned. Academic Year _2011-2012_ Page |59 Underrepresented in Medicine (Black, American Indian, & Hispanic) Graduating Class Total Applicants 2009 2010 2011 2012 2013 2014 2015 2016 4,057 4,331 4,803 4,332 ***3926 ***3451 ***3312 ***3457 URM 838 (155 NJ) 867 (153 NJ) 975 (166 NJ) 775 (140 NJ) 702 (174 NJ) 634 (163 NJ) 525 (167 NJ) 645 (192 NJ) Blacks 528 (96 NJ) 525 (85 NJ) 574 (112 NJ) 454 (83 NJ) 433 (112 NJ) 376 (97 NJ) 302 (86 NJ) 370 (100 NJ) American Indians 18 (4 NJ) 21 (2 NJ) 22 (3 NJ) 12 (1 NJ) 7 (1 NJ) 5 (2 NJ) 9 (3 NJ) 9 (4 NJ) Hispanics 292 (55 NJ) 321 (66 NJ) 369 (51 NJ) 309 (56 NJ) 262 (61 NJ) 253 (64 NJ) 214 (78 NJ) 266 (88 NJ) Total Offers of Acceptance 415 417 409 395 ***384 ***371 368 358 URM 125 (48 NJ) 113 (55 NJ) 109 (52 NJ) 87 (53 NJ) 57 (34 NJ) 94 (68 NJ) 74 (51 NJ) 82 (71 NJ) Blacks 67 (26 NJ) 58 (30 NJ) 53 (23 NJ) 42 (26 NJ) 28 (19 NJ) 49 (37 NJ) 30 (22 NJ) 35 (32 NJ) American Indians 0 1 (1 NJ) 1 (1 NJ) 1 (1 NJ) Hispanics 58 (22 NJ) 54 (24 NJ) 56 (29 NJ) 45 (27 NJ) 29 (15 NJ) 45 (31 NJ) 43 (28 NJ) 46 (38 NJ) Matriculated 170 170 178 194 ***171 ***178 178 178 URM 53 (31NJ) 42 (30 NJ) 37 (25 NJ) 36 (30 NJ) 28 (22 NJ) 36 (33 NJ) 29 (22 NJ) 36 (34 NJ) Blacks 26 (17 NJ) 19 (15 NJ) 15 (9 NJ) 17 (15 NJ) 12 (11 NJ) 17 (16 NJ) 14 (13 NJ) 14 (13 NJ) American Indians Hispanics 0 27 (14 NJ) 0 0 23 (15 NJ) 0 0 22 (16 NJ) 0 0 19 (15 NJ) 0 0 16 (11 NJ) 0 19 (17 NJ) 0 15 (9 NJ) 1 (1 NJ) 21 (20 NJ) ***Includes 7 and 8 year, Deferred and Rutgers Articulated Students The above table shows the trend over the past 8 years for underrepresented in medicine (AfricanAmerican, Hispanic and Native American) applicants for the respective entering classes. We continue to track American Indians as part of our social responsibility. The opportunity for NJMS to engage students who identify as American Indians is through our Robert Wood Johnson Foundation Summer Medical and Dental Education Program (RWJF-SMDEP) which brings 80 undergraduate students each summer to our campus from across the nation. For the entering (graduating) classes of 2009 (2013), 2010 (2014), 2011 (2015), NJMS experienced a steady decline in the total number of underrepresented applicants. This coincided with the Board of Trustees decision in 2008 to require a one year NJ residency status in order to become eligible for in-state tuition. Out-of-state tuition is almost $20,000 higher. On a slightly more positive note, the number of New Jersey underrepresented individuals applying and accepted to NJMS has steadily increased. The entering class of 2012 has garnered the most NJ underrepresented applicants (192) and acceptances (71) over the 8 year period with increases largely attributed to Hispanics. We attribute this increase to our pipeline programs and increased outreach to students in the tri-state area as part of our Northeast Regional Alliance Med Prep Scholars program with Mount Sinai, Columbia, and the Staten Island Area Health Education Center as well as the RWJF Summer Medical and Dental Education national program. Although we are beginning to see increases, the number matriculating has not kept pace, particularly, with African American males and Puerto Rican applicants in general. In response to the decline in African-Americans, in particular men, NJMS launched a new initiative in Academic Year _2011-2012_ Page |60 November, 2012 “Men of Distinction Chapter.” Committee members include African-American and Hispanic male faculty, residents and alums that are charged with assisting NJMS in the recruitment, development, and retention of African American and Hispanic males. They will provide guidance on effective strategies to attract, develop, and graduate men who have become significantly underrepresented in medicine as well as serve as role models and mentors for matriculated students. The Office for Diversity and Community Engagement continues to: (1) work closely with the Office of Admissions in increasing the school’s recruitment outreach to collegiate pre-med advisors from the tri-state area; (2) mentor and develop pipeline students through the Northeast Regional Alliance Med Prep Program: a 3year summer enrichment program for underrepresented, as well as economically and educationally disadvantaged students interested in medicine, and the longstanding RWJF SMDEP programs; and (3) provide drop in consultations to any student interested in applying to NJMS (see MS-8). Women Applicant to Matriculant Trends Graduating Class Total Applicants Males Females % Female 2009 4,057 1,904 2,149 52% 2010 4,331 2,083 2,248 51% 2011 4,803 2,306 2,497 51% 2012 4,332 2093 2239 51% 2013 3926 1895 2028 51% 2014 3451 1641 1810 52% 2015 3312 1679 1633 49% 2016 3457 1770 1682 48% Offers of Acceptance Males Females % Female 415 196 219 52% 417 215 202 48% 409 201 208 50% 395 216 179 45% 384 206 178 46% 371 184 187 50% 368 193 175 47% 358 193 165 46% Matriculated Males Females % Female 170 86 84 49% 170 95 75 44% 178 94 84 47% 194 121 73 37% 171 97 74 43% 178 94 84 47% 178 110 68 38% 178 113 65 36% Women have traditionally represented 44-47% of the class. The data on women matriculates was discussed by the admissions committee and presented to Faculty Council, our governing body, in October 2012. This was driven by the concern that for two years in a row, our women matriculates were much lower than in many of the previous years. The above table shows the trends over the past 8 years including the entering class of 2012 (graduation, 2016). While the absolute numbers have declined over time, the % of female applicants and offers of acceptance has remained consistent. For those women who were accepted for the entering class of 2012, but decided to attend other schools, the preponderance matriculated at Robert Wood Johnson Medical School, our sister school, and NY area medical schools. It should be noted that the majority of the applicants to NJMS are NJ residents. Past strategies have included NJMS female students calling accepted applicants. The admissions committee has and continues to discuss recruitment strategies for women. Some of the initiatives include: • • • • • • • • Increased interaction during visits Increase female faculty/student participation in admissions process Ongoing efforts to improve “appeal” of NJMS Assess competitiveness with other institutions Proactively address potential concerns Survey matriculates and students who were accepted and withdrew Partner with AMWA student chapter Highlight the accomplishments of women students and faculty The Office for Diversity and Community Engagement led by our Vice Dean continues to engage our Out @ NJMS LGBT student chapter by supporting panel discussions and admissions seminar that will be held in the spring of 2013. Academic Year _2011-2012_ Page |61 Our diversity efforts also encompass providing the highest level of student support that culminates in student retention and graduation rates for the targeted groups. To achieve this, there is a strong partnership between the Offices of Diversity and Community Engagement and the Office of Student Affairs. These begin at the pre-matriculation level with our Freshman Introduction to Resources, Skills and Training program where the student also meets with the Center for Academic Success and Enrichment (C.A.S.E.). This Center was established in 2007 to assist students in their transition into and through medical school and with their development as physicians. Its mission is to develop and implement programs to further the academic goals of NJMS and to track the success of individual students in meeting these goals. Students who have difficulty meeting these goals are identified by the Center and are assessed to determine what interventions are needed to assist them in securing their academic success. CASE provides or where appropriate oversees these interventions. CASE develops and provides training experiences to assist the student body as a whole with the various transitions involved in developing into a physician as well as their USMLE preparation. CASE also works with the Office of Education to create training programs for faculty that will further enrich the academic climate and potential of the student. Particular focus is placed on those matriculants who participated in the FIRST program and those identified as underrepresented in medicine. Students receive an individual assessment of academic strengths, weaknesses and learning styles during FIRST and meet with Drs. Karl and Hill, Office of Student Affairs, to have a learning and psychosocial history taken to assess for any potential problems that might impede the student's success once school begins. This evaluation covers the student's previous academic history and any psychosocial problems that might need intervention. CASE tracks the student progress throughout the four-year curriculum; provided relevant workshops and consultations. This includes tutoring and standardized test-taking support funded by the Hispanic Center of Excellence, Health Careers Opportunity Program grant and other resources. This has helped students enhance their critical thinking and problem solving skills in preparation for the United States Medical Licensing Exams. The assessment also includes a review of the student's language history and skills. In our experience biand multilingual students frequently have difficulty managing the timing constraints on shelf and board exams. This is particularly evident in students who have recently immigrated or who have only been speaking English for a few years. Depending on the students linguistic history formal testing may be done to assess whether reading speed and accuracy is impacted. If there is evidence of difficulty in this area a program is developed to assist the student in acclimating to reading English at the rate usually required on NBME exams. To assess the effectiveness of our interventions we track the progress of underrepresented students separately. For the entering class of 2007, our overall retention rate for these students (African-American, Hispanic and Native American) is 92%. NJMS continues to enjoy a high retention rate. ii. Financial Aid: Recognizing the importance of financial aid, NJMS participates in numerous federal, state; Universitybased and privately sponsored programs http://www.umdnj.edu/studentfinancialaid/app_process/major_programs.htm. These include Scholarships and Loans for disadvantaged students, Primary Care Loan and Educational Opportunity Fund. The Office of Student Affairs works closely with the Office of Financial Aid in meeting the current and emerging needs of students. It does not track students according to race/ethnicity or gender. NJMS, however, through its Office of Diversity and Community Engagement works with Financial Aid and Office of Student Affairs to address the emerging needs of any underrepresented and/or any pipeline student (those who have participated in any pre-college or undergraduate program). The New Jersey Medical School, as a federal grantee on a number of diversity related grants, is required to report financial aid support for the targeted group. For example, during the competitive renewal for our Academic Year _2011-2012_ Page |62 Hispanic Center of Excellence grant in May 2012, we provided information indicating that all matriculated Hispanic students were afforded financial aid. The breakdown of the types of support for the 79 (based on total enrollment) was: 8% self-pay, 51% scholarships/grants, 3% tuition waiver (MD/PhD) and 90% student loans. Please note that these categories are not mutually exclusive. In addition, students are eligible to receive scholarships provided by the dean, alumni association and other donors. These include the HealthCare Foundation Humanism Scholarship, NJMS Alumni Association Scholarships, and the New Jersey Health Foundation (that includes Foundation of UMDNJ). For AY 12-13, the Dean approved six (6) $10,000 Academic Excellence scholarships; however, because it was late in the cycle, five (5) $5,000 scholarships were awarded. Our commitment is such that no student goes without the aid needed to support their medical education. iii. Educational Program NJMS has long recognized that developing and enhancing cultural competency is a life-long commitment and an on-going process to better understand ourselves and to communicate and work effectively across cultures. While our faculty and students have always taken pride in their ability to care for the underserved it was not until 1991 when NJMS was awarded the Hispanic Center of Excellence that we began to track our cultural competency education. The first programming began in 1992 in the form of non-credit electives and has over the decades developed into a longitudinal curriculum, consisting of didactic and experiential sessions. In 2004, the New Jubilee Curriculum, (last comprehensive revision), set forth as one of our six curricular goals: Goal #4: A Commitment to the Health of the Community and Appreciation of Social and Cultural Diversity. This has provided the platform for developing students who value diversity and can be advocates for the community and provide cross-cultural care to underserved populations. The educational programs are also coupled with faculty development and now extend across the entire academic community inclusive of pipeline students at all levels, medical students, residents, faculty and administrators. The pre-clinical courses and clerkship rotations in which students learn about issues related to diversity, health equity and cultural competence in health care can be appreciated in the tables provided under ED21-22. While there are a number of non-credit electives offered in the first two years, a few are particularly noteworthy. The Medical Interpreter elective (addresses the needs of the Limited English Proficient and low health literacy populations); Human Sexuality in Medicine (addresses the needs of the LGBT population) and a new Student Family Health Care Center grant initiative (addresses the needs of Newark’s underserved populations). In addition, as part of the cultural competency curriculum, service learning continues to be a major benefit allowing students to practice their newly acquired cultural competency skills. For AY 2012-13, the curriculum committee approved a longitudinal service learning elective, which includes self-reflection. iv. Faculty/staff recruitment, employment, and retention Faculty: NJMS leadership, faculty and administrators have long recognized the importance of having a diverse faculty in both caring for our patients as well as enhancing the learning environment. For decades, NJMS has sought to achieve the highest level of diversity amongst its faculty focusing on women and minorities as those underrepresented in medicine. Our challenge continues to mirror the nation in the retention of minority faculty and their overrepresentation among junior academic ranks (see v. Faculty Development). In recent years, NJMS has been quite successful in the recruitment of a diverse group of faculty. The dean's commitment to diversity has been a constant message beginning with his appointment as Interim and now permanent dean. He has appointed or supported the appointment of women to senior roles within the institution which include the Vice Dean, Associate/Assistant Deans (3), Director of Scientific Research (1), Director of the Faculty Mentoring Program (1) and Interim Chairs (4). In addition, he has strongly encouraged applications for the Executive Leadership in Academic Medicine Academic Year _2011-2012_ Page |63 program (ELAM) with two women completing the program, one who subsequently became an Interim Chair. In April 2011, the Dean charged a “New Beginnings” strategic planning committee. In addition, with the Dean’s support, NJMS collaborated with the American Association of Medical Colleges (AAMC) and a cohort of twelve other US medicals in administering the Faculty Forward Engagement Survey to our fulltime and part-time faculty in the fall of 2011. This confidential survey is designed to assess levels of medical school faculty engagement and satisfaction with their places of employment. NJMS obtained an excellent response rate; 385 of 550 faculty invited (66.4%) responded to the survey, 5% better than the cohort as a whole. We received the results of the survey in April 2012. The Faculty Forward Steering Committee has begun to delve into the very robust data set supplied by this survey. A preliminary review reveals that NJMS scored higher than the cohort on the question, ‘I feel that the workplace culture at NJMS cultivates diversity’. Our newly approved strategic plan continues to support our recruitment and development of a diverse faculty. For the first time, it addresses our residents and fellow trainees. Also, Strategic Goal #3 acknowledges the impact a critical mass of diverse faculty can have in attracting more diverse students to the health professions, the learning environment, shaping institutional policies and practices, serving as role models and championing research on healthcare disparities, to name a few. The newly approved plan puts forth as a supporting strategy: “recruit, develop, and retain a diverse faculty in order to maintain an optimal learning environment.” The corresponding measure of success is: “Benchmarks established to ensure diversity among our student body, trainees, and faculty including their advancement and presence in leadership roles.” At the same time, the dean charged the chair search committees to provide him with candidates for leadership positions that are inclusive of women and minorities given the number of vacancies. NJMS redoubled its efforts to achieve a diverse applicant pool for all leadership positions. Members of Chair search committees are carefully selected to include women and underrepresented minorities. Thus, search committee members are also able to serve as recruiters of diverse candidates. Each search committee meets with the associate dean for faculty affairs who addresses diversity and unconscious bias. The recruitment process actively reaches outside of standard networks. Ads are placed in journals that target minorities and women for job-specific positions. Job descriptions offer a clear sense of institutional climate. Specific Websites targeted: Latpro.com Goldsea.com Diversity.com AMA/Women’s Congress through AMA ELAM The AAMC Missions Management Tool 2012 prepared for UMDNJ-New Jersey Medical School addresses the diversity of our full time, paid faculty through 2010. It should be noted that only a few faculty from our affiliated hospitals who are co-terminus with funding are included in this count. Our Faculty demographics placed NJMS just above the 70th percentile for women and minority (undercounted in the report since it only reflects full time Hispanic, African-American, American Indian, and Alaskan Native) faculty when compared to other medical schools. Table under section c provides a three-year trend for faculty. The concept of Growing Our Own continues to be important. A snapshot of the faculty in March 2012 revealed that of the 79 full and part-time minority faculty, 28 or almost 35% are either alumni and/or residency training program graduates. Between April and October 2012, we lost four (4) minority faculty: one retired, one after almost 20 years left to practice in a rural community, one moved to volunteer status Academic Year _2011-2012_ Page |64 and one took another academic position. However, since July 2012, NJMS has recruited 9 new AfricanAmerican and Hispanic faculty (seven full-time, two part-time); 4 of whom are NJMS alums and/or residents who were part of the pipeline to academia. One is the recipient of a HRSA loan repayment for which NJMS is providing matching funds. Our challenge will be to continue to strive for the highest retention. Residents: As a result of ACGME competencies (IV.A.5.d and e professionalism), NJ licensure mandates, and our curriculum Goal #4 (A Commitment to the Health of the Community and Appreciation of Social and Cultural Diversity) our efforts for residents have centered on cultural competency and health equity training for all trainees. Residents receive this training during the new housestaff and fellows orientation, noon conferences, and grand rounds. There were a total of 448 residents and 62 fellows (duplicated counts based on grand rounds attendance) that received cultural competency training from 2009-2012. Moreover, 177 (2010-11) and 186 (2011-12) new residents/fellows received training during the annual New Housestaff Orientation. We have worked hard to retain our graduates who are underrepresented in graduate medical education programs. At the residency/fellowship program level we have not had a systematic approach to the extent we have had for medical students and faculty. Currently NJMS offers 46 residency and fellowship training programs. Residents and fellows are considered employees of the University. As such demographic information is collected by Human Resources. In 2010-2011, UMDNJ Human Resources introduced a new in-take form which separated race and ethnicity. Possibilities for the inconsistencies in the data regarding race and ethnicity include: 1) how the self-description was categorized and 2) an absolute decline, or 3) both. The representation of women and African-American trainees has remained steady; however, the number of Hispanic trainees has significantly decreased over the past 3 years keeping in mind that Hispanics can be represented along any of the racial categories. For AY 2012-2013, the Assistant Dean for Graduate Medical Education is conducting a program director’s survey to include current strategies and perceived barriers. This will serve to raise awareness (unconscious bias) and to develop strategies and metrics using program specific criteria to enhance diversity. NJMS acknowledges the impact that a diverse resident/fellow workforce can have on medical education, serving as role models and contributing to patient care. In continuing to grow our own we also plan to target trainees in our programs for faculty positions. Specifically, we will discuss careers in academia, their professional development, faculty vacancies at NJMS and the Centers of Excellence Consortium institutions. Future strategies include a visiting student elective program which invites students from diverse backgrounds during their last year of medical school to apply for senior elective rotations at NJMS. Women and men will be defined according to those specialties in which they are underrepresented such as women in radiology and orthopeadics and men in obstetrics and gynecology. Another strategy is an annual residency showcase targeting students from diverse backgrounds particularly those students from groups underrepresented in medicine. Participants will have the opportunity to hear panel discussions with Program Directors and current residents. v. Faculty development It is imperative that we not only recruit a diverse faculty but also develop them to succeed. It is through their representation and advancement that their voices can result in meaningful change. Therefore, a number of faculty development activities take place under our federally funded Hispanic Center of Excellence that includes individualized and group training and has been strongly endorsed by the department chairs. During 2009-2012, activities ranged from grant writing; how to publish workshops; sessions on enhancing negotiation skills; quantitative methods; specialized lab training; and department seminars in the respective discipline. Participation in national meetings and conferences enabled collaborations with other investigators resulting in grant submissions and invitations to national and international meetings, a requirement of promotion to senior title ranks. Several of the faculty trainees Academic Year _2011-2012_ Page |65 were sponsored to attend small, intensive invitation only meetings. Five faculty attended the AAMC Minority Faculty Development program that is uniquely tailored for the advancement of faculty underrepresented in medicine providing an additional opportunity for networking. A Centers of Excellence Consortium on Minority Faculty Development consisting of NJMS led by Dr. Soto-Greene, Vice Dean and Principal Investigator of the Hispanic Center of Excellence, Mount Sinai School of Medicine, Meharry Medical College, University of Pennsylvania School of Medicine, University of Texas Medical Branch at Galveston, and University of Puerto Rico School of Medicine was established in July 2012. The overall goal of the COE Consortium is to increase the collective capacity to attract, develop, and retain underrepresented physician and biomedical scientists for successful careers in academic medicine within a community of institutions committed to advancing diversity. Each partner will sponsor a faculty development seminar annually over 5 years. The sessions may be conducted with the use of technology such as skype and video conferencing to permit maximum participation. The faculty development seminar targets junior faculty and advanced fellows. In addition to the enhancement of faculty skills, as a result of the faculty development conferences/activities, this partnership plans to: 1) establish external mentoring opportunities, 2) provide access to new databases and patient populations for research purposes, and 3) foster peer networking and peer collaborations. Partners hold quarterly conference calls to discuss faculty development and inter-institutional mentoring opportunities for junior faculty. Faculty will have access to a compendium of programs, mentors and resources by June 2013. Sample topics include: Understanding and writing grants, How finance drives your institution; How to get published; Successful medical research approaches: Opportunities in Academic medicine; Mapping your academic career; Exploring leadership roles in medical education; The influential role of department chairs and division chiefs in advancing institutional diversity and, Having difficult conversations. Our approach includes collaborative mentors both inside and outside of the institution. NJMS’ Junior Faculty Mentorship Program and HCOE Faculty Development Programs are the cornerstone to retaining a diverse faculty. In addition informal social networks create venues to socialize, share stories, and celebrate diversity. This creates a sense of community and belonging which enhances retention. Moreover, as a federally funded Centers of Excellence, retention is further addressed with the following guidelines: Mentorship…Mentorship…Mentorship!!! Individualized Academic Plan is a must Beware and protect against the "culture" tax Establish clear timelines for achievement of the goals delineated in Academic Plan Provide opportunities for development which must include protected time Be specific regarding requirements and progress towards attainment of promotion and/or tenure Be flexible In the past three years, these efforts have resulted in the promotion of three minority faculty to associate professor and two others recruited into or placed on the tenure track. One assumed the role of division chief, who was also a HCOE medical student. vi. Liaison activities with community organizations The New Jersey Medical School enjoys partnerships, collaborations and liaison activities with a broad range of community organizations. These specifically address our education, pipeline development and service activities. Under the sections above (i. and iii.) and IS-14 we have put forth some of the relationships. We also partner with the Staten Island Area Health Education Center as part of the Northeast Regional Alliance; and the North Hudson Community Action Corp., a large Federally Qualified Health Center which serves as a clerkship rotation site and also refers students to our pipeline programs. The 4th year public health clerkship also works with a number of community organizations for medical student placement. Academic Year _2011-2012_ Page |66 The STUDENT FAMILY HEALTH CARE CENTER (SFHCC) has been providing care to Newark’s uninsured and underinsured residents since 1967. Students join the clinic in their first year with third year students assuming the role of team leader. It provides a unique opportunity to care for those who often have no other place to go. Students enhance their understanding of the complexities of the delivery of care when access, language, education, and other socioeconomic factors are involved. This clinic is offered two evenings a week. Approximately (30-40 %) of clinic patients are Spanish-speaking. Implemented this year, the SFHCC has partnered with Casa Israel: older adult medical day care center, therapeutic and recreational services, primary and preventive health care (120 clients/day), La Casa de Don Pedro Community Centers: youth, family and counseling assistance, adult development including a Hispanic women’s resource center, senior programs and domestic violence (5 sites), St. James Social Services Corp: after school youth programs, workforce development training, feeding programs, computers for seniors, food pantry (10,000 clients/year), Vision of Hope Community Development Corp: juvenile delinquency, substance abuse, domestic violence, lack of affordable housing, legal help, child care, feeding program, ex-offenders re-entry, Fairmount Homeless Shelter: nighttime shelter, evening meals for about 40 homeless men and women who need on-site basic primary clinical care for acute and chronic diseases, Newark Now: 15 Family Success Centers providing residents with tools to improve their neighborhoods. There is need for increased health literacy and health education for all clients. Two agencies have predominantly Spanish-speaking clients. MINI MEDICAL SCHOOL OUTREACH works with the residents of The Kintock Group (transitional residence for offenders re-entering the community) and The Renaissance House (a residence for troubled adolescents and women suffering from substance abuse) located in Newark. STUDENTS LEARNING ABOUT MEDICINE (SLAM), sponsored by the Latino Medical Student Association, serving as role models to 9-12th graders attending University High and East Side High School with a large Hispanic population exposing them to health professions. The VOICES OF SHARE a year long elective brings together the diverse community outreach and educational programs directed by or affiliated with SHARE Center, our student community service umbrella organization. It consists of an educational lecture series and a community service requirement. Each lecture will focus on an issue to the Newark community and enhancing the understanding of our minority community. STATS (Students Teaching AIDS to Students) works with children and adolescents affected by HIV and AIDS through mentoring and tutoring. Early Start Mentoring Program (ESMP) pairs mentors with at-risk Newark elementary school children. PINACLE (Partnership in Newark Advocating Community Leader's Empowerment) aims to educate and empower using a train-the-trainer model. The partners represent various religious organizations located in our community. c. Based on the institution’s definition of diversity and the LCME standard that “medical schools should consider in their planning elements of diversity including, but not limited to, gender, racial, cultural and economic diversity,” report in the table below information regarding the percentage of enrolled students and employed faculty and staff in each of the categories included in the institution’s definition of diversity In keeping with the University, NJMS reports the racial, ethnic and gender categories provided in section c. (below). As stated under IS-16 a.i., the specific groups whose representation in the NJMS student body and faculty identified to add value to the learning environment have been defined as those underrepresented in medicine with a focus on our community as well as New Jersey and the nation. These are African-Americans, Hispanics that include Portuguese and Brazilians (based on self-description and their representation in our community), women and those individuals who identify as LGBT. While NJMS has been reporting on residents it is only now that we have included them as a strategic group that will address diversity more holistically. Academic Year _2011-2012_ Page |67 NJMS Report on Racial, Ethnic and Gender Categories Ethnicity/Race/Year First year Students All Students Faculty Residents 2009-2010 N=185 M=103 F=82 N=750 M=428 F=322 N=648 M=403 F=245 N=619 M=335 F=284 Hispanic 20 (10.8%) 85 (11.3%) 30 (4.6%) 73 (11.8%) Black/African American 15 (8.1%) 69 (9.2%) 35 (5.4%) 58 (9.4%) American Indian/Alaskan Native 0 (0%) 2 (0.27%) 0 (0%) 0 (0%) Asian/Pacific Islander 78 (42.2%) 291 (38.8%) 172 (26.5%) 228 (36.8%) White 61 (33%) 254 (33.9%) 406 (62.7%) 252 (40.7%) Other 11 (6%) 49 (7.9%) 5 (0.8%) 8 (1.3%) Ethnicity/Race/Year First year Students All Students Faculty Residents 2010-2011 N=186 M=100 F=86 N=754 M=431 F=323 N=643 M=397 F=246 N=607 M=325 F=282 Hispanic 21 (11.3%) 83 (11%) 30 (4.7%) 55 (9.1%) Black/African American 17 (9.1%) 61 (8.1%) 35 (5.4%) 63 (10.4%) American Indian/Alaskan Native 0 (0%) 0 (0%) 0 (0%) 0 (0%) Asian/Pacific Islander 74 (40%) 300 (40%) 176 (27.4%) 227 (37.4%) White 56 (30%) 259 (34.3%) 397 (61.7%) 254 (41.8%) Other 18 (9.7%) 51 (6.8%) 5 (0.8%) 8 (1.3%) Ethnicity/Race/Year First year Students All Students Faculty Residents 2011-2012 N=183 M=113 F=70 N=751 M=443 F=308 N=643 M=395 F=248 N=594 M=320 F=274 Hispanic 16 (8.7%) 71 (9.5%) 29 (4.5%) 46 (7.7%) Black/African American 14 (7.7%) 58 (7.7%) 35 (5.4%) 55 (9.3%) American Indian/Alaskan Native 0 (0%) 0 (0%) 0 (0%) 0 (0%) Asian/Pacific Islander 73 (40%) 302 (40.2%) 174 (27%) 241 (40.6%) White 61 (33.3%) 260 (34.6) 396 (61.6%) 246 (41.1%) 19 (10.4%) 60 (8.0%) 9 (1.4%) 6 (1.0%) Other See also information for standard ED-21 and standard MS-8 in Section III: Medical Students END OF SECTION I