The Client with Reproductive Health Problems
advertisement
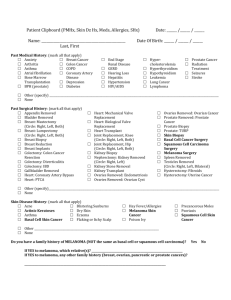
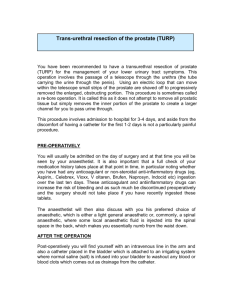
The Client with Reproductive Health Problems TEST ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ ■ The Client with Uterine Fibroids The Client with Breast Disease The Client with Benign Prostatic Hypertrophy The Client with a Sexually Transmitted Disease The Client with Cancer of the Cervix The Client with Cancer of the Ovaries The Client Having Gynecological Surgery The Client with Testicular Disease The Client with Cancer of the Prostate The Client with Erectile Dysfunction Managing Care Quality and Safety Answers, Rationales, and Test Taking Strategies The Client with Breast Disease 23. A postmenopausal woman is worried about pain in the upper outer quadrant of her left breast. The nurse’s fi rst course of action is to: ■ 1. Do a breast examination and report the results to the physician. ■ 2. Explain that pain is caused by hormonal fl uctuations. ■ 3. Reassure the client that pain is not a symptom of breast cancer. ■ 4. Teach the client the correct procedure for breast self-examination (BSE). 24. The nurse teaches a female client that the best time in the menstrual cycle to examine the breasts is during the: ■ 1. Week that ovulation occurs. ■ 2. Week that menstruation occurs. ■ 3. First week after menstruation. ■ 4. Week before menstruation occurs. The Client with Breast Disease 23. A postmenopausal woman is worried about pain in the upper outer quadrant of her left breast. The nurse’s fi rst course of action is to: ■ 1. Do a breast examination and report the results to the physician. ■ 2. Explain that pain is caused by hormonal fl uctuations. ■ 3. Reassure the client that pain is not a symptom of breast cancer. ■ 4. Teach the client the correct procedure for breast self-examination (BSE). 24. The nurse teaches a female client that the best time in the menstrual cycle to examine the breasts is during the: ■ 1. Week that ovulation occurs. ■ 2. Week that menstruation occurs. ■ 3. First week after menstruation. ■ 4. Week before menstruation occurs. 29. During the admission workup for a modifi ed radical mastectomy, the client is extremely anxious and asks many questions. Which of the following approaches would offer the best guide for the nurse to answer questions raised by this apprehensive preoperative client? ■ 1. Tell the client as much as she wants to know and is able to understand. ■ 2. Delay discussing the client’s questions with her until she is convalescing. ■ 3. Delay discussing the client’s questions with her until her apprehension subsides. ■ 4. Explain to the client that she should discuss her questions fi rst with the physician. 30. A client asks the nurse, “Where is cancer usually found in the breast?” When responding to the client, the nurse uses a diagram of a left breast and indicates that most malignant tumors occur in which quadrant of the breast? ■ 1. Upper outer quadrant. ■ 2. Upper inner quadrant. ■ 3. Lower outer quadrant. ■ 4. Lower inner quadrant. 31. Atropine sulfate is included in the preoperative orders for a client undergoing a modifi ed radical mastectomy. The expected outcome is to: ■ 1. promote general muscular relaxation. ■ 2. decrease pulse and respiratory rates. ■ 3. decrease nausea. ■ 4. inhibit oral and respiratory secretions. 32. During the postoperative period after a modifi ed radical mastectomy, the client confi des in the nurse that she thinks she got breast cancer because she had an abortion and she did not tell her husband. The best response by the nurse is which of the following? ■ 1. “Cancer is not a punishment; it is a disease.” ■ 2. “You might feel better if you confi ded in your husband.” ■ 3. “Tell me more about your feelings on this.” ■ 4. “I can have the social worker talk to you if you would like.” 33. Postoperatively after a modifi ed radical mastectomy, a client has an incisional drainage tube attached to Hemovac suction. The nurse determines the suction is effective when: ■ 1. The intrathoracic pressure is decreased and the client breathes easier. ■ 2. There is an increased collateral lymphatic fl ow toward the operative area. ■ 3. Accumulated serum and blood in the operative area are removed. ■ 4. No adhesions are formed between the skin and chest wall in the operative area. 34. Which of the following positions would be best for a client’s right arm when she returns to her room after a right modifi ed radical mastectomy with multiple lymph node excisions? ■ 1. Across her chest wall. ■ 2. At her side at the same level as her body. ■ 3. In the position that affords her the greatest comfort without placing pressure on the incision. ■ 4. On pillows, with her hand higher than her elbow and her elbow higher than her shoulder. 35. The client with breast cancer is prescribed tamoxifen (Nolvadex) 20 mg daily. The client states she does not like taking medicine and asks the nurse if the tamoxifen is really worth taking. The nurse’s best response is which of the following? ■ 1. “This drug is part of your chemotherapy program.” ■ 2. “This drug has been found to decrease metastatic breast cancer.” ■ 3. “This drug will act as an estrogen in your breast tissue.” ■ 4. “This drug will prevent hot fl ashes since you cannot take hormone replacement.” 36. A client undergoing chemotherapy after a modifi ed radical mastectomy asks the nurse questions about a breast prosthesis and wigs. After answering the questions directly, the nurse should also: ■ 1. Provide a list of resources, including the local breast cancer support group. ■ 2. Offer a referral to the social worker. ■ 3. Call the home health care agency. ■ 4. Contact the plastic surgeon. 37. A client is to have radiation therapy after a modifi ed radical mastectomy. The nurse should teach the client to care for the skin at the site of therapy by: ■ 1. Washing the area with water. ■ 2. Exposing the area to dry heat. ■ 3. Applying an ointment to the area. ■ 4. Using talcum powder on the area. 38. The nurse should teach a client that a normal local tissue response to radiation is: ■ 1. Atrophy of the skin. ■ 2. Scattered pustule formation. ■ 3. Redness of the surface tissue. ■ 4. Sloughing of two layers of skin. 39. The nurse refers a client who had a mastectomy to “Reach to Recovery.” The primary purpose of the American Cancer Society’s Reach to Recovery program is to: ■ 1. Foster rehabilitation in women who have had mastectomies. ■ 2. Raise funds to support early breast cancer detection programs. ■ 3. Provide free dressings for women who have had radical mastectomies. ■ 4. Collect statistics for research from women who have had mastectomies. The Client with Benign Prostatic Hypertrophy 40. A 72-year-old male is in the emergency department because he has been unable to void for the past 12 hours. The best method for the nurse to use when assessing for bladder distention in a male client is to check for: ■ 1. A rounded swelling above the pubis. ■ 2. Dullness in the lower left quadrant. ■ 3. Rebound tenderness below the symphysis. ■ 4. Urine discharge from the urethral meatus. 41. During a client’s urinary bladder catheterization, the nurse ensures that the bladder is emptied gradually. The best rationale for the nurse’s action is that completely emptying an overdistended bladder at one time tends to cause: ■ 1. Renal failure. ■ 2. Abdominal cramping. ■ 3. Possible shock. ■ 4. Atrophy of bladder musculature. 42. The primary reason for lubricating the urinary catheter generously before inserting it into a male client is that this technique helps reduce: ■ 1. Spasms at the orifi ce of the bladder. ■ 2. Friction along the urethra when the catheter is being inserted. ■ 3. The number of organisms gaining entrance to the bladder. ■ 4. The formation of encrustations that may occur at the end of the catheter. 43. The primary reason for taping an indwelling catheter laterally to the thigh of a male client is to: ■ 1. Eliminate pressure at the penoscrotal angle. ■ 2. Prevent the catheter from kinking in the urethra. ■ 3. Prevent accidental catheter removal. ■ 4. Allow the client to turn without kinking the catheter. 44. Many older men with prostatic hypertrophy do not seek medical attention until urinary obstruction is almost complete. One reason for this delay in seeking attention is that these men may: ■ 1. Feel too self-conscious to seek help when reproductive organs are involved. ■ 2. Expect that it is normal to have to live with some urinary problems as they grow older. ■ 3. Fear that sexual indiscretions in earlier life may be the cause of their problem. ■ 4. Have little discomfort in relation to the amount of pathology because responses to pain stimuli fade with age. 45. When caring for a client with a history of benign prostatic hypertrophy (BPH), the nurse should do which of the following? Select all that apply. ■ 1. Provide privacy and time for the client to void. ■ 2. Monitor intake and output. ■ 3. Catheterize the client for post void residual urine. ■ 4. Ask the client if he has urinary retention. ■ 5. Test the urine for hematuria. 46. The nurse should specifi cally assess a client with prostatic hypertrophy for which of the following ? ■ 1. Voiding at less frequent intervals. ■ 2. Diffi culty starting the fl ow of urine. ■ 3. Painful urination. ■ 4. Increased force of the urine stream. 47. The nurse is reviewing the medication history of a client with benign prostatic hypertrophy (BPH). Which medication will likely aggravate BPH? ■ 1. Metformin (Glucophage). ■ 2. Buspirone (BuSpar). ■ 3. Inhaled ipratropium (Atrovent). ■ 4. Ophthalmic timolol (Timoptic). 48. A client is scheduled to undergo transurethral resection of the prostate. The procedure is to be done under spinal anesthesia. Postoperatively, the nurse should assess the client for: ■ 1. Seizures. ■ 2. Cardiac arrest. ■ 3. Renal shutdown. ■ 4. Respiratory paralysis. 49. A client with benign prostatic hypertrophy (BPH) is being treated with terazosin (Hytrin) 2 mg at bedtime. The nurse should monitor the client’s: ■ 1. Urine nitrites. ■ 2. White blood cell count. ■ 3. Blood pressure. ■ 4. Pulse. 50. A client underwent transurethral resection of the prostate (TURP), and a large three-way indwelling urinary catheter was inserted in the bladder with continuous bladder irrigation. In which of the following circumstances should the nurse increase the fl ow rate of the continuous bladder irrigation? ■ 1. When drainage is continuous but slow. ■ 2. When drainage appears cloudy and dark yellow. ■ 3. When drainage becomes bright red. ■ 4. When there is no drainage of urine and irrigating solution. 51. A client is to receive belladonna and opium suppositories, as needed, postoperatively after transurethral resection of the prostate (TURP). The nurse should give the client these drugs when he demonstrates signs of: ■ 1. A urinary tract infection. ■ 2. Urine retention. ■ 3. Frequent urination. ■ 4. Pain from bladder spasms. 52. A nursing assistant tells the nurse, “I think the client is confused. He keeps telling me he has to void, but that isn’t possible because he has a catheter in place that is draining well.” Which of the following responses would be most appropriate for the nurse to make? ■ 1. “His catheter is probably plugged. I’ll irrigate it in a few minutes.” ■ 2. “That’s a common complaint after prostate surgery. The client only imagines the urge to void.” ■ 3. “The urge to void is usually created by the large catheter, and he may be having some bladder spasms.” ■ 4. “I think he may be somewhat confused.” 53. A physician has ordered amoxicillin 100 P.O. BID (Ampicillin). The nurse should teach the client to: Select all that apply. ■ 1. Drink 2,500 mL of fl uids daily. ■ 2. Void frequently, at least every 2 to 3 hours. ■ 3. Take time to empty the bladder completely. ■ 4. Take the last dose of the antibiotic for the day at bedtime. ■ 5. Take the antibiotic with food. 54. In discussing home care with a client after transurethral resection of the prostate (TURP), the nurse should teach the male client that dribbling of urine: ■ 1. Can be a chronic problem. ■ 2. Can persist for several months. ■ 3. Is an abnormal sign that requires intervention. ■ 4. Is a sign of healing within the prostate. 55. A priority nursing diagnosis for the client who is being discharged to home 3 days after transurethral resection of the prostate (TURP) is: ■ 1. Defi cient fl uid volume. ■ 2. Imbalanced nutrition: Less than body requirements. ■ 3. Impaired tissue integrity. ■ 4. Ineffective airway clearance. 56. A client with benign prostatic hypertrophy (BPH) has an elevated prostate-specifi c antigen (PSA) level. The nurse should? ■ 1. Instruct the client to have a colonoscopy before coming to conclusions about the PSA results. ■ 2. Instruct the client that a urologist will monitor the PSA level biannually when elevated. ■ 3. Determine if the prostatic palpation was done before or after the blood sample was drawn. ■ 4. Ask the client if he emptied his bladder before the blood sample was obtained. The Client with Testicular Disease 98. A 28-year-old male is diagnosed with acute epididymitis. The nurse should assess the client for: ■ 1. Burning and pain on urination. ■ 2. Severe tenderness and swelling in the scrotum. ■ 3. Foul-smelling ejaculate. ■ 4. Foul-smelling urine. 99. A 20-year-old client is being treated for epididymitis. Teaching for this client should include the fact that epididymitis is commonly a result of a: ■ 1. Virus. ■ 2. Parasite. ■ 3. Sexually transmitted infection. ■ 4. Protozoon. 100. When teaching a client to perform testicular self-examination, the nurse explains that the examination should be performed: ■ 1. After intercourse. ■ 2. At the end of the day. ■ 3. After a warm bath or shower. ■ 4. After exercise. 101. The nurse is assessing a client’s testes. Which of the following fi ndings indicate the testes are normal? ■ 1. Soft. ■ 2. Egg-shaped. ■ 3. Spongy. ■ 4. Lumpy. 102. A client has a testicular nodule that is highly suspicious for testicular cancer. A laboratory test that supports this diagnosis is: ■ 1. Decreased alpha fetoprotein (AFP). ■ 2. Decreased beta–human chorionic gonadotropin (hCG). ■ 3. Increased testosterone. ■ 4. Increased AFP. 103. Although the cause of testicular cancer is unknown, it is associated with a history of: ■ 1. Undescended testes. ■ 2. Sexual relations at an early age. ■ 3. Seminal vesiculitis. ■ 4. Epididymitis. 104. Risk factors associated with testicular malignancies include: ■ 1. African-American race. ■ 2. Residing in a rural area. ■ 3. Lower socioeconomic status. ■ 4. Age older than 40 years. 105. A client with a testicular malignancy undergoes a radical orchiectomy. In the immediate postoperative period the nurse should particularly assess the client for: ■ 1. Bladder spasms. ■ 2. Urine output. ■ 3. Pain. ■ 4. Nausea. 106. A right orchiectomy is performed on a client with a testicular malignancy. The client expresses concerns regarding his sexuality. The nurse should base the response on the knowledge that the client: ■ 1. Is not a candidate for sperm banking. ■ 2. Should retain normal sexual drive and function. ■ 3. Will be impotent. ■ 4. Will have a change in secondary sexual characteristics. 107. A client diagnosed with seminomatous testicular cancer expresses fear and questions the nurse about his prognosis. The nurse should base the response on the knowledge that: ■ 1. Testicular cancer is almost always fatal. ■ 2. Testicular cancer has a cure rate of 90% when diagnosed early. ■ 3. Surgery is the treatment of choice for testicular cancer. ■ 4. Testicular cancer has a 50% cure rate when diagnosed early. The Client with Cancer of the Prostate 108. The nurse is developing a program about prostate cancer for a health fair. The nurse should provide information about which of the following topics? ■ 1. The Prostate-Specifi c Antigen (PSA) test is reliable for detecting the presence of prostate cancer. ■ 2. For all men, age 50 and older, the American Cancer Society recommends an annual rectal examination. ■ 3. Avoid lifting more than 20 lb aids in prevention of prostate cancer. ■ 4. Regular sexual activity promotes health of the prostate gland to prevent cancer. 109. The nurse is caring for a client who will have a bilateral orchiectomy. The client asks what is involved with this procedure. The nurse’s most appropriate response would be? “The surgery: ■ 1. Removes the entire prostate gland, prostatic capsule, and seminal vesicles.” ■ 2. Tends to cause urinary incontinence and impotence.” ■ 3. Freezes prostate tissue, killing cells.” ■ 4. Results in reduction of the major circulating androgen, testosterone.” 110. The nurse is teaching a client newly diagnosed with prostate cancer. Which of the following points should be included in the instruction? Select all that apply. ■ 1. Prostate cancer is usually multifocal and slow-growing. ■ 2. Most prostate cancers are adenocarcinoma. ■ 3. The incidence of prostate cancer is higher in African American men, and the onset is earlier. ■ 4. A prostate specifi c antigen (PSA) lab test greater than 4 ng/mg will need to be monitored. ■ 5. Cancer cells are detectable in the urine. 111. When a client is receiving hormone replacement for prostate cancer, the nurse should do which of the following? Select all that apply. ■ 1. Inform the client that increased libido is expected with hormone therapy. ■ 2. Reassure the client and his signifi cant other that erectile dysfunction will not occur as a consequence of hormone therapy. ■ 3. Provide the client the opportunity to communicate concerns and needs. ■ 4. Utilize communication strategies that enable the client to gain some feeling of control. ■ 5. Suggest that an appointment be made to see a psychiatrist. 112. A client asks the nurse why the prostate specifi c antigen (PSA) level is determined before the digital rectal examination. The nurse’s best response is which of the following? ■ 1. “It is easier for the client.” ■ 2. “A prostate examination can possibly decrease the PSA.” ■ 3. “A prostate examination can possibly increase the PSA.” ■ 4. “If the PSA is normal, the client will not have to undergo the rectal examination.” 113. The nurse is performing a digital rectal examination. Which of the following fi nding is a key sign for prostate cancer? ■ 1. A hard prostate, localized or diffuse. ■ 2. Abdominal pain. ■ 3. A boggy, tender prostate. ■ 4. A nonindurated prostate. 114. A client is undergoing a total prostatectomy for prostate cancer. The client asks questions about his sexual function. The best response by the nurse is which of the following? ■ 1. “Loss of the prostate gland means that you will be impotent.” ■ 2. “Loss of the prostate gland means that you will be infertile and there will be no ejaculation. You can still experience the sensations of orgasm.” ■ 3. “Loss of the prostate gland means that you will have no loss of sexual function and drive.” ■ 4. “Loss of the prostate gland means that your erectile capability will return immediately after surgery.” 115. A 65-year-old client has been told by the physician that his prostate cancer was graded at stage IIB. The client inquires if this means he is going to die soon. The best response by the nurse is which of the following? ■ 1. “Prostate cancer at this stage is very slow growing.” ■ 2. “Prostate cancer at this stage is very fast growing.” ■ 3. “Prostate cancer at this stage has spread to the bone.” ■ 4. “Prostate cancer at this stage is diffi cult to predict.” 116. A client with prostate cancer is treated with hormone therapy consisting of diethylstilbestrol (DES; Stilphostrol), 2 mg daily. The nurse should instruct the client to expect to have: ■ 1. Tenderness of the scrotum. ■ 2. Tenderness of the breasts. ■ 3. Loss of pubic hair. ■ 4. Decreased blood pressure. Answers The Client with Breast Disease 23. 1. This complaint warrants the nurse’s performing an examination and reporting the results to the physician. Hormone fl uctuations do cause breast discomfort, but an examination must be done at this time to assess the breast. Although pain is not common with breast cancer, it can be a symptom. Teaching the client to perform BSE is important, but it is not the priority action in this case. CN: Physiological adaptation; CL: Synthesize 24. 3. It is generally recommended that the breasts be examined during the fi rst week after menstruation. During this time, the breasts are least likely to be tender or swollen because estrogen is at its lowest level. Therefore, the examination will be more comfortable for the client. The examination may also be more accurate because the client is more likely to notice an actual change in her breast that is not simply related to hormonal changes. CN: Health promotion and maintenance; CL: Apply 25. 2. The client needs to become more confi dent and knowledgeable about the normal feel of the implants and her breast tissue. The best technique is for the nurse to demonstrate breast self-examination (BSE) to the client as the nurse conducts the clinical breast examination. Implant surgery does not exclude the need for monthly BSE. A mammogram is not a substitute for monthly BSE. CN: Health promotion and maintenance; CL: Synthesize 26. 2. The breasts may vary in size before menstruation because of breast engorgement caused by hormonal changes. A woman may then note that her bra fi ts more tightly than usual. Benign cysts do not cause variation in breast size. A change in breast size that does not follow hormonal changes could warrant further assessment. The breasts normally are about the same size, although some women have one breast slightly larger than the other. CN: Health promotion and maintenance; CL: Apply 27. 2. Advancing age in postmenopausal women has been identifi ed as a risk factor for breast cancer. A 76-year-old client needs monthly breast selfexamination and a yearly clinical breast examination and mammogram to comply with the screening schedule. While mammograms are less painful as breast tissue becomes softer, the nurse should advise the woman to have the mammogram. Family history is important, but only about 5% of breast cancers are genetic. CN: Health promotion and maintenance; CL: Synthesize 28. 1. If a client has questions the nurse cannot answer, it is best to delay the signing of the consent until the questions are clarifi ed for the client. The surgeon should be notifi ed, and the appropriate information or collaboration should be provided for the client before she signs the surgical consent. Telling her she should concentrate on recovery fi rst ignores the client’s questions and concerns. Frequently the plastic surgeon needs to be consulted at the beginning of the treatment because various surgical decisions depend on the future plans for breast reconstruction. CN: Management of care; CL: Synthesize 29. 1. An important nursing responsibility is preoperative teaching, and the most frequently recommended guide for teaching is to tell the client as much as she wants to know and is able to understand. Delaying discussion of issues about which the client has concerns is likely to aggravate the situation and cause the client to feel distrust. As a general guide, the client would not ask the question if she were not ready to discuss her situation. The nurse is available to answer the client’s questions and concerns and should not delay discussing these with the client. CN: Psychosocial adaptation; CL: Synthesize 30. 1. About half of malignant breast tumors occur in the upper outer quadrant of the breast. For no known reason, cancer appears in the left breast more often than in the right breast. The upper outer quadrants of the breast, and especially the axillary area, should be covered thoroughly in the clinical breast examination and breast self-examination. CN: Physiological adaptation; CL: Apply 31. 4. Atropine sulfate, a cholinergic blocking agent, is given preoperatively to reduce secretions in the mouth and respiratory tract, which assists in maintaining the integrity of the respiratory system during general anesthesia. Atropine is not used to promote muscle relaxation, decrease nausea and vomiting, or decrease pulse and respiratory rates. It causes the pulse to increase. CN: Pharmacological and parenteral therapies; CL: Evaluate 32. 3. The nurse should respond with an openended statement that elicits further exploration of the client’s feelings. Women with cancer may feel guilt or shame. Previous life decisions, sexuality, and religious beliefs may infl uence a client’s adjustment to a diagnosis of cancer. The nurse should not contradict the client’s feelings of punishment or offer advice such as confi ding in the husband. A social worker referral may be benefi cial in the future, but is not the fi rst response needed to elicit exploration of the client’s feelings. CN: Psychosocial adaptation; CL: Synthesize 33. 3. A drainage tube is placed in the wound after a modifi ed radical mastectomy to help remove accumulated blood and fl uid in the area. Removal of the drainage fl uids assists in wound healing and is intended to decrease the incidence of hematoma, abscess formation, and infection. Drainage tubes placed in a wound do not decrease intrathoracic pressure, increase collateral lymphatic fl ow, or prevent adhesion formation. CN: Reduction of risk potential; CL: Evaluate 34. 4. Lymph nodes can be removed from the axillary area when a modifi ed radical mastectomy is done, and each of the nodes is biopsied. To facilitate drainage from the arm on the affected side, the client’s arm should be elevated on pillows with her hand higher than her elbow and her elbow higher than her shoulder. A sentinel node biopsy procedure is associated with a decreased risk of lymphedema because fewer nodes are excised. CN: Physiological adaptation; CL: Synthesize 35. 2. Tamoxifen is an antiestrogen drug that has been found to be effective against metastatic breast cancer and to improve the survival rate. The drug causes hot fl ashes as an adverse effect. CN: Pharmacological and parenteral therapies; CL: Synthesize 36. 1. Giving the client a list of community resources that could provide support and guidance assists the client to maintain her self-image and independence. The support group will include other women who have undergone similar therapies and can offer suggestions for breast products and wigs. Because the client is asking about specifi c resources, she does not need a referral to a social worker, home health agency, or plastic surgeon. CN: Management of care; CL: Synthesize 37. 1. A client receiving radiation therapy should avoid lotions, ointments, and anything that may cause irritation to the skin, such as exposure to sunlight, heat, or talcum powder. The area may safely be washed with water if it is done gently and if care is taken not to injure the skin. CN: Reduction of risk potential; CL: Synthesize 38. 3. The most common reaction of the skin to radiation therapy is redness of the surface tissues. Dryness, tanning, and capillary dilation are also common. Atrophy of the skin, pustules, and sloughing of two layers would not be expected and should be reported to the radiologist. CN: Reduction of risk potential; CL: Apply 39. 1. The American Cancer Society’s Reach to Recovery is a rehabilitation program for women who have had breast surgery. It is designed to meet their physical, psychological, and emotional needs. The Reach to Recovery program is implemented by women who have had breast cancer themselves. Many women benefi t from this peer information and support. CN: Psychosocial adaptation; CL: Apply The Client with Benign Prostatic Hypertrophy 40. 1. The best way to assess for a distended bladder in either a male or female client is to check for a rounded swelling above the pubis. This swelling represents the distended bladder rising above the pubis into the abdominal cavity. Dullness does not indicate a distended bladder. The client might experience tenderness or pressure above the symphysis. No urine discharge is expected; the urine fl ow is blocked by the enlarged prostate. CN: Reduction of risk potential; CL: Analyze 41. 3. Rapid emptying of an overdistended bladder may cause hypotension and shock due to the sudden change of pressure within the abdominal viscera. Previously, removing no more than 1,000 mL at one time was the standard of practice, but this is no longer thought to be necessary as long as the overdistended bladder is emptied slowly. CN: Reduction of risk potential; CL: Apply 42. 2. Liberal lubrication of the catheter before catheterization of a male reduces friction along the urethra and irritation and trauma to urethral tissues. Because the male urethra is tortuous, a liberal amount of lubrication is advised to ease catheter passage. The female urethra is not tortuous, and, although the catheter should be lubricated before insertion, less lubricant is necessary. Lubrication of the catheter will not decrease spasms. The nurse should use sterile technique to prevent introducing organisms. Crusts will not form immediately. Irrigating the catheter as needed will prevent clot and crust formation. CN: Reduction of risk potential; CL: Apply 43. 1. The primary reason for taping an indwelling catheter to a male client so that the penis is held in a lateral position is to prevent pressure at the penoscrotal angle. Prolonged pressure at the penoscrotal angle can cause a ureterocutaneous fi stula. CN: Reduction of risk potential; CL: Apply 44. 2. Research shows that older men tend to believe it is normal to live with some urinary problems. As a result, these men often overlook symptoms and simply attribute them to aging. As part of preventive care for men older than age 40, the yearly physical examination should include palpation of the prostate via rectal examination. Prostatespecifi c antigen screening also is done annually to determine elevations or increasing trends in elevations. The nurse should teach male clients the value of early detection and adequate follow-up for the prostate. CN: Reduction of risk potential; CL: Apply 45. 1, 2, 4, 5. Because of the history of benign prostatic hypertrophy (BPH), the nurse should provide privacy and time for the client to void. The nurse should also monitor intake and output, assess the client for urinary retention, and test the urine for hematuria. It is not necessary to catheterize the client. CN: Physiological adaptation; CL: Synthesize 46. 2. Signs and symptoms of prostatic hypertrophy include diffi culty starting the fl ow of urine, urinary frequency and hesitancy, decreased force of the urine stream, interruptions in the urine stream when voiding, and nocturia. The prostate gland surrounds the urethra, and these symptoms are all attributed to obstruction of the urethra resulting from prostatic hypertrophy. Nocturia from incomplete emptying of the bladder is common. Straining and urine retention are usually the symptoms that prompt the client to seek care. Painful urination is generally not a symptom of prostatic hypertrophy. CN: Physiological adaptation; CL: Analyze 47. 3. Ipratropium is a bronchodilator, and its anticholinergic effects can aggravate urine retention. Metformin and buspirone do not affect the urinary system; timolol does not have a systemic effect. CN: Pharmacological and parenteral therapies; CL: Apply 48. 4. If paralysis of vasomotor nerves in the upper spinal cord occurs when spinal anesthesia is used, the client is likely to develop respiratory paralysis. Artifi cial ventilation is required until the effects of the anesthesia subside. Seizures, cardiac arrest, and renal shutdown are not likely results of spinal anesthesia. CN: Physiological adaptation; CL: Analyze 49. 3. Terazosin is an antihypertensive drug that is also used in the treatment of BPH. Blood pressure must be monitored to ensure that the client does not develop hypotension, syncope, or orthostatic hypotension. The client should be instructed to change positions slowly. Urine nitrates, white blood cell count, and pulse rate are not affected by terazosin. CN: Pharmacological and parenteral therapies; CL: Analyze 50. 3. The decision by the surgeon to insert a catheter after TURP or prostatectomy depends on the amount of bleeding that is expected after the procedure. During continuous bladder irrigation after a TURP or prostatectomy, the rate at which the solution enters the bladder should be increased when the drainage becomes brighter red. The color indicates the presence of blood. Increasing the fl ow of irrigating solution helps fl ush the catheter well so that clots do not plug it. There would be no reason to increase the fl ow rate when the return is continuous or when the return appears cloudy and dark yellow. Increasing the fl ow would be contraindicated when there is no return of urine and irrigating solution. CN: Pharmacological and parenteral therapies; CL: Synthesize 51. 4. Belladonna and opium suppositories are prescribed and administered to reduce bladder spasms that cause pain after TURP. Bladder spasms frequently accompany urologic procedures. Antispasmodics offer relief by eliminating or reducing spasms. Antimicrobial drugs are used to treat an infection. Belladonna and opium do not relieve urine retention or urinary frequency. CN: Pharmacological and parenteral therapies; CL: Synthesize 52. 3. The indwelling urinary catheter creates the urge to void and can also cause bladder spasms. The nurse should ensure adequate bladder emptying by monitoring urine output and characteristics. Urine output should be at least 50 mL/hour. A plugged catheter, imagining the urge to void, and confusion are less likely reasons for the client’s complaint. CN: Reduction of risk potential; CL: Synthesize 53. 1, 2, 3, 4. Ampicillin may be given with or without food, but the nurse should instruct the client to obtain an adequate fl uid intake (2,500 mL) to promote urinary output and to fl ush out bacteria from the urinary tract. The nurse should also encourage the client to void frequently (every 2 to 3 hours) and empty the bladder completely. Taking the antibiotic at bedtime, after emptying the bladder, helps to ensure an adequate concentration of the drug during the overnight period. CN: Physiological adaptation; CL: Synthesize 54. 2. Dribbling of urine can occur for several months after TURP. The client should be informed that this is expected and is not an abnormal sign. The nurse should teach the client perineal exercises to strengthen sphincter tone. The client may need to use pads for temporary incontinence. The client few months and will not be a chronic problem. Dribbling is not a sign of healing, but is related to the trauma of surgery. CN: Basic care and comfort; CL: Synthesize 55. 1. Defi cient fl uid volume is a priority diagnosis because the client needs to drink a large amount of fl uids to keep the urine clear. The urine should be almost without color. About 2 weeks after TURP, when desiccated tissue is sloughed out, a secondary hemorrhage could occur. The client should be instructed to call the surgeon or go to the emergency department if at any time the urine turns bright red. The client is not specifi cally at risk for nutritional problems after TURP. The client is not specifi cally at risk for impaired tissue integrity because there is no external incision, and the client is not specifi cally at risk for airway problems because the procedure is done under spinal anesthesia. CN: Basic care and comfort; CL: Analyze 56. 3. Rectal and prostate examinations can increase serum PSA levels; therefore, instruct the client that a manual rectal examination is usually part of the test regimen to determine prostate changes. The prostatic palpation should be done after the blood sample is drawn. The PSA level must be monitored more often than biannually when it is elevated. Having a colonoscopy is not related to the fi ndings of the PSA test. It is not necessary to void prior to having PSA blood levels tested. CN: Health promotion and maintenance; CL: Synthesize The Client with Testicular Disease 98. 2. Epididymitis causes acute tenderness and pronounced swelling of the scrotum. Gradual onset of unilateral scrotal pain, urethral discharge, and fever are other key signs. Epididymitis is occasionally, but not routinely, associated with urinary tract infection. Burning and pain on urination and foulsmelling ejaculate or urine are not classic symptoms of epididymitis. CN: Physiological adaptation; CL: Analyze 99. 3. Among men younger than age 35, epididymitis is most frequently caused by a sexually transmitted infection. Causative organisms are usually chlamydia or Neisseria gonorrhoeae. The other major form of epididymitis is bacterial, caused by the Escherichia coli or Pseudomonas organisms. The nurse should always include safe sex teaching for a client with epididymitis. The client should also be is a mode of transmission of gram-negative rods to the epididymis. CN: Reduction of risk potential; CL: Apply 100. 3. After a warm bath or shower, the testes hang lower and are both relaxed and in the ideal position for manual evaluation and palpation. CN: Health promotion and maintenance; CL: Apply 101. 2. Normal testes feel smooth, egg-shaped, and fi rm to the touch, without lumps. The surface should feel smooth and rubbery. The testes should not be soft or spongy to the touch. Testicular malignancies are usually nontender, nonpainful hard lumps. Lumps, swelling, nodules, or signs of infl ammation should be reported to the physician. CN: Health promotion and maintenance; CL: Analyze 102. 4. AFP and hCG are considered markers that indicate the presence of testicular disease. Elevated AFP and hCG and decreased testosterone are markers for testicular disease. Measurements of AFP, hCG, and testosterone are also obtained throughout the course of therapy to help measure the effectiveness of treatment. CN: Physiological adaptation; CL: Apply 103. 1. Cryptorchidism (undescended testes) carries a greatly increased risk for testicular cancer. Undescended testes occurs in about 3% of male infants, with an increased incidence in premature infants. Other possible causes of malignancy include chemical carcinogens, trauma, orchitis, and environmental factors. Testicular cancer is not associated with early sexual relations in men, even though cervical cancer is associated with early sexual relations in women. Testicular cancer is not associated with seminal vesiculitis or epididymitis. CN: Health promotion and maintenance; CL: Apply 104. 2. The incidence of testicular cancer is higher in men who live in rural rather than suburban areas. Testicular cancer is more common in white than black men. Men with higher socioeconomic status seem to have a greater incidence of testicular cancer. The exact cause of testicular cancer is unknown. Cancer of the testes is the leading cause of death from cancer in the 15- to 35-year-old agegroup. CN: Health promotion and maintenance; CL: Analyze 105. 3. Because of the location of the incision in the high inguinal area, pain is a major problem during the immediate postoperative period. The incisional area and discomfort caused by movement contribute to increased pain. Bladder spasms and elimination problems are more commonly associated with prostate surgery. Nausea is not a priority problem. CN: Physiological adaptation; CL: Synthesize 106. 2. Unilateral orchiectomy alone does not result in impotence if the other testis is normal. The other testis should produce enough testosterone to maintain normal sexual drive, functioning, and characteristics. Sperm banking before treatment is commonly recommended because radiation or chemotherapy can affect fertility. CN: Psychosocial adaptation; CL: Synthesize 107. 2. When diagnosed early and treated aggressively, testicular cancer has a cure rate of about 90%. Treatment of testicular cancer is based on tumor type, and seminoma cancer has the best prognosis. Modes of treatment include combinations of orchiectomy, radiation therapy, and chemotherapy. The chemotherapeutic regimen used currently is responsible for the successful treatment of testicular cancer. CN: Physiological adaptation; CL: Apply The Client with Cancer of the Prostate 108. 2. Most prostate cancer is adenocarcinoma and is palpable on rectal examination because it arises from the posterior portion of the gland. Although the PSA is not a perfect screening test, the American Cancer Society recommends an annual rectal examination and blood PSA level for all men age 50 and older, or starting at age 40 if African American or if there is family history of prostate cancer. To help achieve optimal sexual function, give the client the opportunity to communicate his concerns and sexual needs. Regular sexual activity does not prevent cancer. CN: Health promotion and maintenance; CL: Synthesize 109. 4. Bilateral orchiectomy (removal of testes) results in reduction of the major circulating androgen, testosterone, as a palliative measure to reduce symptoms and progression of prostate cancer. A radical prostatectomy (removal of entire prostate gland, prostatic capsule, and seminal vesicles) may include pelvic lymphadenectomy. Complications include urinary incontinence, impotence, and rectal injury with the radical prostatectomy. Cryosurgery freezes prostate tissue, killing tumor cells without prostatectomy. CN: Health promotion and maintenance; CL: Apply 110. 1, 2, 3, 4. Cancer of the prostate gland is the second-leading cause of cancer death among American men and is the most common carcinoma in men older than age 65. Incidence of prostate cancer is higher in African American men, and onset is earlier. Most prostate cancers are adenocarcinoma. Prostate cancer is usually multifocal, slow-growing, and can spread by local extension, by lymphatics, or through the bloodstream. Prostate-specifi c antigen (PSA) greater than 4 ng/mg is diagnostic; a free PSA level can help stratify the risk of elevated PSA levels. Metastatic workup may include skeletal x-ray, bone scan, and CT or MRI to detect local extension, bone, and lymph node involvement. The urine does not have prostate cancer cells. CN: Health promotion and maintenance; CL: Create 111. 3, 4. Hormone manipulation deprives tumor cells of androgens or their by-products and, thereby, alleviates symptoms and retards disease progression. Complications of hormonal manipulation include: hot fl ashes, nausea and vomiting, gynecomastia, and sexual dysfunction. As part of supportive care, provide explanations of diagnostic tests and treatment options and help the client gain some feeling of control over his disease and decisions related to it. To help achieve optimal sexual function, give the client the opportunity to communicate his concerns and sexual needs. Inform the client that decreased libido is expected after hormonal manipulation therapy, and that impotence may result from some surgical procedures and radiation. A psychiatrist is not needed. CN: Psychosocial adaptation; CL: Synthesize 112. 3. Manipulation of the prostate during the digital rectal examination may falsely increase the PSA levels. The PSA determination and the digital rectal examination are both necessary as screening tools for prostate cancer, and both are recommended for all men older than age 50. Prostate cancer is the most common cancer in men and the second leading killer from cancer among men in the United States. Incidence increases sharply with age, and the disease is predominant in the 60- to 70-year-old age-group. CN: Health promotion and maintenance; CL: Apply 113. 1. On digital rectal examination, key signs of prostate cancer are a hard prostate, induration of the prostate, and an irregular, hard nodule. Accompanying symptoms of prostate cancer can include constipation, weight loss, and lymphadenopathy. Abdominal pain usually does not accompany prostate cancer. A boggy, tender prostate is found with infection (e.g., acute or chronic prostatitis). CN: Health promotion and maintenance; CL: Analyze 114. 2. Loss of the prostate gland interrupts the fl ow of semen, so there will be no ejaculation fl uid. The sensations of orgasm remain intact. The client needs to be advised that return of erectile capability is often disrupted after surgery, but within 1 year 95% of men have returned to normal erectile function with sexual intercourse. CN: Physiological adaptation; CL: Synthesize 115. 1. Clients who have stage IA or IIB prostate cancer have an excellent survival rate. Prostate cancer is usually slow growing, and many men who have prostate cancer do not die from it. A stage I or II tumor is confi ned to the prostate gland and has not spread to the extrapelvic region or bone. CN: Physiological adaptation; CL: Synthesize 116. 2. Diethylstilbestrol causes engorgement and tenderness of the breasts (gynecomastia). Stilbestrol is prescribed as palliative therapy for men with androgen-dependent prostatic carcinoma. An increase in blood pressure can occur. Tenderness of the scrotum and dramatic changes in secondary sexual characteristics should not occur. CN: Pharmacological and parenteral therapies; CL: Apply