The Immune System - APBio10-11
advertisement

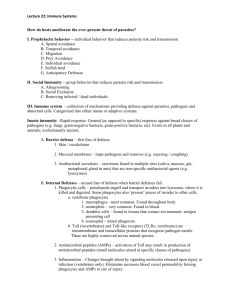
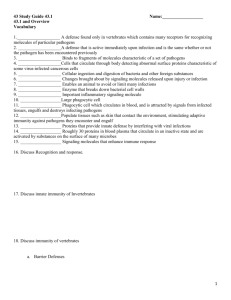
THE IMMUNE SYSTEM OVERVIEW: RECONNAISSANCE, RECOGNITION AND RESPONSE Pathogens: infectious agents that cause disease o An animal’s body offers nutrients, protection for growth and means of transportation Immune system: defense that allow an animal to avoid/limit infections Innate immunity: found in all animals o Responses are active immediately upon infection and are the same whether or not the pathogen has been encountered previously o Includes barrier defenses (skin), defenses that combat pathogens after they enter the body Acquired immunity: adaptive immunity o Active after innate immune defenses take effect, develop more slowly o Synthesis of proteins that inactive bacterial toxin, targeted killing of a virally infected body cell 43.1: INNATE IMMUNITY: RECOGNITION AND RESPONSE RELY ON SHARED TRAITS OF PATHOGENS INNATE IMMUNITY OF INVERTEBRATES Invertebrates rely only innate immunity o Insects rely on their exoskeleton as defense against infection Lysozyme: enzyme that digest microbial cell walls Low pH Hemocyte: immune cells that circulate within the hemolymph, carry out Phagocytosis: ingestion and digestion of bacteria and other foreign substances Trigger production of chemicals that kill microbes/entrap parasites Antimicrobial peptides: inactivate/kill fungi and bacteria by disrupting their plasma membranes o Insect immune cells secrete specialized recognition proteins, which bind to the macromolecules on invaders INNATE IMMUNITY OF VERTEBRATES BARRIER DEFENSES Mammals o Epithelial tissues block entry of pathogens – skin + mucous membranes lining the digestive, respiratory, urinary and reproductive tracts Mucus: viscous fluid that enhances defenses by trapping microbes Ciliated epithelial cells sweep mucus and microbes upward, preventing infection of lungs Saliva, ears, mucous secretions Saliva contains lysozyme CELLULAR INNATE DEFENSES Pathogens that get into the body encounter leukocytes (WBC) Toll-like receptor (TLR): recognizes fragments of molecules characteristic of a set of pathogens o Recognition triggers a series of defenses, starting with phagocytosis WBC engulfs the invading microbes, trapping them in a vacuole—fuses with a lysosome Neutrophils: most abundant phagocytic cells in the mammalian body; attracted by signals from infected tissues Macrophages: seen in spleen, lymph nodes; really large and can trap larger microbes Eosinophils: defend against multicellular invaders (parasitic worms); discharge destructive enzymes that damage invader Dendritic cells: populate tissues, stimulate development of acquired immunity against microbes ^The human lymphatic system Made up of the lymphatic vessels, adenoids, tonsils, lymph nodes, spleen, Peyer’s patches and appendix ANTIMICROBIAL PEPTIDES AND PROTEINS Interferons: proteins that provide innate defense against viral infections o Virus-infected body cells secrete interferons, inducing uninfected cells to produce substances that inhibit viral reproduction o Limit cell-to-cell spread of viruses, controlling viral infections like colds/flu Complement system: 30 proteins in blood plasma o Circulate in an inactive state and are activated by substances on the surface of microbes o Activation results in an influx of biochemical reactions leading to the lysis of invading cells o Inflammation INFLAMMATORY RESPONSES Inflammatory response: changes brought about by signaling molecules released upon injury Histamine: inflammatory signally molecule, stored in mast cells, connective tissues cells that store chemicals in granules fore secretion o Histamine released by mast cells @ sites of damage triggers blood vessels to dilate and become more permeable o Macrophages discharge additional signally molecules that promote blood flow to the injured site o Increase in local blood supply causes redness and heat of inflammation Cycles of signaling and response transform the infection site o Enhanced blood flow = antimicrobial proteins o Activated complement proteins = release of histamine and help attract phagocytes o Endothelial cells secrete signaling molecules = attract neutrophils and macrophages o Pus: fluid rich in white blood cells, dead microbes and cell debris Major damage may lead to a response that’s systemic (throughout the whole body) – increased production of WBC Fever: systemic inflammatory response o Pyrogens: released by macrophages, reset body’s thermostat to higher temp o Fevers accelerate tissue repair by speeding up chemical reactions? Septic shock: life-threatening condition: high fever, low blood flow, low BP NATURAL KILLER CELLS Natural Killer (NK) Cells: help recognize and eliminate certain diseased cells o Patrol body, attach to sick cells and release chemicals that lead to cell death INNATE IMMUNE SYSTEM EVASION BY PATHOGENS Pathogens have evolved in order to avoid destruction by phagocytic cells o Aren’t recognized by , prevent destruction, resistance to breakdown within lysosomes following phagocytosis (Tuberculosis) 43.2: ACQUIRED IMMUNITY: LYMPHOCYTE RECEPTORS PROVIDE PATHOGEN SPECIFIC RECOGNITION BUNCH OF VOCAB Lymphocyte: B cells and T cells, types of WBC, critical for acquired immune defense Thymus: an organ in the thoracic cavity above the heart that houses the T Cells B Cells: mature in the bone marrow B&T Cells recognize and inactivate foreign cells and molecules, contribute to Immunological memory: enhanced response to foreign molecule encountered previously o responsible for the protection we obtain against chicken pox o B&T cells only function in acquired immunity, but the two systems aren’t independent Signally molecules of phagocytic cells set the stage for acquired immunity Cytokines: proteins secreted by phagocytic cells that help recruit and activate lymphocytes ACQUIRED IMMUNITY: AN OVERVIEW “Each B cell or T cell has on its surface many receptor proteins that can bind to particular foreign molecule. The receptor proteins on a single lymphocyte are all the same, but there are millions of lymphocytes in the body that differ in the foreign molecules that their receptors recognize. When an animal is infected, B and T cells with receptors that can recognize the microbe are activated […] B and T cells interact with fragments of microbes displayed on the surface of cells. Activated lymphocytes undergo cell division […] Some T cells assist in activated other lymphocytes. Other T cells detect and kill infected host cells. Specialized B cells secrete soluble receptor proteins that attack foreign molecules and cells” (936). ANTIGEN RECOGNITION BY LYMPHOCYTES Antigen: a foreign molecule that is specifically recognized by lymphocytes and elicits a response o Most are large molecules, either proteins or polysaccharides o Some are toxins secreted by bacteria B and T cells recognize antigens using their antigen-specific receptors embedded in their plasma membranes A single B or T cell has about 100,000 antigen receptors on its surface o Sometimes B cells give rise to plasma cells that secrete a soluble form of the antigen receptor, the antibody or immunoglobulin (Ig). Epitope: antigenic determinant, a small accessible portion of an antigen All of the receptors on a single lymphocyte recognize the same epitope; each of the body’s lymphocytes displays specificity for a particular epitope ANTIGEN RECEPTORS OF B CELLS AND T CELLS B cell receptor for an antigen is a Y-shaped molecule consisting of four polypeptide chains o Two identical heavy chains o Two identical light chains o With two disulfide bridges linking the chains together o The light and heavy chains have a constant (C) region: amino acid sequences vary little among the receptors, includes the cytoplasmic tail and transmembrane region of the heavy chain and all the disulfide bridges o Variable (V) region: two tips of the Y shape, amino acid sequence varies from one B cell to the other o Antibodies have the same overall recognition as B cell receptors except they lack the transmembrane region and cytoplasmic tail T cell receptor: consists of two different polypeptide chains: a chain and b chain, linked by disulfide bridge o Have as many features as the B cell receptors o Tip of the molecule = V region: antigen binding site o Rest of the molecule = C region B cell receptors recognize and bind to an intact antigen whether it is free or bound to a pathogen ; T cell receptors bind only to antigen fragments that are displayed on the surface of host cells Major histocompatibility complex (MHC): genes in a group , produces a host cell protein that can present an antigen fragment to a T cell receptor THE ROLE OF THE MHC Antigen presentation: display of the antigen fragment on the cell surface o By MHC proteins either activates immune responses against the antigen or target destruction of the infected cell Class I MHC molecules: o found in almost all cells of the body o bind to peptide fragments of foreign antigens synthesized within cells o recognized by cytotoxic T cells (kill by toxic gene products) Class II MHC molecules: made by just a few cell types—dendritic cells, macrophages, B cells o bind to antigen fragments derived from foreign materials that have internalized through phagocytosis/endocytosis o antigen-presenting cells: dendritic cells, macrophages and B cells because of their key role in displaying internalized antigens o recognized by cytotoxic T cells and helper T cells: a group of T cells that assist both B cells and cytotoxic T cells LYMPHOCYTE DEVELOPMENT Major properties of acquired immune system o Diversity of receptors ensures that new pathogens are recognized as foreign o Ability to recognize vast numbers of foreign molecules coexist with a lack of reactivity against body’s own molecules o Response to antigen that has been encountered previously is stronger (immunological memory) GENERATION OF L YMPHOCYTE DIVERSITY BY GENE REARRANGEMENT Differences in amino acid sequences of V regions make antigen receptors extremely different Each person has 1 million + different B cells and 10 million + different T cells Understanding the origin of receptor diversity o Immunoglobulin (Ig) gene that encodes the light chain of secreted antibodies and membranebound B cell receptors Joins randomly selected V and J gene segments Undergoes transcription, splicing and translation ORIGIN OF SELF-TOLERANCE Lymphocytes mature in the bone marrow of thymus; tested for self-reactivity o The ones that try to destroy the body’s own cell are destroyed by apoptosis or rendered nonfunctional o Body lacks mature lymphocytes that react against its own components AMPLIFYING LYMPHOCYTES BY CLONAL SLECTION It is rare for an antigen to encounter a lymphocyte with a specific for that antigen; acquired immune response is effective because of the changes in cell number and behavior triggered by the binding of the antigen to the lymphocyte Binding of an antigen receptor o B cells or T cells amplify by dividing many times, forming two different types of clones Effector cells: short lived, attack antigen and any pathogens producing the antigen Memory cells: long lived, less numerous, bear receptors specific for the antigen o Clonal selection: proliferation of a lymphocyte into a clone of cells in response to binding an antigen The presentation of an antigen to specific receptors on a lymphocyte leads to repeated rounds of cell division Result? Clonal population of thousands of cells, specific to that antigen Primary immune response: first exposure to an antigen, peaks about 10-17 days after initial exposure o B cells generate plasma cells, antibody secreting effector cells o T cells activated to their effector forms (helper cells and cytotoxic cells) Secondary immune response: repeated exposure to the same antigen, faster response and of greater magnitude o Relies on the reservoir of T and B memory cells generated after the initial exposure Long-lived cells = provide immunological memory that can span many decades 43.3: ACQUIRED IMMUNITY DEFENDS AGAINST INFECTION OF BODY CELLS AND FLUIDS OVERVIEW Humoral immune response: activation and clonal selection of effector B cells- which secrete antibodies that circulate in the blood and lymph Cell-mediated immune response: activation and clonal selection of cytotoxic T cells- which identify and destroy target cells HELPER T CELLS: RESPONSE TO NEARLY ALL ANTIGENS Helper T cells are activated by encounters with antigen-presenting cells Cell proliferates after interacting with antigen fragments displayed by antigen-presenting cells Activated helper T cells secrete cytokines that stimulate activation of nearby B cells and cytotoxic T cells CD4: protein found on the surface of most helper T cells, binds to class II MHC molecule o Keep the helper T cell and antigen-presenting cell joined Dendritic cells are particularly important in triggering primary immune response o Serve as messengers, capture antigens, migrate to the lymphoid tissues CYTOTOXIC T CELLS: RESPONSE TO INFECTED CELLS Effector cells in cell-mediated immune response Require signaling from helper T cells to become active, as well as interaction with an anti-gen presenting cell CD8: protein found on most cytotoxic T cells, enhances interaction between target cell and T cell Destruction involves the secretion of proteins that cause cell rupture and cell death o Exposes pathogen to circulating antibodies Dendritic cell can present fragments from a wide variety of protein antigens, whereas B cells only present only to the antigen to which it binds ANTIBODY CLASSES Monoclonal antibodies: prepared from a single clone of B cells grown in culture – identical and specific for the same epitope on an antigen – useful for tagging specific molecules THE ROLE OF ANTIBODIES IN IMMUNITY Neutralization: antibodies bind to the surface proteins of a virus or bacterium, blocking the pathogen’s ability to infect a host cell Opsonization: antibodies bound to antigens present readily recognized structure for macrophages and increase phagocytosis Complement: proteins increase the effectiveness of antibody directed attacks on bacteria Membrane attack complex: forms a pore in the membrane of the foreign cell, water and ions rusin into the cell- lyses Phagocytosis: eating of pathogen PASSIVE AND ACTIVE IMMUNIZATION Active immunity: clones of memory cells form in response to an infection Passive immunity: antibodies provided by the mother guard against microbes, persists only for a short time Immunization: introduction of antigens into the body to develop active immunity o Vaccination: weakened forms of the pathogen to develop immunological memory IMMUNE REJECTION BLOOD GROUPS Type A blood would react with the type B antigen, shit would go down TISSUE AND ORGAN TRANSPLANTS MHC molecules stimulate immune response that leads to organ/tissue rejection 43.4: DISRUPTIONS IN IMMUNE SYSTEM FUNCTION CAN ELICIT OR EXACERBATE DISEASE EXAGGERATED, SELF-DIRECTED, AND DIMINISHED IMMUNE RESPONSES ALLERGIES Allergens: antigens that elicit an exaggerated response- mostly often involve IgE class antibodies Degranulation: interaction with the large pollen grains cross-links adjacent IgE molecules, inducing mast cell to release histamine Vascular changes: sneezes, runny noses, tearing eyes, difficulty breathing (antihistamines diminish allergy symptoms) Anaphylactic shock: develops when widespread mast cell degranulation triggers abrupt dilation of peripheral blood vessels, causing a precipitous drop in blood pressure (epinephrine, counters allergic responses) AUTOIMMUNE DISEASES Autoimmune disease: immune system turns against particular molecules of the body o Lupus: immune system generates antibodies against histones and DNA released by the normal breakdown of body cells o Rheumatoid arthritis: leads to painful inflammation of the cartilage and bone of joints o Type 1 diabetes mellitus: cytotoxic T cells destroy insulin-producing beta cells of the pancreas o Multiple sclerosis: T cells infiltrate central nervous system and destroy the myelin sheath that surrounds parts of many neurons EXERTION, STRESS, AND THE IMMUNE SYSTEM Stress weakens the immune system, so does exhaustive exercise Disrupt immune regulation by altering interplay of hormonal/nervous/immune system IMMUNODEFICIENCY DISEASES Immunodeficiency: disorder in which the ability of an immune system to protect against pathogens is defective/absent Inborn immunodeficiency: genetic/developmental defect in immune system Acquired immunodeficiency: develops later in life following exposure to chem/bio agents Acquired immunodeficiency syndrome /AIDS: caused by virus, shit happens ACQUIRED IMMUNE SYSTEM EVASION BY PATHOGENS ANTIGENIC VARIATION Pathogen alters how it appears to the immune system o Can reinfect/remain in host w/o triggering rapid response, trick memory cells o Antigenic variation: changes in epitope expression, regular events for some viruses (sleeping sickness, flu) LATENCY Largely inactive state, ceasing production of viral production targeted by lymphocytes (herpes, HIV from mother to baby) ATTACK ON THE I MMUNE SYSTEM: HIV HIV infects helper T cells, cells that have low CD4 (macrophages, brain cells) RNA genome is reverse-transcribed, product DNA is integrated into host cell’s genome Reasons why HIV thrives o Antigenic variation- mutates at high rate during replication o Latency- protected from antiviral agents used against HIV o Abolishes T cells, impairing both humoral and cell-mediated immune responses HIV sucks. Basically. CANCER AND IMMUNITY Cancer increases when immune response is impaired