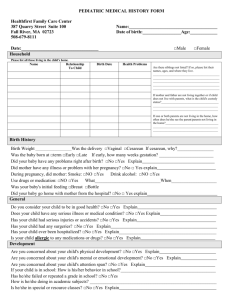
Messages for household members
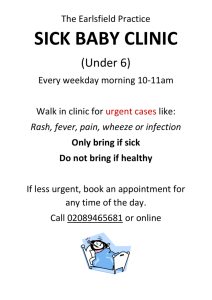
advertisement

Householder SMS + Audio messages (Updated Dec 2014) Pregnancy Month 2 Week No. 5 SMS Congratulations, there's a baby on the way! You can help the mother make sure her baby is healthy. Encourage her to visit the clinic often. Audio Message Notes to partners Congratulations! There is a baby on the way! There will be lots of things for the whole family to do. Fit the number to antenatal appointments to your country recommendations. Regular clinic visits in pregnancy help detect problems early and keep the mother and her baby safe. The mother will need at least four visits during her pregnancy. The staff at the clinic will check that the mother and her baby are growing well and that there are no problems. This message establishes to the guardian that they can play a meaningful part in the mother's pregnancy and encourages early access to antenatal services. You can help the mother and her baby stay safe and healthy. Find out where the nearest clinic is. Encourage the mother to speak to a health worker at the clinic about her pregnancy. If you can’t go with her, find someone who can. Make sure that the mother has a way of traveling there safely, too. It will be worth it for a healthy mother and baby. If you want to do one good thing for the baby this week, see that the mother goes to the clinic soon. A qualitative study in India highlighted the perception of pregnancy as a natural process that only warranted ANC when problems arose (Griffith & Stephenson 2001). This message explains that ANC is not only to treat complications BUT to detect them. References WHO: factsheets. http://www.who.int/mediacentre/factsheets/fs290/en/ WHO. Making pregnancy safer. http://www.who.int/making_pregnancy_safer/countries/soa.pdf DH. 2007. Maternity matters. London: Department of Health www.dh.gov.uk [pdf file, accessed September 2011] Lynn F, McNeill J, Alderdice F. 2010. Current trends in antenatal screening services: results from a regional survey. Ulster Med J 79(1):12-15 NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman. National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed September 2011] Report of the UNICEF/WHO Regional Consultation. 1999. Prevention and Control of Iron Deficiency Anaemia in Women and Children. Geneva, Switzerland Overview of 12 by 12 Initiative. WHO, UNICEF. Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. USAID. Counselling cards for maternal and neonatal health for community health workers WHO (2013). World Health Statistics 2013 http://www.who.int/gho/publications/world_health_statistics/2013/en/ Solarin & Black (2013). “They told me to come back”: Women’s Antenatal Care Booking Experience in Inner City Johannesburg. Matern Child Health J 17 Simkhada et al (2008) factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. Journal of Advanced Nursing 61 (3) http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2648.2007.04532.x/pdf “Free pills” can work as a motivator, but 2 6 Remind the mother to take iron and During her pregnancy, the mother will need iron and folic-acid only if iron and folic acid are freely folic-acid pills every day. She can get pills. These pills will help her to grow a strong, healthy baby. available in your area. them free at the clinic. A healthy mother grows a healthy baby. Encourage the mother to get these pills from the clinic. It is important to start taking these pills as early as possible in pregnancy. Stock-outs were a common challenge for iron supplementation (Maina-Gathigi L et al. 2013; WHO 2006) These pills are for free at the clinic. 20% of maternal deaths are due to maternal iron-deficiency anaemia and stunting in women. In India - 88% of pregnant and 74% of non-pregnant women are affected. In Africa - 50% of pregnant and 40% of non-pregnant women are anaemic. (The Lancet, 2006) Make sure she keeps a good stock of pills in the home. She can get more at the clinic before they run out. If the clinic is out of stock, see that she knows when to come back for more pills. The mother will need to take these pills every day. Suggest she takes them after dinner. If you want to do one good thing for the baby this week, get the mother some iron and folic-acid pills from the clinic. Anaemia is the most common nutritional deficiency disorder in the world. 20% of maternal deaths are due to maternal iron-deficiency, anemia and stunting in women. (The Lancet: Khan, 2006) References http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf Stoltzfus R.J. and Dreyfuss M.L. Guidelines for the Use of Iron Supplements to Prevent and Treat Iron Deficiency Anemia. International Nutritional Anemia Consultative Group (INACG) Essential Nutrition Actions - Improving Maternal-Newborn-Infant and Young Child Health and Nutrition. WHO. 2011 Weekly Iron-Folic Acid Supplementation (WIFS) in Women of Reproductive Age: Its Role in Promoting Optimal Maternal and Child Health. WHO. 2009. Report of the UNICEF/WHO Regional Consultation. 1999. Prevention and Control of Iron Deficiency Anaemia in Women and Children. Geneva, Switzerland Overview of 12 by 12 Initiative. WHO, UNICEF. USAID. Counselling cards for maternal and neonatal health for community health workers WHO.2001. Iron deficiency anaemia: Assessment, prevention and control, A guide for programme users. Essential Nutrition Actions - Improving Maternal-Newborn-Infant and Young Child Health and Nutrition. WHO. 2011 Weekly Iron-Folic Acid Supplementation (WIFS) in Women of Reproductive Age: Its Role in Promoting Optimal Maternal and Child Health. WHO. 2009. Khan, Wojdyla et al (2006). 'WHO analysis of the causes of maternal death: a systematic review', Lancet, 367:1066-74.http://www.who.int/mediacentre/factsheets/fs348/en/ Weekly Iron-Folic Acid Supplementation (WIFS) in Women of Reproductive Age: Its Role in Promoting Optimal Maternal and Child Health. WHO. 2009. USAID. Counselling cards for maternal and neonatal health for community health workers WHO, Micronutrient deficiencies. http://www.who.int/nutrition/topics/ida/en/ Department of Making Pregnancy Safer (2006) Iron and folate supplementation, Standards for Maternal and neonatal care http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/iron_folate_supplementation.pdf Maina-Gathigi L et al. (2013) Utilization of folic acid and iron supplementation services by pregnant women attending an antenatal clinic at a regional referral hospital in Kenya. Matern Child Health J. 2013 Sep;17(7):1236-42. doi: 10.1007/s10995-012-1120-x. http://www.ncbi.nlm.nih.gov/pubmed/22907273 Peña-Rosas JP et al. (2012) Effects and safety of preventive oral iron or iron + folic acid supplementation for women during pregnancy http://summaries.cochrane.org/CD004736/effects-and-safety-of-preventive-oral-iron-or-iron--folic-acid-supplementation-for-women-during-pregnancy#sthash.lFl3YQiu.dpuf Pick foods which are easily available in 2 7 Check the mother eats meat, beans, You can help the mother have a healthy pregnancy by making your area. fruits and vegetables daily. She needs sure she eats enough good food. iodised salt, too. Eating well will help her have a healthy baby. She will need several different sorts of food. First, make sure she has food that gives her energy, like rice, wheat and oats. Then check that she is having foods such as meat, fish and eggs which will help her baby grow. If the mother doesn’t eat meat, she will need lots of peas, beans, lentils and eggs. Some foods help the baby grow strong bones. Milk, yoghurt and soya, peas, leafy green vegetables and beans all help build Adapt to suit the local strategy for iodine deficiency prevention. Find out if salt is iodised. Pregnant women should have a minimum iodine intake of 250 µg and maximum of 500 µg a day. Lack of iodine causes brain damage and thyroid function disorders in babies. (WHO 2007) WHO recommends that mothers take calcium supplements to help prevent hypertension. Check whether strong bones. The mother will also need to eat plenty of fruit and vegetables. They are protective foods and will help the baby grow well. Citrus fruits like oranges and lemons will help her body absorb iron. Encourage her to have an extra mouthful of food with each meal, and some extra snacks if she is hungry. Growing a baby is hard work! Suggest the mother also uses iodised salt instead of regular salt. Iodine is good for the baby's brain. If you want to do one good thing for the baby this week, help the mother buy the food she needs to grow a healthy baby. supplements are available and adjust messages accordingly. Maternal undernutrition affects women’s chances of surviving pregnancy. Serious maternal undernutrition is common in subSaharan Africa, South Asia and SouthEast Asia, and is critical in Bangladesh, Eritrea and India. Maternal and child undernutrition is the single leading cause of health loss worldwide. (UNICEF, 2008; Blössner and de Onis, 2005.) References WHO (2014). Feto – maternal nutrition and low birth weight. http://www.who.int/nutrition/topics/feto_maternal/en/ [Accessed on 1 May 2014]Seumo, E.F. and Abdallah F. Nutritional Counseling for Pregnant Women in Tanzania. USAID, ACCESS. Black R.E. et al. Maternal and child undernutrition: global and regional exposures and health consequences.Lancet 2008; 371: 243-60 doi: 10.1016/S0140-6736(07)61690-0 pmid:18207566 FDA. Food Safety for Moms-to-Be- Educator’s Resource Guide. www.cfsan.fda.gov/pregnancy.html Fisher, J., Tran, T., Biggs, B., Tran, T., Dwyer, T., Casey, G., et al. (2011). Iodine Status in Late Pregnancy and Psychosocial determinants of iodized salt use in rural Viet Nam. Bulletin of World Health Organization , 813-820. Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ 1987; 65: 663–737 Kramer MS, Victora C. Low birth weight and perinatal mortality. In: Semba RD, Bloem MW, eds. Nutrition and health in developing countries. Humana Press, 2001 Langiano, E. 2011. Food safety at home: knowledge and practices of consumers. Journal of Public Health: 1-11. UNICEF. (2008, October 1). Nutrition: Micronutrients - Iodine, Iron and Vitamin A. Retrieved November 14, 2011, from UNICEF: http://www.unicef.org/nutrition/index_iodine.html USAID. Counselling cards for maternal and neonatal health for community health workers Victora CG et.al. Worldwide timing of growth faltering: Revisiting implications for interventions. Pediatrics 2010; 125:e473-e480. WHO/UNICEF. (2007). Reaching Optimal Iodine Nutrition in Pregnant and Lactating Women and Young Children. Geneva: World Health Organization. World Health Organization. (2011). Nutrition: Micronutrient Deficiencies. Retrieved November 14, 2011, from WHO: http://www.who.int/nutrition/topics/idd/en/ WHO. 2011. Background Paper 2 - A Review of health interventions with an effect on nutrition pdf, 1.51Mb UNICEF. (2008, October 1). Nutrition: Micronutrients - Iodine, Iron and Vitamin A. Retrieved November 14, 2011, from UNICEF: http://www.unicef.org/nutrition/index_iodine.html WHO/UNICEF. (2007). Reaching Optimal Iodine Nutrition in Pregnant and Lactating Women and Young Children. Geneva: World Health Organization. World Health Organization. (2011). Nutrition: Micronutrient Deficiencies. Retrieved November 14, 2011, from WHO: http://www.who.int/nutrition/topics/idd/en/ WHO. 2007. ' Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation', Public Health Nutrition, 10(12A): 1606-1611.; http://www.who.int/nutrition/publications/micronutrients/PHN10(12a).pdf 2 8 Reassure the mother that sickness It is time for the mother to go for her first check-up at the clinic. Long waiting times were found to be a barrier to ANC use (Simkhada et al. 2008) early in pregnancy is common. Ginger Help her plan to get there. or lemon tea may help soothe her stomach. Dry bread can help, too. Ask her to take some food and water to the clinic so she can eat something while waiting to be seen by the health worker. Maybe you or someone else can go with her if she wants company. Reassure the mother if she is feeling very sick and nauseous. This is very common at this stage and will get better in a few weeks. Between 70-80% of women will experience pregnancy sickness (Festin 2009; Matthews et al. 2010; NCCWCH 2008). It is not usually medically significant, but messages that reflect the woman's experience build trust in the SMS programme. Don’t let anyone give her traditional herbs or remedies to help with the sickness. They can be harmful to the mother and her baby. Tonics sold on market stalls may also be unsafe. There are other things you could suggest which will help: Encourage her to eat small amounts of food throughout the day. This will help her to keep up her strength. Persuade her to eat something, even if she does not feel like it. Small mouthfuls of food may help her stop being sick. She may find it easier to eat foods like dry biscuits, plain vegetables or bread. If she cannot eat, give her plenty of clean water to drink. If you want to do one good thing for the baby this week, make sure the mother goes to the clinic. References Chuang, Chao-Hua et al, 2006. “Herbal Medicines Used During the First Trimester and Major Congenital Malformations: An Analysis of Data from a Pregnancy Cohort Study”, Drug Safety, 29 (6): 537-548 (12). A A Opaneye, 1998. “Traditional medicine in Nigeria and modern obstetric practice: need for cooperation”, Central African Journal of Medicine, 44(10):258-61. Thein , Koh et al., 1995. “Risk factors for birth defects in Singapore: a case control study”. Annals, Academy of Medicine, Singapore. 24(3):421-7. USAID. Counselling cards for maternal and neonatal health for community health workers Blössner and de Onis,2005. “Malnutrition - Quantifying the health impact at national and local levels”, Environmental Burden of Disease Series, No. 12. WHO: Seumo, E.F. and Abdallah F. Nutritional Counseling for Pregnant Women in Tanzania. USAID, ACCESS. Black R.E. et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 2008; 371: 243-60 doi: 10.1016/S0140-6736(07)61690-0 pmid:18207566 WHO. 2011. Background Paper 2 - A Review of health interventions with an effect on nutrition pdf, 1.51Mb “Progress for Children - A Report Card on Maternal Mortality”. UNICEF, No. 7, September 2008. Victora CG et.al. Worldwide timing of growth faltering: Revisiting implications for interventions. Pediatrics 2010; 125:e473-e480. Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al., Maternal and Child Undernutrition Study Group, et al. Maternal and child undernutrition: global and regional exposures and health consequences.Lancet 2008; 371: 243-60 doi: 10.1016/S0140-6736(07)61690-0 pmid:18207566 Change to suit local malaria prevention 3 9 Mosquitoes cause illnesses like Mosquito bites can cause illnesses like malaria and dengue. strategy concerning IPT. malaria. Make sure the mother Pregnant women are more at risk of such illnesses. And they sleeps under an insecticide-treated get sicker when they do have an infection. bednet to prevent mosquito bites. You can help protect the mother and the baby from mosquitorelated illnesses like malaria and dengue. Encourage the mother to sleep under an insecticide-treated net every night. If it’s hot and stuffy, open the windows to let the air in. The net will keep her protected from mosquitoes. If there’s a hole in the net, stitch a small piece over it. Keep a spare net, just in case one gets damaged. Nearly one million deaths were caused by Malaria in 2008 globally - with pregnant women especially risk. (MCHIPUSAID; WHO, 2005) Over 2.5 billion people – over 40% of the world's population – are now at risk from dengue (WHO 2009). You can set an example by sleeping under one every night yourself! Check the area around the mother's home for stagnant water, rotting leaves or damp areas. Mosquitoes collect in these areas. Try to get rid of them or, if the area is small, pour old cooking oil on them. This will keep the mosquitoes away. Encourage the mother to wear long, light-coloured clothes as mosquitoes like dark colours. Suggest she uses an indoor spray and wears insect repellant as well. The mother may get some medicine to protect herself from malaria. If you want to do one good thing for the baby this week, make sure the mother uses an insecticide-treated net every night. References WHO (2013a). World Malaria Report http://www.who.int/malaria/media/world_malaria_report_2013/en/ WHO (2013b). Malaria in Pregnant Women http://www.who.int/malaria/areas/high_risk_groups/pregnancy/en/ Arogundade., E. D. et al. 2011. Relationship between care-givers' misconceptions and non-use of ITNs by under-five Nigerian children. [Online]. Available on: http://www.malariajournal.com/content/10/1/170 [Accessed on 29 January 2014] CDC. 2012. Intermittent Preventive Treatment of Malaria for Pregnant Women (IPTp). [Online]. Available on: http://www.cdc.gov/malaria/malaria_worldwide/reduction/iptp.html [Accessed on 29 January 2014] Doctors without borders., 2012. Malaria. [Online]. Available on: http://www.msf.org.uk/malaria [Accessed on 28 January 2014] East African Community., 2014. Malaria Prevention and Control. [Online]. Available on: http://www.eac.int/health/index.php?option=com_content&id=95%3Amalaria-prevention-andcontrol&Itemid=32 [Accessed on 29 January 2014] Isa AY and Nwobodo EL (2009) 'Awareness and utilization of insecticide-treated mosquito nets among pregnant mothers at a tertiary health institution in north-western Nigeria' Niger J Med. 2009 Apr-Jun;18(2):175-8. http://www.ncbi.nlm.nih.gov/pubmed/19630324 Falade et al. (2005/06). The influence of cultural perception of causation, complications and severity of childhood malaria on determinants of treatment and preventive pathways. Int Q Community Health Education 24 (4). http://www.ncbi.nlm.nih.gov/pubmed/17686690 Morenkeji (2009). Perception and management of Malaria in secondary schools in a Nigerian city. Pakistan Journal of Medical Sciences 25 (3). http://www.pjms.com.pk/issues/aprjun209/article/SC1.html Mwenesi, H., Harpham, T., and Snow, R.W. (1995) Child malaria treatment practices among mothers in Kenya. Social Science and Medicine 40: 1271-1277. Nuwaha (2002). People’s perception of malaria in Mbarara, Uganda. Tropical Medicine and International Health 7 (5) http://onlinelibrary.wiley.com/doi/10.1046/j.1365-3156.2002.00877.x/full NHS., 2013. Can I take Malaria tablets if I am pregnant? [Online]. Available on: http://www.nhs.uk/chq/Pages/2475.aspx?CategoryID=54 [Accessed on 29 January 2014] Nosten., F. and White., N., 2007. Artemisinin-Based Combination Treatment of Falciparum Malaria. [Online]. Available on: http://www.ncbi.nlm.nih.gov/books/NBK1713/pdf/pg181.pdf [Accessed on 28 January 2014] Roll Back Malaria., 2010. Economic costs of malaria. [Online]. Available on: http://www.malariaconsortium.org/userfiles/file/Malaria%20resources/RBM%20Economic%20costs%20of%20malaria.pdf [Accessed on 28 January 2014] Roll Back Malaria., 2012. Annual Report 2012. [Online]. Available on: http://www.rollbackmalaria.org/AnnualReport2012/index.html. [Accessed on 28 January 2014] Rhee M et al. (2005). ' Use of insecticide-treated nets (ITNs) following a malaria education intervention in Piron, Mali: a control trial with systematic allocation of households', Malaria Journal 2005, 4:35 doi:10.1186/1475-2875-4-35 http://www.malariajournal.com/content/4/1/35 Sangaré LR, Weiss NS, Brentlinger PE, Richardson BA, Staedke SG, et al. (2012) Determinants of Use of Insecticide Treated Nets for the Prevention of Malaria in Pregnancy: Jinja, Uganda. PLoS ONE 7(6): e39712. doi:10.1371/journal.pone.0039712 http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0039712 Welch K and Fuster M (2012) 'Barriers in access to insecticide treated bed nets for malaria prevention: An analsyis of Combodian DHS data', J Vector Borne Dis. 2012 Mar;49(1):1-7. http://www.ncbi.nlm.nih.gov/pubmed/22585235 WHO., 2003. Fixed-Dose Combinations for HIV/AIDS, Tuberculosis, and Malaria. [Online]. Available on: http://apps.who.int/medicinedocs/en/d/Js6172e/ [Accessed on 29 January] WHO., 2012a. 10 Facts on Malaria in Africa. [Online]. Available on: http://www.afro.who.int/en/clusters-a-programmes/dpc/malaria/features/2287-10-facts-on-malaria-in-africa.html [Accessed on 28 January 2014] WHO., 2012b. Malaria. [Online]. Available on: http://www.salute.gov.it/imgs/C_17_pubblicazioni_1879_ulterioriallegati_ulterioreallegato_0_alleg.pdf [Accessed on 28 Janaury 2014] WHO., 2012c. Intermittent Preventive Treatment of malaria in pregnancy using Sulfadoxine-Pyrimethamine (IPT-p-SP). [Online]. Available on: http://www.who.int/malaria/iptp_sp_updated_policy_recommendation_en_102012.pdf [Accessed on 29 January 2014] WHO. (2009). Dengue – Guidelines for diagnosis, treatment, prevention and control. http://whqlibdoc.who.int/publications/2009/9789241547871_eng.pdf?ua=1 [Accessed on 23 May 2014] WHO. 2014. Climate change and infectious diseases. http://www.who.int/globalchange/publications/climatechangechap6.pdf [Accessed on 23 May 2014] Adapt the TT vaccine to fit local timings. 3 10 Make sure the mother goes to the When the mother goes to the clinic, the health worker will do clinic for a check-up this week. Staff will do tests to check if she is well. She can go with a friend. tests and checks to make sure both mother and baby are well. The health worker will also make sure she is protected from tetanus. Tetanus can be caught through a cut, a burn or a deep wound. The mother can catch it just after birth. The baby can catch it WHO estimated that neonatal tetanus killed approximately 180,000 babies in 2002.(WHO) "Goal Five, Indicator 5.5. Reduce maternal mortality rate with greater antenatal coverage (at least four through the umbilical cord. Tetanus is serious and can be very harmful. Tetanus can be prevented by a vaccine. The vaccine will help the mother to fight the infection if it enters her body. The mother can get a dose at her clinic check-up about now. She may need another dose in a month. She needs to get all the doses at the right time for them to work, and to keep her baby safe. Remind her to find out how many doses she needs. If you want to do one good thing for the baby this week, make sure the mother goes to the clinic for her first check-up. visits). WHO. The Partnership for Maternal, Newborn and Child Health. 2011.Millennium Development Goals. Transport issues (cost, availability, weather conditions) may prevent women accessing clinics. Women may need family permission or funding to get to the clinic. In South Africa, reasons for women booking late for antenatal care included: uncertainty about the usefulness of care, difficulty arranging child care and fears about the rudeness of staff. Adjust message to fit local issues. R. Jewkes et al. 1998" WHO. The Partnership for Maternal, Newborn and Child Health. 2011. Millennium Development Goals. References WHO. The Partnership for Maternal, Newborn and Child Health. 2011.Millennium Development Goals; http://www.who.int/mediacentre/factsheets/fs290/en/ NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman. National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed September 2011] Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Khan, Wojdyla et al (2006). 'WHO analysis of the causes of maternal death: a systematic review', Lancet, 367:1066-74. R. Jewkes et al. 1998. Study of health care seeking practices of pregnant women in Cape Town, Report Four: Summary of Findings, Conclusions and Policy Action. Blencowe et al (2011). 'Clean Birth and Postnatal Care Practises to reduce neonatal deaths from sepsis and Tetanus: A Systematic Review and Delphi Estimation of Mortality Effect', BMC Public Health, 11 (3). WHO (2008), Managing puerperal sepsis. WHO, 2008. Tetanus: Immunisation, vaccines and biologicals. http://www.who.int/immunization/topics/tetanus/en/ accessed July 2012. Around a quarter of pregnant women 3 11 If the mother has a miscarriage, give Pregnancy is a very special time for the mother and her family. have some sort of bleeding in the first her your support. It isn't her fault. But sometimes there are complications. You can help by trimester. (Weiss et al 2004, NGC 2005, Sadly, miscarriage is common early in looking out for them. This way, you can get help quickly and Poulouse et al 2006) pregnancy. help prevent the mother and baby from being harmed. Tell the mother that slight bleeding is not unusual. But if it comes with pain, it may be a miscarriage. Support her and go to the clinic. Ask the mother to be aware of any pain in the lower stomach. If the mother complains of pains in this area, it is best to get her to the clinic. Help her to travel there quickly and easily. Another danger sign is bleeding from the birth canal. Talk to the mother about this sign and ask her to tell you if she notices it. If the mother starts bleeding, get her to the clinic. Make sure she has transport and someone to go with her if you can’t. You can also help the mother by preparing an emergency plan. Find out the fastest route to the clinic and the best transport to take. Although this is not unusual, it is important for a pregnant woman and the family to recognize the danger signs in pregnancy so she can be taken, when necessary, to a qualified health professional. Loss of blood in pregnancy can be a sign of a complication. USAID. Counselling Cards for Maternal and Neonatal Health Even though about one in four pregnancies ends in miscarriage, there’s a lot that we still don’t know about why it happens. That means that most women never find out the cause of their loss, even if they have investigations. Miscarriage Association. Set up an emergency fund. Save a little money every day. Leave money for transport if you are away from home. Have taxi and ambulance numbers ready and always keep some balance on your phone. This way, if there is ever an emergency, the mother can get help fast. Planning ahead helps to keep the mother and her baby safe. If you want to do one good thing for the baby this week, prepare an emergency plan. References USAID. Counselling cards for maternal and neonatal health for community health workers Miscarriage Association. Causes, tests and treatment. Accessed 25/07/2012 http://www.miscarriageassociation.org.uk/information/causes-tests-and-treatment/ K. Danielsson. 2008. After miscarriage: Medical facts and emotional support for pregnancy loss. 12 Make sure the family washes their Pregnancy can make the mother ill more easily. Washing hands In 2008, 2.6 billion people had no access to a hygienic toilet or latrine and 1.1 hands after using the toilet and is one of the best ways to keep sickness at bay. It removes lots billion were defecating in the open. before eating. This will keep germs of germs that could make her sick. away and keep the mother healthy. Encourage the whole family to wash their hands often. They should wash their hands when they come home, after using the toilet, after handling animals, changing nappies and before preparing food. The best way to clean hands is with plenty of clean water and soap. Make sure there is enough in the house for the whole family to use. If the family does not have soap, buy some from the market. Inadequate sewerage spreads infections such as schistosomiasis, trachoma, viral hepatitis and cholera. A review of more than 30 studies found that handwashing with soap cuts the incidence of diarrhoea by nearly half.(Fewtrell, Kaufmann et al., 2005; WHO, 2011) When washing hands, it is best to wash the wrists and under the nails, too. This will remove lots of germs. It will be worth it for a healthy family. If you want to do one good thing for the baby this week, encourage the whole family to wash their hands often. Set a good example, and wash your own hands often. References Van Wyk, R. 2007. "A review of health and hygiene promotion as part of sanitation delivery programmes to informal settlements in the City of Cape Town". CPUT Theses & Dissertations. Paper 48. http://dk.cput.ac.za/td_cput/48 Duse, AG et al. 2003. Coping with hygiene in South Africa, a water scarce country. International Journal of Environmental Health Research. Volume 13, Supplement 001: S95-S105. 24th WEDC Conference. 1998. Sanitation and Water for All. Operation and Maintenance of Water and Sanitation Facilities. Ntombentle Zungula, South Africa. Langiano, E. 2011. Food safety at home: knowledge and practices of consumers. Journal of Public Health: 1-11. FDA. Food Safety for Moms-to-Be- Educator’s Resource Guide. www.cfsan.fda.gov/pregnancy.html Journal of Diarrhoeal Diseases Research, 14:2. 1996. UNICEF, The London School of Hygiene and Tropical Medicine. 1999. Towards Better programming - A manual on hygiene promotion. Phaswana-Mafuya, N. and Shukla N. Factors that could motivate people to adopt safe hygienic practices in the Eastern Cape Province, South Africa. Afr Health Sci. 2005 March; 5(1): 21–28 UNICEF. 2012. Diarrhoea. http://www.unicef.org/health/index_43834.html. [Accessed on 3 June 2014] WHO. 2011. Zinc supplementation in the management of diarrhoea. http://www.who.int/elena/titles/bbc/zinc_diarrhoea/en/. [Accessed on 3 June 2014] WHO. 2013. Diarrhoeal Disease. http://www.who.int/mediacentre/factsheets/fs330/en/ [Accessed on 3 June 2014] Water pollution, unsafe water handling 3 13 See that the mother drinks plenty of With a baby on the way, the mother will need to drink lots of and storage of water compounds are clean boiled water every day and water. This will help to keep her feeling refreshed. Encourage eats an extra mouthful of food at each meal. This will keep her strong. her to drink clean water. This will keep germs and sickness away. To make the water clean, it needs to be boiled and filtered. Pour water through a clean cotton cloth to remove any dirt. Then bring the water to a rolling boil for a minute. This process makes the water clean, killing the germs and removing any bits of dirt in the water. Make sure that there is plenty of clean water in the mother’s home by preparing enough water for the whole family for the day. This will help to keep everyone healthy. Keep it in a cool area and covered to stop flies and dirt getting in. some of the serious problems remain in many developing countries (UNICEF 2013). Water often can be made safe to drink by boiling, adding disinfectants, or filtering (CDC 2013). But if there is a method more appropriate for your community, substitute it with boiling. Dehydration can lead to complications, spontaneous abortion or early labour. (NCCWCH,2008) An estimated 2 million yearly diarrhoeal deaths are related to unsafe water, sanitation, and hygiene - majority among children under 5. (WHO. 2004. Water, Sanitation and Hygiene. Links to Health: Facts and Figures.) Encourage the mother to drink plenty of clean water every day. She may need extra water if it is hot. Also, encourage her to take plenty of clean water with her when she goes out. Drinks sold by vendors are not always safe. They could harm the mother and her baby. If you want to do one good thing for the baby this week, make sure the family prepares plenty of clean water each day. References WHO. 2014. Health through safe drinking water and basic sanitation. http://www.who.int/water_sanitation_health/mdg1/en/ [Accessed on 27 May 2014] WHO. 2014. United Nations Synthesis Report on Arsenic in Drinking Water. http://www.who.int/water_sanitation_health/dwq/arsenicun3.pdf?ua=1 [Accessed on 27 May 2014] WHO. 2014. Progress on Drinking Water and Sanitation. http://apps.who.int/iris/bitstream/10665/112727/1/9789241507240_eng.pdf?ua=1 [Accessed on 27 May 2014] Pica may be more common than we 4 14 Make sure the mother doesn't eat Many pregnant women crave non-foods. It’s a common assume (ranging from (6%-38%). Many non-foods such as soil. They may symptom of pregnancy. may not report pica because they are harm the baby. Many pregnant ashamed to report. So pica needs to be women crave non-foods during These cravings are caused by the hormones in the mother’s addressed in a non-judgemental tone. pregnancy. body. Cravings may also be caused by the mother lacking a certain nutrient. As long as the mother craves actual food, it is alright for her to eat it. Sometimes the mother may begin to crave non-foods like soil. Things like soil, clay and sand can be very harmful to the mother and her baby. They can contain lots of germs and could give the mother worms. Explain this to friends and family and advise the mother not to eat any non-foods. This will keep her and her baby healthy. Maternal malnutrition affects women’s chances of surviving pregnancy. Serious maternal malnutrition is common in subSaharan Africa, South Asia and SouthEast Asia, and is critical in Bangladesh, Eritrea and India. Maternal and child malnutrition is the single leading cause of health loss worldwide. (Blössner and de Onis, 2005; WHO,2011) If the mother continues to crave non-foods, take her to the clinic. Staff there will be able to help her. If you want to do one good thing for the baby this week, make sure the mother has plenty of healthy food to eat. References Blössner and de Onis,2005. “Malnutrition - Quantifying the health impact at national and local levels”, Environmental Burden of Disease Series, No. 12. WHO: Geneva. Seumo, E.F. and Abdallah F. Nutritional Counseling for Pregnant Women in Tanzania. USAID, ACCESS. Black R.E. et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 2008; 371: 243-60 doi: 10.1016/S0140-6736(07)61690-0 pmid:18207566 WHO. 2011. Background Paper 2 - A Review of health interventions with an effect on nutrition pdf. 1.51Mb “Progress for Children - A Report Card on Maternal Mortality”. UNICEF, No. 7, September 2008 USAID. Counselling cards for maternal and neonatal health for community health workers Walker ARP et al. (1985) Nausea and vomiting, cravings and aversions during pregnancy in South African women. British Journal of Obstetrics and Gynaecology 92,484-489. Caplan, C.D. (2001) Evolutionary causes and importance of pregnancy sickness. (http://www.geogle.com/derekeqplan.htm) site visited on 26/08/2006 Coronios-vargas, M. et al. (1991) Cultural influences on food cravings and aversions during pregnancy. Ecology of Food and Nutrition 27, 43-49. Darkish, O.A., Amine, E.K. & Abdullah, S.M. (1982) Food habits during pregnancy and lactation in Iraq. Food and Nutrition Bulletin 4, 14-16. Corbett RW et al. (2003) Pica in pregnancy: does it affect pregnancy outcomes? MCN Am J Matern Child Nurs. 2003 May-Jun;28(3):183-9; quiz 190-1. http://www.ncbi.nlm.nih.gov/pubmed/12771697 Nyaruhucha CNM (2009), “Food cravings, aversions and pica among pregnant women in Dar es Salaam, Tanzania”, Tanzania Journal of Health Research, 11(1): 29-34 WHO recommends smoking 4 15 Encourage the mother not to smoke If the mother breathes in smoke or drinks alcohol, it could interventions such as counseling and or drink alcohol while pregnant. It make her baby weak and sickly. behaviour change therapy. Check what could harm her baby. Ask her family services are available in your area and to smoke outside, too. If the mother smokes, explain to her the effect that the smoke add them to the messages. Research shows that more and more women in will have on her baby. Encourage her to stop smoking. She will developing countries are becoming be more likely to succeed with your support. If you smoke too, why not try quitting with her? If other family members smoke, ask them to smoke outside. If the mother’s house is smoky, it will also have a bad effect on the health of her baby. Make sure that windows are opened often to let the smoke out. Alcohol can also affect the baby’s health. It can make him weak. Explain to the mother that it is best if she doesn’t drink at all during her pregnancy. smokers. Smoking and drinking alcohol by pregnant women is associated with low birthweight and premature birth, as well as higher rates of illness, breathing problems, and sudden infant death syndrome (SIDS). Can also result in birth defects.(WHO, 2011) If you want to do one good thing for the baby this week, encourage the mother to not smoke or drink alcohol. References Seumo, E.F. and Abdallah F. Nutritional Counseling for Pregnant Women in Tanzania. USAID, ACCESS. Black R.E. et al. Maternal and child undernutrition: global and regional exposures and health consequences.Lancet 2008; 371: 243-60 doi: 10.1016/S0140-6736(07)61690-0 pmid:18207566 Victora CG et.al. Worldwide timing of growth faltering: Revisiting implications for interventions.Pediatrics 2010; 125:e473-e480. Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ 1987; 65: 663–737 Kramer MS, Victora C. Low birth weight and perinatal mortality. In: Semba RD, Bloem MW, eds. Nutrition and health in developing countries. Humana Press, 2001 WHO. 2011. Background Paper 2 - A Review of health interventions with an effect on nutrition pdf, 1.51Mb http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf UNICEF. (2008, October 1). Nutrition: Micronutrients - Iodine, Iron and Vitamin A. Retrieved November 14, 2011, from UNICEF: http://www.unicef.org/nutrition/index_iodine.html WHO/UNICEF. (2007). Reaching Optimal Iodine Nutrition in Pregnant and Lactating Women and Young Children. Geneva: World Health Organization. World Health Organization. (2011). Nutrition: Micronutrient Deficiencies. Retrieved November 14, 2011, from WHO: http://www.who.int/nutrition/topics/idd/en/ WHO. 2007. ' Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation', Public Health Nutrition, 10(12A): 1606-1611.; http://www.who.int/nutrition/publications/micronutrients/PHN10(12a).pdf 4 16 Keep the mother healthy by making Pregnancy can make it easier for the mother to get sick. Tell the The homesetting is considered the first place in which foodborne diseases sure she only eats fresh, well-cooked mother that the food she eats must be clean. develop, due to poor personal and/or food. Food that is left out or raw is full of germs. It could make her sick. Food must be stored in a cool, dry place. This will keep the food environmental hygiene with an increased risk of infection (Istituto Superiore di fresh. Sanità 2003; Comodo et al. 2000; Fara and Proietti 2000; Griffith et al. 1998; Old food that has gone rotten or stale should be thrown away. Istituto Superiore di Sanità 2006; Kagan et al. 2002; Redmond and Griffith 2003; Fruit and vegetables can have a lot of dirt and germs. They must be washed well in clean water before they are cooked. Scott 2001) Food must be cooked in clean water. Food must also be cooked well in order to kill germs. Meat must be cooked until it is no longer pink. Eggs should be firm in the middle. Milk should also be boiled to kill any germs. The kitchen must be kept clean. Dishes and utensils need to be washed with clean water and soap. Animals should be kept away from the kitchen. It's best the mother doesn’t eat or drink anything from street vendors or stalls. They may not be clean. If you want to do one good thing for the baby this week, share these tips with the mother. References Van Wyk, R. 2007. "A review of health and hygiene promotion as part of sanitation delivery programmes to informal settlements in the City of Cape Town". CPUT Theses & Dissertations. Paper 48. http://dk.cput.ac.za/td_cput/48 Duse, AG et al. 2003. Coping with hygiene in South Africa, a water scarce country. International Journal of Environmental Health Research. Volume 13, Supplement 001: S95-S105. 24th WEDC Conference. 1998. Sanitation and Water for All. Operation and Maintenance of Water and Sanitation Facilities. Ntombentle Zungula, South Africa. Langiano, E. 2011. Food safety at home: knowledge and practices of consumers. Journal of Public Health: 1-11. FDA. Food Safety for Moms-to-Be- Educator’s Resource Guide. www.cfsan.fda.gov/pregnancy.html Journal of Diarrhoeal Diseases Research, 14:2. 1996. UNICEF, The London School of Hygiene and Tropical Medicine. 1999. Towards Better programming - A manual on hygiene promotion. Phaswana-Mafuya, N. and Shukla N. Factors that could motivate people to adopt safe hygienic practices in the Eastern Cape Province, South Africa. Afr Health Sci. 2005 March; 5(1): 21–28 Tieu J, Crowther CA, Middleton P. 2008. Dietary advice in pregnancy for preventing gestational diabetes mellitus. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD006674. www.mrw.interscience.wiley.com[Accessed September 2011] Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Langiano, E. 2011. Food safety at home: knowledge and practices of consumers. Journal of Public Health: 1-11 Taking time to rest and relax was urged 4 17 Being pregnant makes the mother Growing a baby is hard work! You can help by persuading the by midwives from a midwife convention tired. She needs extra care. Make family to share some of the mother's work so she can rest in Durban. Not getting enough rest can sure the family members share her more. lead to complications due to exhaustion and dehydration. work and give her time to rest. Help her to order necessary tasks and share out work amongst the family. If the whole family helps, the mother will have more time to rest when she needs to. Why not set an example and help the mother with some work yourself? Encourage the mother to go to bed before it gets too late. She needs about eight hours sleep a night. Going to bed early will give her far more energy and will help her to grow a healthy baby. If you want to do one good thing for the baby this week, share the mother’s work out amongst the family. In Nepal mothers often skipped ANC appointments because they viewed their work load as heavy and unavoidable. Found that some mothers in law prioritised work over their daughter-inlaws health. (B. Simkhada et al 2010) In many cultures pregnant women are expected to continue working in pregnancy. An SMS message on this topic will help the guardian to understand why this may be unhealthy. For example, women in North-east Brazil often continue their agricultural work during late pregnancy. This has been linked to decreased birth weight. Lima et al. (1999). References Williams MA, Miller RS, Qiu C et al. 2010. Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. SLEEP 33(10):1363-71 Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Lima et al. 1999. Influence of heavy agricultural work during pregnancy on birthweight in North-East Brazil. International Journal of Epidemiology vol.28 Murray I, Hassall J. 2009. Change and adaptation in pregnancy. In: Fraser DM, Cooper MA. eds. Myles Textbook for Midwives. 15th ed. Edinburgh: Churchill Livingstone, 189-225 NHS. 2011. Common pregnancy health problems: Sleeplessness. NHS pregnancy care planner. www.nhs.uk [Accessed April 2011] Williams MA, Miller RS, Qiu C et al. 2010. Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. SLEEP 33(10):1363-71B. Simkhada et al 2010. ‘The Role of Mothers-in-Law in Antenatal Care Decision-making in Nepal: a qualitative study’, BMC Pregnancy and Childbirth 10:34 Pick local food to illustrate size of fetus. 5 18 Help the mother cope with dizziness Sometimes pregnant women feel dizzy. This may be because by asking her to rest, eat regular her body is adjusting to the changes of pregnancy, or because snacks and take iron pills. Stock up on she has an empty stomach. Being anaemic can also cause pills before they run out. dizziness. You can help the mother deal with her dizziness. If she says she feels dizzy, take her outside. The fresh air will help. Getting her to lie or sit down will also help. See that she eats often. Remind her to have snacks throughout the day. Make sure she takes food with her when she goes out. 20% of maternal deaths are due to maternal iron-deficiency anaemia and stunting in women. In India - 88% of pregnant and 74% of non-pregnant women are affected. In Africa - 50% of pregnant and 40% of non-pregnant women are anaemic.(The Lancet, 2006) This will stop her blood sugar from dropping and making her feel weak. Make sure she takes her iron pills every day. Iron helps to make more blood which helps her feel less tired and dizzy. Getting too much sun can also cause dizziness. Encourage the mother to wear a hat and long, light clothing when she goes outside. If the mother gets dizziness and a headache, a fast heartbeat or blurry vision, take her to the clinic. These are signs that she is ill. Make sure she can get to the clinic quickly and safely. The staff there will be able to help her. If you want to do one good thing for the baby this week, encourage the mother to eat often. References Bothamley J, Boyle M. 2009. Medical conditions affecting pregnancy and childbirth. Oxford: Radcliffe Publishing, 31-49 CKS. 2008. Anaemia - Iron deficiency. Clinical Knowledge Summaries, Clinical topic. www.cks.library.nhs.uk [Accessed January 2010] Murray I, Hassall J. 2009. Change and adaptation in pregnancy. In: Fraser DM, Cooper MA. eds. Myles Textbook for Midwives. 15th ed. Edinburgh: Churchill Livingstone, 189-225 NHS Choices. 2008. Fainting. NHS Choices, Health A-Z. www.nhs.uk [Accessed January 2010] Rodriguez A, Bohlin G, Lindmark G. 2001. Symptoms across pregnancy in relation to psychosocial and biomedical factors. Acta Obstet Gynecol Scand80(3): 213-23 Maina-Gathigi L et al. (2013) Utilization of folic acid and iron supplementation services by pregnant women attending an antenatal clinic at a regional referral hospital in Kenya. Matern Child Health J. 2013 Sep;17(7):1236-42. doi: 10.1007/s10995-012-1120-x. http://www.ncbi.nlm.nih.gov/pubmed/22907273 Peña-Rosas JP et al. (2012) Effects and safety of preventive oral iron or iron + folic acid supplementation for women during pregnancy http://summaries.cochrane.org/CD004736/effects-and-safety-of-preventive-oral-iron-or-iron--folic-acid-supplementation-for-women-during-pregnancy#sthash.lFl3YQiu.dpuf Nearly 34% of maternal deaths in Africa 5 19 Find out the mother's blood type at It is important to plan for the birth now. Planning ahead will and more than 30% in Asia are due to the clinic. Then find people who make the event less stressful for the mother. PPH. (MCHIP-USAID) match. This may save her life if she bleeds heavily after the birth. Encourage the family to start saving money for when the baby is here. You could set an example and begin saving yourself. Saving will help the family have more money ready for when the baby arrives. Births do not always go to plan. Sometimes there are complications. If the mother loses a lot of blood, she will need a blood transfusion. Find out her blood group at the clinic. By knowing her blood group, you will be able to identify the people who could donate blood to her in advance. This means that the mother will get a transfusion much more quickly. Why don’t you find out the whole family’s blood types? Once you have matched them with the mother, make sure you have their contact details. They may be useful in the future. If you want to do one good thing for the baby this week, encourage the mother to find out her blood group. References Lynn F, McNeill J, Alderdice F. 2010. Current trends in antenatal screening services: results from a regional survey. Ulster Med J 79(1):12-15 NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman. National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed May 2011] RCOG. 2003. Prevention of early onset neonatal group B streptococcal disease. Royal College of Obstetricians and Gynaecologists, Green-top guideline, 36. London: RCOG press. www.rcog.org.uk [pdf file, accessed May 2011] Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID WHO (2008) Universal access to safe blood transfusion. WHO recommends calcium 5 20 Encourage the mother to pay Around now, the mother will feel her baby move for the first supplementation for pregnant women attention to her baby's movements. time! Over time, the movements will get stronger as the baby from 20 weeks gestation until the end of Take her to the clinic if the grows. pregnancy. If this is routine in your area, movements slow or stop. encourage householder to make sure the mother starts calcium pills. Sometimes the baby will be still and sleepy, and at other times he will wriggle about. Encourage the mother to notice her baby’s routine. Remind her to spend a few minutes every day feeling her baby’s movements. If she notices that her baby’s movements slow down or stop, take her to the clinic. A health worker will be able to check that the baby is healthy. If the mother doesn’t feel the baby move soon, encourage her to speak to the health worker at the clinic. The health worker Inappropriate response to fetal movements is one of top reasons for stillbirth in South Africa (WHO; Making Pregnancy Safer) Apart from being an element indicating fetal life, fetal movements are associated with embryo-fetal health. A marked reduction or interruption of such will be able to check that everything is going well. The mother may need to start taking calcium pills daily to prevent problems later on in pregnancy. But she shouldn’t take them together with her iron pills. If she takes an iron pill in the morning, she needs to take the calcium pill in the evening. movements should suggest health problems or even fetal death. CLAP/WRPAHO/WHO 2009 If you want to do one good thing for the baby this week, encourage the mother to spend time feeling her baby move. References http://www.who.int/making_pregnancy_safer/countries/soa.pdf Arulkumaran S, Anandakumar C, Wong YC, et al. 1989. Evaluation of maternal perception of sound-provoked fetal movement as a test of antenatal fetal health.Obstet Gynecol 73(2):182-6 Chutiwongse S, Tannirandorn Y, Sukcharoen N, et al. 1991. Maternal perception of sound-provoked fetal movement as a test of antepartum fetal wellbeing. J Med Assoc Thai 74(5):257-63 Gillieson M, Dunlap H, Nair R, et al. 1984. Placental site, parity, and date of quickening. Obstet Gynecol 64(1):44-5 Heazell AEP, Froen JF. 2008. Methods of fetal movement counting and the detection of fetal compromise. J Obstet Gynaecol 28(2):147-54 Hijazi ZR, East CE. 2009. Factors affecting maternal perception of fetal movement. Obstet Gynecol Surv 64(7):489-97 Holm Tveit JV, Saastad E, Stray-Pedersen B, et al. 2009. Maternal characteristics and pregnancy outcomes in women presenting with decreased fetal movements in late pregnancy. Acta Obstet Gynecol Scand Nov 2, epub ahead of print. Mangesi L, Hofmeyr GJ. 2007. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database of Systematic Reviews (1):CD004909.mrw.interscience.wiley.com [pdf file, accessed December 2009] NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman.National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed December 2009] Olesen AG, Svare JA, 2004. Decreased fetal movements: background, assessment, and clinical management, Acta Obstet Gynecol Scand 83(9):818-26 O'Sullivan O, Stephen G, Martindale E, et al. 2009. Predicting poor perinatal outcome in women who present with decreased fetal movements J Obstet Gynaecol 29(8):705-10 Tveit JV, Saastad E, Stray-Pederson B, et al. 2009. Reduction of late stillbirth with the introduction of fetal movement information and guidelines - a clinical quality improvement. BMC Pregnancy Childbirth 9:32. www.ncbi.nlm.nih.gov [pdf file, accessed December 2009] de Vries JI, Fong BF. 2006. Normal fetal motility: an overview. Ultrasound Obstet Gynecol 27(6):701-11 WHO (2013). Calcium supplementation in pregnant women. http://apps.who.int/iris/bitstream/10665/85120/1/9789241505376_eng.pdf?ua=1 [Accessed on 2 May 2014] In South Africa no antenatal care was the 5 21 If the mother is ill or in pain, get to When a woman is pregnant, her body goes through many topmost reason for stillbirths. In 2010 the clinic. She may need treatment. changes. But there are some changes that are signs of a just over half of all pregnant women Vomiting, fever, pain and bleeding problem. made the WHO-recommended minimum are signs of a problem. of four antenatal visits. In Africa and Fever could mean she has an infection. She will need treatment South-East Asia less than half of all births had skilled assistance. (WHO; making at the clinic and rest. pregnancy safer) A sharp pain in the abdomen is another danger sign. If the pain doesn’t go away, take the mother to the clinic. The staff there can find out what is wrong. Ask the mother to tell you if she has any bleeding. This can be a sign that there is a problem with the pregnancy. Take her to the clinic if she starts bleeding. Vomiting is also a sign of illness, as is feeling constantly thirsty and not passing much urine. The mother will need treatment at the clinic. Check if the mother is feeling breathless or has pain when urinating. As soon as any of these signs are spotted, take the mother to clinic. Make sure she has a fast way of getting there and that there is someone to go with her if you can’t. If you want to do one good thing for the baby this week, discuss these signs with the family so that everyone knows what to look out for. References Baker P (Ed). 2006. Obstetrics by ten teachers. 18th edition. London: Arnold BDA. 2007. Fluid – why you need it and how to get enough. British Dietetic Association. www.bda.uk.com [pdf file, accessed September 2011] Cahill AG, Bastek JA, Stamilio DM et al. 2008. Minor trauma in pregnancy--is the evaluation unwarranted? Am J Obstet Gynecol. 2008 Feb;198(2):208.e1-5. Crafter H. 2009. Problems of pregnancy. In: Fraser DM, Cooper MA. eds. Myles Textbook for Midwives. 15th ed. Edinburgh: Churchill Livingstone, 333-359 Gaufberg S. 2008. Abruptio Placentae. emedicine.www.emedicine.medscape.com [Accessed September 2011] Murray I, Hassall J. 2009. Change and adaptation in pregnancy. In: Fraser DM, Cooper MA, eds. Myles Textbook for Midwives. 15th ed. Edinburgh: Churchill Livingstone, 189-225 NCCWCH. 2007. Intrapartum care: care of healthy women and their babies during childbirth. National Collaborating Centre for Women's and Children's Health (NCCWCH). London: RCOG Press. www.rcog.org.uk [pdf file, accessed September 2011] NCCWCH. 2008a. Diabetes in pregnancy management of diabetes and its complications from preconception to the postnatal period. National Collaborating Centre for Women's and Children's Health (NCCWCH). London: NICE.www.nice.org.uk [pdf file, accessed August 2011] NCCWCH. 2008b. Routine antenatal care for healthy pregnant women.www.nice.org.uk [pdf file, accessed September 2011] PRODIGY. 2008. Nausea and vomiting in pregnancy: Clinical topic.www.prodigy.clarity.co.uk [Accessed September 2011] PRODIGY. 2009. Urinary tract infection (lower) in women: Clinical topic.www.prodigy.clarity.co.uk [Accessed September 2011] PRODIGY. 2010. Ectopic pregnancy: Clinical topic. www.prodigy.clarity.co.uk[Accessed September 2011] RCOG. 2006a. Obstetric cholestasis. Royal College of Obstetricians and Gynaecologists, Green-top guideline, 43. London: RCOG press.www.rcog.org.uk [pdf file, accessed September 2011] RCOG. 2006b. Preterm prelabour rupture of membranes. Royal College of Obstetricians & Gynaecologists, Green Top Guideline No. 44. London: RCOG Press. www.rcog.org.uk [pdf file 160KB; AccessedSeptember 2011] RCOG. 2007. Obstetric cholestasis (itching liver disorder): information for you.Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk [pdf file, accessed September 2011] RCOG. 2010a. An ectopic pregnancy: information for you. www.rcog.org.uk[Accessed September 2011] Symonds IM. 2009. Abnormalities of early pregnancy. In: Fraser DM, Cooper MA. eds., Myles Textbook for Midwives 15th ed. Edinburgh: Churchill Livingstone, 313-32 6 22 Ease the mother's backache with a massage. Try supporting her bump with pillows when she lies down, too. This will make her comfortable. As the baby continues to grow, the mother may find it more uncomfortable to lie down or get to sleep. She may have backache or leg cramps. A back massage will help ease the mother's back ache. Whilst she is lying on her side, slowly rub her back in gentle, but firm strokes, focusing on her lower back and the areas on either side of her spine. You could also help to make her more comfortable by tucking a pillow under her bump when she lies on her side at night. This will help to take some of the weight of the baby off her back and sides. A warm compress, bath or shower can help to take her aches and pains away. Why don’t you suggest these to her? Leg cramps can wake her up at night. Stretch the leg and rub the calf muscle. Encourage her to stretch her legs every day. She can do this by standing on her tiptoes or pointing her toes. Drinking plenty of clean water will also help. Make sure she drinks throughout the day. If you want to do one good thing for the baby this week, help the mother to have a good night's rest. References BAP. 2010. Consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. British Association for Psychopharmacology. Journal of Psychopharmacology 0(0):1-25.www.bap.org.uk [Accessed May 2011] CKS. 2009. Clinical topic: Insomnia. NHS Clinical Knowledge Summaries.www.cks.uk [Accessed May 2011] Stacey T, Thompson JMD, Mitchell EA, et al. 2011. Association between maternal sleep practices and risk of late stillbirth: a case-control study. BMJ 342.www.bmj.com [Accessed June 2011] An estimated 1.7 million people died 6 23 Make sure anyone in the family with If the mother catches TB, it could be harmful to her and her from TB in 2009. The highest number of TB gets treated. TB can make baby. deaths was in the Africa Region. pregnant women very sick. A cough (WHO, 2011) that lasts and chest pain are signs of TB. TB is spread through the air by coughs and sneezes. The germs can stay in the air for a long time. If someone in the mother’s family has TB, tell them to get treatment. They won’t be infectious once they have had treatment for two days. They must complete the whole course of treatment, even if they feel better. If they stop taking the medicine, the TB will come back. Ask them to cover their mouth and nose when sneezing and coughing, and wash their hands afterwards. This will help to prevent the spread of germs to the mother. Look out for signs of TB. A cough with a fever, tiredness and unexpected weight loss are all signs of TB. If you spot any of these signs, take the ill person to the clinic for treatment straightaway. Eating lots of fruit and vegetables will keep the whole family healthy. Help to keep illness away by getting the family and the mother plenty of good food to eat. If you want to do one good thing for the baby this week, look out for signs of TB. References WHO (2013) Global Tuberculosis Report. http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf?ua=1 WHO (2014) Guidance for national tuberculosis programmes on the management of tuberculosis in children, Second edition; http://apps.who.int/iris/bitstream/10665/112360/1/9789241548748_eng.pdf?ua=1&ua=1 WHO (2013) Guideline: Nutritional care and support from patients with Tuberculosis; http://apps.who.int/iris/bitstream/10665/94836/1/9789241506410_eng.pdf?ua=1 WHO (2012) Recommendations for investigating contacts of persons with infectious tuberculosis in low- and middle-income countries http://apps.who.int/iris/bitstream/10665/77741/1/9789241504492_eng.pdf?ua=1 WHO (2013) Systematic screening for active tuberculosis: principles and recommendations. http://apps.who.int/iris/bitstream/10665/84971/1/9789241548601_eng.pdf?ua=1 WHO (2009) WHO policy on TB infection control in health-care facilities, congregate settings and households. http://whqlibdoc.who.int/publications/2009/9789241598323_eng.pdf?ua=1 Liefooghe R et al. (1997) From their own perspective. A Kenyan community's perception of tuberculosis Tropical Medicine & International Health, 2(8): 809–821, http://onlinelibrary.wiley.com/doi/10.1046/j.1365-3156.1997.d01-380.x/abstract In South Africa no antenatal care was the 6 24 Make sure the mother gets to her You can make sure that both mother and baby are healthy and topmost reason for stillbirths. In 2010 second check-up this week. Suggest happy by helping her get to the clinic. It is time for her second just over half of all pregnant women the family starts saving money for visit. made the WHO-recommended minimum other check-ups and the birth, too. of four antenatal visits. In Africa and South-East Asia less than half of all births It is important for the mother to visit the clinic regularly had skilled assistance. (WHO; making throughout her pregnancy. She will need at least four visits. At pregnancy safer). each visit, the health worker will check that mother and baby are strong and healthy. They will also be able to spot any problems. Help the mother receive this important care by making sure she has the time and money to go. Get someone to go with her if you can’t. By doing this, you will really be helping to keep the mother and her baby safe and healthy. If you want to do one good thing for the baby this week, make In accordance with WHO guidelines but fit to meet local ANC expectations. sure the mother can go to her check-up at the clinic. References http://www.who.int/mediacentre/factsheets/fs290/en/ http://www.who.int/making_pregnancy_safer/countries/soa.pdf DH. 2007. Maternity matters. London: Department of Health www.dh.gov.uk [pdf file, accessed September 2011] Lynn F, McNeill J, Alderdice F. 2010. Current trends in antenatal screening services: results from a regional survey. Ulster Med J 79(1):12-15 NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman. National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed September 2011] Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. WHO. The Partnership for Maternal, Newborn and Child Health. 2011.Millennium Development Goals; http://www.who.int/mediacentre/factsheets/fs290/en/ NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman.National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed September 2011] Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Khan, Wojdyla et al (2006). 'WHO analysis of the causes of maternal death: a systematic review', Lancet, 367:1066-74. R. Jewkes et al. 1998. Study of health care seeking practices of pregnant women in Cape Town, Report Four: Summary of Findings, Conclusions and Policy Action. Pick local food to illustrate size of fetus. 6 25 Every baby's life is precious - girls and Now that the baby is growing very quickly and gaining weight, boys. Keep the baby healthy by making sure the mother eats beans, lentils and meat. you need to make sure that the mother is eating enough. She needs to eat a couple of extra mouthfuls at each meal. Make sure that the mother gets this extra food. Explain to the family why she needs it. You should also encourage her to eat a variety of foods. By eating different foods, she will get lots of goodness to feed her baby. To help the mother and her baby grow strong, encourage her to eat lots of protein. It can be found in fish, meat, lentils, peas and beans. Iron can also be found in these foods. Iron will help the mother and her baby grow. Look out for signs that the mother isn't getting enough iron. She may be feeling dizzy or breathless if she isn't getting 20% of maternal deaths are due to maternal iron-deficiency anaemia and stunting in women. In India - 88% of pregnant and 74% of non-pregnant women are affected. In Africa - 50% of pregnant and 40% of non-pregnant women are anaemic. (The Lancet, 2006) Maternal malnutrition affects women’s chances of surviving pregnancy and the incidence of low birth-weight babies. Serious maternal malnutrition is common in sub-Saharan Africa, South Asia and South-East Asia, and is critical in Bangladesh, Eritrea and India. Maternal and child malnutrition is the single leading cause of health loss worldwide. (Blossner and de Onis, 2005) Motivational message designed to enough. If you notice that her hands, eyelids or tongue are pale, it means that she is very short of iron. Take her to the clinic fast if you spot these signs. emphasise the importance of both male and female babies. This message also highlights the importance of caring for the mother. If you want to do one good thing for the baby this week, make sure the mother gets two extra mouthfuls at every meal. Remove reference to meat in vegetarian communities. Change foods to ones available locally. References http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf Black R.E. et al. Maternal and child undernutrition: global and regional exposures and health consequences.Lancet 2008; 371: 243-60 doi: 10.1016/S0140-6736(07)61690-0 pmid:18207566 Blössner and de Onis,2005. “Malnutrition - Quantifying the health impact at national and local levels”, Environmental Burden of Disease Series, No. 12. WHO: Geneva. Seumo, E.F. and Abdallah F. Nutritional Counseling for Pregnant Women in Tanzania. USAID, ACCESS. Stoltzfus R.J. and Dreyfuss M.L. Guidelines for the Use of Iron Supplements to Prevent and Treat Iron Deficiency Anemia. International Nutritional Anemia Consultative Group (INACG) “Progress for Children - A Report Card on Maternal Mortality”. UNICEF, No. 7, September 2008 USAID. Counselling cards for maternal and neonatal health for community health workers Essential Nutrition Actions - Improving Maternal-Newborn-Infant and Young Child Health and Nutrition. WHO. 2011 Weekly Iron-Folic Acid Supplementation (WIFS) in Women of Reproductive Age: Its Role in Promoting Optimal Maternal and Child Health. WHO. 2009. Report of the UNICEF/WHO Regional Consultation. 1999. Prevention and Control of Iron Deficiency Anaemia in Women and Children. Geneva, Switzerland Overview of 12 by 12 Initiative. WHO, UNICEF. WHO. 2011. Background Paper 2 - A Review of health interventions with an effect on nutrition pdf, 1.51Mb WHO.2001. Iron deficiency anaemia: Assessment, prevention and control, A guide for programme users. Essential Nutrition Actions - Improving Maternal-Newborn-Infant and Young Child Health and Nutrition. WHO. 2011 Weekly Iron-Folic Acid Supplementation (WIFS) in Women of Reproductive Age: Its Role in Promoting Optimal Maternal and Child Health. WHO. 2009. Khan, Wojdyla et al (2006). 'WHO analysis of the causes of maternal death: a systematic review', Lancet, 367:1066-74.http://www.who.int/mediacentre/factsheets/fs348/en/ Local adaptation for whether baby will 6 26 Make plans now for the mother to The day of the birth is getting closer now. It is time you, the have her baby at a clinic or with a family and the mother started thinking about the best place for be had at a clinic or hospital. trained birth attendant. It is the safest way. her to have her baby. The clinic is the safest place. It is clean and the staff there will help to keep germs away from the mother. There will also be help at hand if there are complications. It is best to be prepared, just in case. If the mother does not want to give birth in a clinic, make sure she has a skilled birth attendant with her. The attendant will be 30-40% of infections resulting in neonatal sepsis deaths are transmitted at the time of childbirth (Blencowe et al, 2011) Every year an estimated 30 million newborns acquire infection (MCHIPUSAID) able to advise and support the mother during her labour. It will make her birth much safer. Why don’t you start discussing these things with the mother and family? Once a decision is made, you can all begin making plans for the big day! If you want to do one good thing for the baby this week, start talking to the mother about where she wants to have her baby. References Lang, J. B. and Elkin, E. D. (1997), A Study of the Beliefs and Birthing Practices of Traditional Midwives in Rural Guatemala. Journal of Midwifery & Women’s Health, 42: 25–31. Goldie SJ, Sweet S, 2010. Alternative Strategies to Reduce Maternal Mortality in India: A Cost-Effectiveness Analysis. PLoS Med 7(4): e1000264. Mathai, M. (2011), To ensure maternal mortality is reduced, quality of care needs to be monitored and improved alongside increasing skilled delivery coverage rates. BJOG: An International Journal of Obstetrics & Gynaecology, 118: 12–14. Chuku, S.N. 2008. Low Birth Weight in Nigeria: Does Antenatal Care Matter? Institute of Social Studies, The Hague, The Netherlands. Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Mathai, M. (2011), To ensure maternal mortality is reduced, quality of care needs to be monitored and improved alongside increasing skilled delivery coverage rates. BJOG: An International Journal of Obstetrics & Gynaecology, 118: 12–14. Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF (2006). 'WHO analysis of causes of maternal death: a systematic review', Lancet, 367: 1066–74. Taking time to rest and relax was urged 6 27 If the mother has swollen hands and Growing a baby is hard work. Sometimes it can become very in many midwife messages from a feet, encourage her to rest with her uncomfortable. You may want to give the mother some herbal midwife convention in Durban. Not feet up. Swelling is caused by the remedies, but it is best not to. Some remedies can be very getting enough rest can lead to weight of the baby. harmful for the mother and her baby. There are other ways you complications due to exhaustion and dehydration can help her. In Nepal mothers often skipped ANC appointments because they viewed their If the mother is suffering with heartburn, try giving her some work load as heavy and unavoidable. cool, boiled milk. This will help to soothe the burning sensation. Found that some mothers in law prioritised work over their daughter-inAlso make sure that the mother gets plenty of rest. Resting with laws health. (B. Simkhada et al 2010). her feet up will help swollen ankles and veins. You may notice that the mother has nosebleeds. It is caused by the extra blood in her body. Pinch the top of her nostrils and ask her to lean forwards slightly. This will stop the flow. Oedema is not a serious problem, but it is common in pregnancy. Referring to it will help the mother to build a relationship with the SMS programme. A heavy baby can also cause abdominal pain. Get the mother to lie on her side and prop up her bump with pillows. This will help. Between 50 and 80 per cent of healthy pregnant women will have oedema in pregnancy. (Shepherd et al 2004:259). If the mother’s discomforts continue, or if she starts bleeding, getting headaches or has a pain down one side of her bump, take her to the clinic. If you want to do one good thing for the baby this week, try to make the mother’s pregnancy more comfortable. References CKS. 2008. Dyspepsia: pregnancy associated. Clinical Knowledge Summaries, Clinical topic. www.cks.nhs.uk [Accessed May 2011] NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman.National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed May 2011] NHS Choices. 2010. Indigestion (dyspepsia) in pregnancy. NHS Choices, Health A-Z. www.nhs.uk [Accessed May 2011] Rodriguez A, Bohlin G, Lindmark G. 2001. Symptoms across pregnancy in relation to psychosocial and biomedical factors. Act Obstet Gynecol Scand80:213-23 Bamigboye AA, Smyth RMD. 2007. Interventions for varicose veins and leg oedema in pregnancy. Cochrane Database of Systematic Reviews(1):CD001066. mrw.interscience.wiley.com [pdf file, accessed December 2009] CKS. 2008. Varicose veins. Clinical Knowledge Summaries, Clinical topic.www.cks.nhs.uk [Accessed December 2009] NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman.National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed December 2009] NHS Choices. 2008. Varicose veins. NHS Choices, Health A-Z. www.nhs.uk[Accessed December 2009] NHS Evidence. 2009. Annual evidence update on antenatal and pregnancy care - heartburn, constipation, haemorrhoids, varicose veins and vaginal discharge during pregnancy NHS Evidence, Women's health. www.library.nhs.uk[Accessed December 2009] Bamigboye AA, Smyth RMD. 2007. Interventions for varicose veins and leg oedema in pregnancy. Cochrane Database of Systematic Reviews(1):CD001066. mrw.interscience.wiley.com [pdf file, accessed December 2009] NHS Choices. 2008. Oedema. NHS Choices, Health A-Z. www.nhs.uk [Accessed December 2008] Bamimore O, Silverberg MA. 2009. Epistaxis. eMedicine.emedicine.medscape.com [Accessed December 2009] McNabb M. 2004. Maternal and fetal physiological responses in pregnancy. In: Henderson C, McDonald S. eds. Mayes' midwifery. 13th ed. London: Bailliere Tindall, 288-311 NHS Choices. 2009. Nosebleed. NHS Choices, Health A-Z. www.nhs.uk[Accessed December 2009] Bamigboye AA, Smyth RMD. 2007. Interventions for varicose veins and leg oedema in pregnancy. Cochrane Database of Systematic Reviews(1):CD001066. mrw.interscience.wiley.com [pdf file, accessed December 2009] NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman.National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed December 2009] NHS Choices. 2008. Oedema. NHS Choices, Health A-Z. www.nhs.uk [Accessed December 2008] 7 28 Look out for signs of diabetes. Tiredness, thirst and blurred vision are signs. Take the mother to the clinic if you spot them. By looking out for signs of illness in the mother, you can help keep her safe and healthy. One illness you can look out for is diabetes. Make necessary local changes concerning whether tests will definitely be performed. Pregnancy causes many changes. Sometimes, it can alter blood sugar levels. This can cause the mother to get diabetes – even though she may not have had it before. Diabetes can cause neonatal hyperglycaemia and jaundice. Can also lead to complicated birth due to larger baby. This is a growing problem in low resource settings. (Bellamy L et al, 2009) A mother with diabetes will be very tired, and will need to urinate a lot. She will also be very thirsty and may have blurred vision. If she has any of these signs, take her to the clinic for a check-up. If the mother does get diabetes you can help her through it. Make sure she has plenty of healthy food to eat and that she doesn’t have too many sugary things. Light exercise will also help. Why don’t you both go for a short walk together? You can help prevent diabetes. Check the mother eats well, exercises and stops smoking. Also make sure that the mother can go to all her check-ups. Clinic staff will test for diabetes. If you want to do one good thing for the baby this week, encourage the mother to get tested for diabetes. Reference Bellamy L, Casas J, Hingorani AD, et al. 2009. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373 (9677): 1773-1779 CEMACH. 2007. Diabetes in pregnancy: are we providing the best care? Findings of a national enquiry. Confidential Enquiry into Maternal and Child Health. www.cemach.org.uk [pdf file, accessed August 2010] DH. 2001. National Service Framework for Diabetes. Department of Health.www.dh.gov.uk [pdf file, accessed August 2010] Dempsey JC, Sorensen TK, Williams MA, et al. 2004. Prospective Study of Gestational Diabetes Mellitus Risk in Relation to Maternal Recreational Physical Activity before and during Pregnancy. American Journal of Epidemiology 159(7): 663-6 NCCWCH. 2008. Diabetes in pregnancy management of diabetes and its complications from preconception to the postnatal period. National Collaborating Centre for Women's and Children's Health (NCCWCH). London: RCOG Press.www.nice.org.uk [pdf file, accessed August 2010] NHS Choices. 2010. Gestational diabetes: introduction. How common is gestational diabetes? www.nhs.co.uk [accessed August 2010] Tieu J, Crowther CA, Middleton P. 2008. Dietary advice in pregnancy for preventing gestational diabetes mellitus. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD006674. www.mrw.interscience.wiley.com[Accessed August 2010] Hadlock FP, Yogesh PS, Kanon DJ, Lindsey JV. 1992. Fetal crown-rump length: Re-evaluation of relation to menstrual age (5-18 weeks) with high-resolution real-time US. Radiology 182(2):501-5 Hill M. 2009. Development week by week. University of New South Wales Embryology. embryology.med.unsw.edu.au [Accessed August 2009] Medline Plus Medical Encyclopedia. www.nlm.nih.gov Pick local food to illustrate size of fetus. 7 29 Look out for sudden swelling in the You need to know what changes are normal in pregnancy, and mother's hands, feet and face. These are signs of a problem. Get her to a clinic fast if you spot them. which ones aren't. By knowing when to take the mother to the clinic, you can help keep her safe. Gradual swelling in the hands and feet is quite common. It is caused by the weight of her baby. If the swelling is sudden, then this is a sign of a problem. It is also a problem if she gets swelling with a headache or blurred vision. If she has any of these signs, get the mother to the clinic quickly. They could be symptoms of a condition called preeclampsia. It can be harmful to mother and baby. Keep the mother and her baby safe by making sure she goes to all of her check-ups. She will have her blood pressure checked. High blood pressure can lead to preeclampsia. By getting it checked, clinic staff can make plans for the mother to have a safe birth. Talk to the family about these signs. This way you can all help to keep the mother and her baby safe. If you want to do one good thing for the baby this week, talk to the family about the signs of preeclampsia. WHO recommends that mothers with eclampsia are given magnesium sulphate. Causes 12% of maternal deaths globally an estimated 63,000 women per year (MCHIP-USAID) Hypertension, along with haemorrhage, account for the largest proportion of maternal deaths in developing countries (Khan et al, 2006). PET causes 12% of maternal deaths globally - an estimated 63,000 women per year (MCHIP-USAID) References Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, Forest JC, Giguère Y.Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010 Aug;116(2 Pt 1):402-14 Prof Gus Dekker MD, Prof Baha Sibai MD; Primary, secondary, and tertiary prevention of pre-eclampsia The Lancet, Volume 357, Issue 9251, Pages 209 - 215, 20 January 2001 Hofmeyr GJ, Duley L, Atallah A. Dietary calcium supplementation for prevention of pre-eclampsia and related problems: a systematic review and commentary. BJOG 2007;114:933–43. Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al. Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling. Health Technology Assessment 2008 12(6):1-270 Okafor UV, Efetie RE. Critical care management of eclamptics: challenges in an African setting. Trop Doct. 2008 Jan; 38(1):11-3. Peng, CT. 2008. Review: Calcium Supplementation During Pregnancy Reduces the Risk of Pre-Eclampsia. EBM. (13:8), 38 Dr D Wilhelm Steyn, Hein J Odendaal; Randomised controlled trial of ketanserin and aspirin in prevention of pre-eclampsia; The Lancet, Volume 350, Issue 9087, Pages 1267 - 1271, 1 November 1997 BMJ. 2009. Pre-eclampsia: patient leaflet. BMJ Publishing Group. Duley L. 2009. Pre-eclampsia, eclampsia and hypertension. Clinical Evidence. NICE. 2006. Routine postnatal care of women and their babies. National Institute of Health and Clinical Excellence, Clinical guideline, 37. www.nice.org.uk [pdf file, accessed March 2010] NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman. National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed March 2010] NHS Choices. 2009. Pre-eclampsia NHS Choices, Health A-Z. www.nhs.uk[Accessed March 2010] RCOG. 2006. The management of severe pre-eclampsia/eclampsia. Royal College of Obstetricians and Gynaecologists, Green-top guideline, 10a. London: RCOG press. www.rcog.org.uk [pdf file, accessed March 2010] RCOG. 2007. Pre-eclampsia: what you need to know. Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk [pdf file, accessed March 2010] Khan, Wojdyla et al (2006). 'WHO analysis of the causes of maternal death: a systematic review', Lancet, 367:1066-74. 7 30 Clinic birth is safest. Find out the With the baby’s arrival near, it is time for you and the family to Make necessary local changes about where you would suggest having baby fastest way to get there when it's start making preparations. whether at a clinic, hospital etc. time. Organise transport, money, and have enough airtime on phones. If the mother is having a clinic birth, now is a good time to work out how long it takes to get there. Find out what is the quickest route. Find out what transport is available and which is the fastest, too. If the mother is having her baby at home, encourage her to have a skilled birth attendant. It will help keep her and her baby safe. Talk to her about who could be chosen. Make sure you have their contact details. You may be able to get a birth kit from an NGO. It contains a plastic sheet, gloves, clean string to tie the cord, and tools for cutting the cord. If you can’t get one, find a clean sheet for the Pick local food to illustrate size of fetus. WHO recommends that the mother have a social supporter with her during labour. We have only mentioned early labour here in case mothers are not allowed people with them. If the mother is allowed someone with her during delivery, add this to later messages. If the clinic / hospital is a long way away from the clinic, the family should take that into account, and leave enough time to get there before labour. mother to give birth on. You will also need a clean sharp knife, razor or scissors. Two cloths are also needed - one to dry the baby, and the other to wrap him in. If you want to do one good thing for the baby this week, start preparing for the birth. References Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Lang, J. B. and Elkin, E. D. (1997), A Study of the Beliefs and Birthing Practices of Traditional Midwives in Rural Guatemala. Journal of Midwifery & Women’s Health, 42: 25–31. Goldie SJ, Sweet S, 2010. Alternative Strategies to Reduce Maternal Mortality in India: A Cost-Effectiveness Analysis. PLoS Med 7(4): e1000264. Mathai, M. (2011), To ensure maternal mortality is reduced, quality of care needs to be monitored and improved alongside increasing skilled delivery coverage rates. BJOG: An International Journal of Obstetrics & Gynaecology, 118: 12–14. Chuku, S.N. 2008. Low Birth Weight in Nigeria: Does Antenatal Care Matter? Institute of Social Studies, The Hague, The Netherlands. Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. USAID. Counselling cards for maternal and neonatal health for community health workers Mathai, M. (2011), To ensure maternal mortality is reduced, quality of care needs to be monitored and improved alongside increasing skilled delivery coverage rates. BJOG: An International Journal of Obstetrics & Gynaecology, 118: 12–14. Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF (2006). 'WHO analysis of causes of maternal death: a systematic review', Lancet, 367: 1066–74. 12.1% of stillbirths were caused because 8 31 Get the mother to the clinic as soon Look out for signs that labour is starting. If you spot any, fetch of a delay in seeking medical attention as labour starts. Regular strong the birth attendant or get the mother ready to go to the clinic. during labour in South Africa (WH0). contractions or the breaking of her waters are signs of labour. She needs to go as soon as labour starts. One sign of labour is contractions. Labour contractions are painful and regular. They get stronger and closer together as the labour moves along. At first, the mother may just feel a slight backache or tummy cramps. Another sign is the breaking of the mother’s waters. There may be a trickle or a rush of fluid. Once the mother’s waters have broken she will be at risk of infection. Make sure you get her to the clinic or to her birth attendant fast! If you want to do one good thing for the baby this week, talk to the mother and family about the signs of labour. References Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. USAID. Counselling cards for maternal and neonatal health for community health workers RCOG. 2008b. When your waters break early (preterm prelabour rupture of membranes): information for you. Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk [pdf file, accessed April 2010] McCormick C. 2009. The first stage of labour: physiology and early care. In: Fraser DM, Cooper MA. eds. Myles Textbook for Midwives. 15th ed. Edinburgh: Churchill Livingstone, 457-75 Walsh D. 2004. Care in the first stage of labour. In: Henderson C, McDonald S. eds. Mayes' midwifery. 13th edition. London: Bailliere Tindall, 428-57. WHO http://www.who.int/mediacentre/factsheets/fs290/en/ ANC visit number is in accordance with 8 32 Remind the mother to go to her next You need to keep the baby warm after he is born. Babies can WHO guidelines but fit to meet local ANC check-up. Prepare for an emergency get cold very easily. There are several things you can do. expectations. birth. Get clean water, soap, string and a sharp tool to cut the cord. First, make sure that windows and doors are closed to help prevent cold draughts. Next, dry the baby with a cloth and then wrap him in a warm towel. A hat or cloth should then be put on his head. Babies lose a lot of heat through their heads. Remind the mother not to swaddle him too tightly when she wraps him. Ask the attendant to lay the baby on his mother’s chest and cover them both with a blanket. His mother's body will keep him warm. Skin-to-skin contact will also help mother and baby bond. It can also protect the baby against illness. Check your baby's temperature by feeling her tummy, hands and feet. They should all be warm - not too hot or cold. If the mother has any questions about the birth, encourage her to ask her health worker. She can ask at her next check-up. Make sure she can get there. Hypothermia at birth is one of the most important risk factors for morbidity and mortality in newborn infants of all birth weights and gestational ages. Prevention and management of hypothermia is one of the key interventions for reducing neonatal mortality and morbidity. According to UNICEF, such interventions can help reduce neonatal mortality or morbidity by 18%–42% (McCall et al, 2010) If you want to do one good thing for the baby this week, encourage the mother to go for her next check-up. References McCall EM, Alderdice F, Halliday HL, Jenkins JG, Vohra S. (2010) Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database of Systematic Reviews http://www.who.int/features/factfiles/breastfeeding/en/ WHO. 2011. Essential Interventions, Commodities and Guidelines for Reproductive, Maternal, Newborn and Child Health. WHO (2006), Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice http://whqlibdoc.who.int/publications/2006/924159084X_eng.pdf?ua=1 Immediate and exclusive breastfeeding 8 33 Encourage the mother to breastfeed Offering the mother breastfeeding support is one of the best straight away. The first milk isn't things you can do. Breastfeeding is the best way to help a baby has been identified as important for child nutrition. Is safest nutritional dirty, but is creamy with goodness. grow strong and healthy. It has all the baby needs. It can also option. (MCHIP, USAID/WHO) It's the best food for the baby. help to protect her from illness. Once the baby is born, encourage the mother to start breastfeeding straight away. The first milk the mother makes is very thick and creamy. It is called colostrum. You may have heard that this milk is ‘dirty’. But this milk is the best food for the newborn baby. It is creamy and full of goodness. Feeding the baby anything else is a waste of this precious milk. Globally less than 40% of infants under six months of age are exclusively breastfed. Adequate breastfeeding support for mothers and families could save many young lives. (WHO) The mother will be able to make enough milk to feed her baby. She won’t need anything else. Don’t feed the baby honey or ghee. They could be harmful to the delicate newborn. Encourage the mother to breastfeed whenever her baby wants instead. If you want to do one good thing for the baby this week, explain the benefits of the first milk to the family. Referencing American Academy of Pediatrics. 2004. Breastfeeding and the Use of Human Milk. Pediatrics 115:2. 496-506 UNICEF and WHO. 2009. SECTION 3: BREASTFEEDING PROMOTION AND SUPPORTIN A BABY-FRIENDLY HOSPITAL: A 20-HOUR COURSE FOR MATERNITY STAFF. WHO.2011. Essential Nutrition Actions: Improving Maternal-Newborn Infant and Young Child Health and Nutrition. WHO.2010. WHO Technical Consultation on Postpartum and Postnatal Care. WHO.2003. Global Strategy for Infant and Young Child Feeding. WHO. 2002 NUTRIENT ADEQUACY OF EXCLUSIVE BREASTFEEDING FOR THE TERM INFANT DURING THE FIRST SIX MONTHS OF LIFE. WHO.2001. REPORT OF THE EXPERT CONSULTATION ON THE OPTIMAL DURATION OF EXCLUSIVE BREASTFEEDING. 8 34 Baby needs to be warm. Have warm towels ready and encourage the mother to hold the baby against her skin. Check for draughts, too. If the mother has an early baby, you can help keep the baby healthy and happy. Babies who are born early need extra special care. Encourage the mother to breastfeed as soon as her baby is born. The first milk she produces will give the baby everything she needs to grow stronger. If the baby is not strong enough to feed at the breast, suggest that the mother feeds her baby by expressing milk into a boiled cup. By tilting the cup, the baby will be able to lap the milk. You can also help by encouraging the mother to hold her baby skin to skin. This will keep her warm and will help her to develop. If you want to do one good thing for the baby this week, look out for signs of early labour. Hypothermia at birth is one of the most important risk factors for morbidity and mortality in newborn infants of all birth weights and gestational ages. Prevention and management of hypothermia is one of the key interventions for reducing neonatal mortality and morbidity. According to UNICEF, such interventions can help reduce neonatal mortality or morbidity by 18%–42% (McCall et al, 2010). UNICEF believes that kangaroo mother care (skin to skin) is a key intervention in reducing neonatal mortality and morbidity. KMC was associated with a reduction in the risk of mortality, sepsis, hypothermia and length of hospital stay. (Conde-Agudelo et al, 2011 ; UNICEF, 2007)" Immediate and exclusive breastfeeding has been identified as important for child nutrition. Is safest nutritional option. (WHO) References Butte, N.F. et al. 2002. Nutrient Adequacy of Exclusive Breastfeeding for the Term Infant During the First Six Months of Life. WHO. Carfoot S, Williamson P R, Dickson R. Centre for Reviews and Dissemination; A systematic review of randomized controlled trials evaluating the effect of mother/baby skin-to-skin care on successful breast feeding. Conde-Agudelo A, Belizán JM, Diaz-Rossello J. Kangaroo mother care to reduce morbidity and mortality in low birth weight infants. Cochrane Database of Systematic Reviews 2011, Issue 3. Art. No.: CD002771. DOI: 0.1002/14651858.CD002771.pub2 Cramer K, Wiebe N, Hartling L, Crumley E, Vohra S.; Heat loss prevention: a systematic review of occlusive skin wrap for premature neonates; Complementary and Alternative Research and Education Program, Department of Paediatrics, University of Alberta, Alberta, Canada. Ferber, Makhoul IR. 2004. Pediatrics. 113(4):858-65.; The effect of skin-to-skin contact (kangaroo care) shortly after birth on the neurobehavioral responses of the term newborn: a randomized, controlled trial. Hartley. P. 2008. Neonatal Thermoregulation; http://www.ceufast.com/courses/63/63.htm Lawn JE, Mwansa-Kambafwile J, Horta BL, Barros FC, Cousens S. Centre for Reviews and Dissemination; 'Kangaroo mother care' to prevent neonatal deaths due to preterm birth complications Moore ER, Anderson GC, Bergman N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD003519. DOI: 10.1002/14651858.CD003519.pub2; Mullany et al. 2010. BMC Medicine 2010, 8:43; http://www.biomedcentral.com/1741-7015/8/43 East of England Neonatal Benchmaking Group; NHS; Clinical Guideline: Thermoregulation; May 2011 Wariki WMV and Mori R. Interventions to prevent hypothermia at birth in preterm and/or low-birth-weight infants: RHL commentary (last revised: 1 June 2010). The WHO Reproductive Health Library; Geneva: World Health Organization WHO. 2001. The Optimal Duration of Exclusive Breastfeeding - Report of an Expert Consultation. Geneva. WHO. 2011. Essential Nutrition Actions - Improving Maternal-Newborn-Infant and Young Child Health and Nutrition. WHO, UNICEF. 2009. Baby-Friendly Hospital Initiative. Section 3 - Breastfeeding Promotion and Support in a Baby-Friendly Hospital. Essential newborn nursing for small hospital in resource restricted countries: Learner’s guide. Publication of Department of Pediatrics WHO-CC, New Delhi, 2004. Breastfeeding and the Use of Human Milk. 2005. Pediatrics, 115 ( 2) Goldie SJ, Sweet S, 2010. Alternative Strategies to Reduce Maternal Mortality in India: A Cost-Effectiveness Analysis. PLoS Med 7(4): e1000264. Mathai, M. (2011), To ensure maternal mortality is reduced, quality of care needs to be monitored and improved alongside increasing skilled delivery coverage rates. BJOG: An International Journal of Obstetrics & Gynaecology, 118: 12–14. Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Moore ER, Anderson GC et al. 2007. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews, Issue 3. Art. No.: CD003519. Ferber and Makhoul IR. 2004. “The effect of skin-to-skin contact (kangaroo care) shortly after birth on the neurobehavioral responses of the term newborn: a randomized, controlled trial”. Pediatrics, 113(4):858-65. Conde-Agudelo A, Belizán JM, et al. 2011. “Kangaroo mother care to reduce morbidity and mortality in low birth weight infants”. Cochrane Database of Systematic Reviews, Issue 3. Art. No.: CD002771. Carfoot S, Williamson P R et al. 2005. “evaluating the effect of mother/baby skin-to-skin care on successful breast feeding”. Centre for Reviews and Dissemination; A systematic review of randomized controlled trials. Lawn JE, Mwansa-Kambafwile J, et al. 2010.” 'Kangaroo mother care' to prevent neonatal deaths due to preterm birth complications. “Centre for Reviews and Dissemination. Publication of Department of Pediatrics WHO-CC, New Delhi, 2004. Essential newborn nursing for small hospital in resource restricted countries: Learner’s guide. McCall EM, Alderdice F, Halliday HL, Jenkins JG, Vohra S. (2010) Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database of Systematic Reviews WHO (2006), Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice http://whqlibdoc.who.int/publications/2006/924159084X_eng.pdf?ua=1 In Africa and South-East Asia less than half 8 35 You and the family need to know By preparing the family for complications, you could help of all births had skilled assistance. (WHO) danger signs of birth: fever, save the mother's life. bleeding, fitting and difficult breathing mean the mother needs clinic help. Plan how to get to the clinic quickly. This will help in an emergency. Find out what transport is available and which is the fastest route to the clinic. By doing this you can help keep the mother and her baby safe. You can also prepare for complications by knowing the danger signs. Hypertension and haemorrhage account for the largest proportion of maternal deaths in developing countries. (Khan et al 2006). A labour that is very long or slow could mean there is a problem. Heavy bleeding is another sign that the mother needs help. Sudden swelling of the mother's hands, face and feet will need emergency treatment, too. If you want to do one good thing for the baby this week, work out a fast way to the clinic in case of an emergency. References Alderdice F, McKenna D, Dornan J. 2003. Techniques and materials for skin closure in caesarean section. Cochrane Database of Systematic Reviews Issue 2. Art no CD003577 www.mrw.interscience.wiley.com [Accessed August 2009] Anorlu RI, Maholwana B, Hofmeyr GJ. 2008. Methods of delivering the placenta at caesarean section. Cochrane Database of Systematic Reviews Issue 3. Art no CD004737. www.mrw.interscience.wiley.com [Accessed August 2009] BirthChoiceUK. 2008. Maternity statistics: 2007. www.birthchoiceuk.com [Accessed August 2009] Chippington Derrick D, Lowdon G et al. 2004. Caesarean birth: your questions answered.London: The National Childbirth Trust Hadiati DR, Hakimi M, Nurdiati DS. 2008. Skin preparation for preventing infection following caesarean section. (Protocol). Cochrane Database of Systematic Reviews Issue 4. Art no CD007462. www.mrw.interscience.wiley.com [Accessed August 2009] NCCWCH. 2004. Caesarean section National Collaborating Centre for Women's and Children's Health. Clinical Guideline. www.nice.org.uk [Accessed August 2009] RCOA. 2006. Royal College of Anaesthetists. Risks associated with your anaesthetic. Section 3: Shivering. www.rcoa.ac.uk [Accessed February 2009] RCOG. 2006. Royal College of Obstetricians and Gynaecologists. Caesarean birth: consent advice 7 www.rcog.org.uk [Accessed August 2009] Thomas J, Paranjothy S. 2001, Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit. The National Sentinel Caesarean Section Audit Report. London: RCOG Press Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. USAID. Counselling cards for maternal and neonatal health for community health workers BMJ. 2009. Pre-eclampsia: patient leaflet. BMJ Publishing Group. Duley L. 2009. Pre-eclampsia, eclampsia and hypertension. Clinical Evidence. NHS Choices. 2009. Pre-eclampsia NHS Choices, Health A-Z. www.nhs.uk[Accessed March 2010] RCOG. 2006. The management of severe pre-eclampsia/eclampsia. Royal College of Obstetricians and Gynaecologists, Green-top guideline, 10a. London: RCOG press. www.rcog.org.uk [pdf file, accessed March 2010] RCOG. 2007. Pre-eclampsia: what you need to know. Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk [pdf file, accessed March 2010] Khan, Wojdyla et al (2006). 'WHO analysis of the causes of maternal death: a systematic review', Lancet, 367:1066-74. ANC visit recommendation is in accordance 9 36 This week, get the mother to her The mother needs to go for another check-up this week. with WHO guidelines but fit to meet local check-up and prepare for the birth. Make sure she can get there. ANC expectations Get clean water, soap, string and a sharp tool to cut and clean the cord. It is time for you and the family to prepare for caring for the baby's cord. The cord must be cut and cleaned carefully. It can get infected easily. After the cord is cut, some hospitals apply an antiseptic gel or a liquid on the cord stump. Adapt according to local hospital guidelines and practices. Get the things needed to cut the cord ready now. You need a sharp new knife, razor or scissors. They must be boiled for ten minutes to clean them. You also need two pieces of string. They must also be boiled for three minutes. After the birth, have plenty of soap and clean water ready. Both the mother and the attendant need to wash their hands. If you touch the cord or cut it, you will also need to wash your hands. The cord should be tied once it stops moving. One piece of string is tied about three fingers from the baby, and the other is tied three fingers from the mother. The cord is cut in between. Once the cord is cut, sponge it with clean water and let the air dry it. Putting anything else on the cord could cause an infection. If the cord stump becomes smelly, is bleeding or is red and swollen, take the baby to the clinic. If you want to do one good thing for the baby this week, get the things needed to cut the cord safely. In some areas iron supplementation is recommended for 3 months postpartum. At the clinic visit, the mother can collect her iron pills. Mention this if postpartum iron supplementation is routine in your locality. Neonatal sepsis causes 26% of all neonatal deaths worldwide (Lawn et al. 2005) Every year an estimated 30 million newborns acquire infection and 1-2 million of these babies die. (MCHIP/USAID) 30-40% of infections resulting in neonatal sepsis deaths are transmitted at the time of childbirth (Blencowe et al,2011) References http://labspace.open.ac.uk/mod/oucontent/view.php?id=452292&section=20.5.6 Blencowe et al. BMC Public Health 2011, 11(Suppl 3):S11, Clean birth and postnatal birth practices to reduce neonatal deaths from sepsis and tetanus: a systematic review and Delphi estimation of mortality effect. http://www.biomedcentral.com/1471-2458/11/S3/S11 Melal Mohammad Al .J et al. 2010. Placental Cord Drainage after Vaginal Delivery as part of Management of 3rd Stage of Labour. Medical Journal of Babylon 17:3-4 404-409 Mullany et al. Risk Factors for Umbilical Cord Infection among Newborns of Southern Nepal 2006, Vol. 165, No. 2 Opiyo and English. 2011. What clinical signs best identify severe illness in young infants aged 0-59? A systematic review. Arch Dis Child 96: 1052-59. Sguassero Y, Mignini L, Abalos E. Should placental cord be drained after spontaneous vaginal delivery as part of the third stage of labour? A SUPPORT Summary of a systematic review. December 2008 Soltani H, Poulose TA, Hutchon DR. Placental cord drainage after vaginal delivery as part of the management of the third stage of labour. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No.: CD004665. DOI: 10.1002/14651858.CD004665.pub3 USAID. Counselling cards for maternal and neonatal health for community health workers World Health Organization; Maternal and Newborn Health Safe Motherhood. Care of the Umbilical Cord: A review of the evidence (1998) http://www.who.int/mediacentre/factsheets/fs290/en/ http://www.who.int/making_pregnancy_safer/countries/soa.pdf Who, 2008; http://www.who.int/mediacentre/factsheets/fs134/en/ WHO. The Partnership for Maternal, Newborn and Child Health. 2011.Millennium Development Goals. http://www.who.int/pmnch/media/press_materials/fs/about_mdgs/en/ 9 37 Talk to the mother about the You can protect the baby from illness by making sure she gets Immunisation prevents three million child deaths each year. WHO estimates that 20% importance of vaccines. They will vaccinated. Babies can get sick easily. She will need of the remaining under-five deaths— protect her baby from disease. Her protection to keep her healthy. approximately two million deaths baby will need vaccines after the annually—could be prevented with existing vaccines. birth. Vaccinations are the best way to protect the new baby. They (MCHIP/USAID) will protect her from certain diseases and help her fight off infection. They need to be given at the right time in order to work. Remind the mother to take her baby to get vaccinated. We will send you messages when the mother needs to go. Check she has a way of getting there and that someone goes with her. She can cuddle or feed her baby after the vaccination to comfort her. If you want to do one good thing for the baby this week, talk to the mother about the importance of vaccination. Expanded Programme for Immunisation (EPI) is part of WHO strategy to tackle MDG 4 (WHO) References http://www.who.int/immunisation/documents/positionpapers/ Argarwal. S. et al. 2005. Understanding and Addressing Childhood Immunisation Coverage in Urban Slums. Indian Pediatrics 42:653-663 Oyo-Ita A, Nwachukwu CE, Oringanje C, Meremikwu MM. 2011. Interventions for improving coverage of child immunisation in low- and middle-income countries (Review). Cochrane Collaboration. U.S. Department of Health and Services and the Centers for Disease Control and Prevention.2010. Rotavirus Vaccine: What you need to Know. USAID.2003. Immunisation Essentials: A Practical Guide. WHO (2004) Immunisation in practice: a practical resource guide for Health workers – 2004 update. USAID. Counselling cards for maternal and neonatal health for community health workers WHO. 2003. Kangaroo mother care - a practical guide. 9 38 Reassure the mother that her baby will come when ready. But you can help get labour started by encouraging her to go for short walks. Now the baby is ready to be born, there are things you can do to help get labour started. Encourage the mother to take some short walks. This can sometimes start labour. If you can, go with her to keep her company. Make sure she doesn’t get too tired though; she will need to save energy for the birth! You could also suggest that the mother sits with her knees below her bottom. Give her some pillows to put on her chair when she sits. This helps her baby to move into the right position. You can also encourage the mother to lie on her side at night. Some friends and family members may have advice on how to start labour. They may recommend traditional remedies. It's best if the mother does not take them. They can be harmful. If you want to do one good thing for the baby this week, go for some short walks with the mother. References Andrews CM, Andrews EC. 2004. Physical theory as a basis for successful rotation of fetal malpositions and conversion of fetal malpresentations. Biological Research for Nursing 6:126-40 Anim-Somuah M, Smyth RMD, Howell CJ et al. 2005. Epidural versus non-epidural or no analgesia in labour. Cochrane Database of Systematic Reviews Issue 4. Art no CD000331 www.mrw.interscience.wiley.com [Accessed August 2009] Burden B, Simons M. 2004. Anatomy of male and female reproduction. In: Henderson C, McDonald S. eds. Mayes' midwifery. 13th edition. London: Bailliere Tindall, 65-88 Coates T. 2009. Malpositions of the occiput and malpresentations. In: Fraser DM, Cooper MA. eds. Myles Textbook for Midwives. 15th edition. Edinburgh: Churchill Livingstone, Elsevier, 573-605 Hunter S, Hofmeyr GJ, Kulier R. 2007. Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). Cochrane Database of Systematic Reviews, Issue 4. Art no CD001063 www.mrw.interscience.wiley.com [Accessed August 2009] Lieberman E, Davidson K, Lee-Parritz A et al. 2005. Changes in fetal position during labor and their association with epidural analgesia. Obstetrics and Gynecology 105(5 I):974–82 NCCWCH. 2007. Intrapartum care: Care of healthy women and their babies during childbirth. National Collaborating Centre for Women's and Children's Health. Clinical Guideline. London: RCOG Press. www.nice.org.uk [Accessed August 2009] Sutton J. 1994. Optimal fetal positioning: A midwifery approach to increasing the number of normal births. MIDIRS Midwifery Digest 4(3): 283-6 Sutton, J. and Scott, P. 1996. Understanding and Teaching Optimal Foetal Positioning. Tauranga, New Zealand: Birth Concepts Vance ME. 2009. The female pelvis and the reproductive organs. In: Fraser DM, Cooper MA. eds. Myles Textbook for Midwives. 15th edition. Edinburgh: Churchill Livingstone, Elsevier, 103-126 Walmesley K. 2000. Managing the OP labour. MIDIRS Midwifery Digest 10(1): 61-2 USAID. Counselling cards for maternal and neonatal health for community health workers WHO. 1998. Care of the Umbilical Cord: A review of the evidence. L.C. Mullany, et al. 2009. Risk of Mortality Subsequent to Umbilical Cord Infection Among Newborns of Southern Nepal. Cord Infection and Mortality. Pediatric Infectious Disease Journal, 28 ( 1). McDonald SJ and Middleton P. “Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes” (Review). The Cochrane Collaboration. USAID. Essential delivery care practices for maternal and newborn health and nutrition Mosha, F. et al. 2005. “Evaluation of the effectiveness of a clean delivery kit intervention in preventing cord infection and puerperal sepsis among neonates and their mothers in rural Mwanza Region, Tanzania”. Tanzania Health Research Bulletin 7: 185-188. Highlights the importance of breastfeeding. 9 39 Support the mother in You can help the baby get the best start in life by supporting This message also encourages guardian breastfeeding straight after the the mother's breastfeeding. Encourage the mother to support, which may make breastfeeding birth. Her first, creamy milk is the breastfeed her baby whenever he wants. Her milk is perfect easier for the mother. best food for the baby. He needs nothing else. for him. It will help him grow strong. The mother’s body knows exactly how to care for her new baby. She will make just the right amount of milk for him. As the baby grows, her milk will change to suit her baby. The thick, creamy milk she makes first is perfect for her newborn. You don't need to give the baby anything else. The mother's milk will be enough for his first six months. Giving him honey, ghee or water could be harmful. Explain this to the family. The WHO recommendation is to put newborn babies to the breast within the first hour of life. We have said 'straight after the birth' to allow for cultures who have a different understanding of time. If the birth is clinic-based or clocks are commonly used, please amend to 'within one hour of the birth.' By supporting breastfeeding, you will also be helping the mother. Breastfeeding will help her to recover from the birth, and help her to delay having another baby. Having a baby too soon can lead to a weak or early baby. If you want to do one good thing for the baby this week, explain the benefits of exclusive breastfeeding to the family. Referencing American Academy of Pediatrics. 2004. Breastfeeding and the Use of Human Milk. Pediatrics 115:2. 496-506 UNICEF and WHO. 2009. SECTION 3: BREASTFEEDING PROMOTION AND SUPPORTIN A BABY-FRIENDLY HOSPITAL: A 20-HOUR COURSE FOR MATERNITY STAFF. WHO.2011. Essential Nutrition Actions: Improving Maternal-Newborn Infant and Young Child Health and Nutrition. WHO.2010. WHO Technical Consultation on Postpartum and Postnatal Care. WHO.2003. Global Strategy for Infant and Young Child Feeding. WHO. 2002 NUTRIENT ADEQUACY OF EXCLUSIVE BREASTFEEDING FOR THE TERM INFANT DURING THE FIRST SIX MONTHS OF LIFE. WHO.2001. REPORT OF THE EXPERT CONSULTATION ON THE OPTIMAL DURATION OF EXCLUSIVE BREASTFEEDING. http://www.who.int/mediacentre/factsheets/fs290/en/ http://www.who.int/making_pregnancy_safer/countries/soa.pdf DH. 2007. Maternity matters. London: Department of Health www.dh.gov.uk [pdf file, accessed September 2011] NCCWCH. 2008. Antenatal care: routine care for the healthy pregnant woman.National Collaborating Centre for Women's and Children's Health, Clinical guideline. London: RCOG Press. www.nice.org.uk [pdf file, accessed September 2011] Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Khan, Wojdyla et al (2006). 'WHO analysis of the causes of maternal death: a systematic review', Lancet, 367:1066-74 Three quarters of all newborn deaths occur 9 40 You and the family need to know You can help keep the baby safe by looking out for signs of the signs of early illness: a fever, illness. Newborns can get ill very quickly. It is best to get them in the first week of life. Up to two-thirds of newborn deaths can be prevented if unresponsiveness and vomiting treated straight away. known, effective health measures are mean the baby needs help at the provided at birth and during the first week of life. (WHO. 2005, The Lancet’s Newborn clinic. Take the baby to the clinic fast if you spot any of these signs: Survival Series 2004 and UNICEF 2008). Her skin, face, eyes, urine, palms or soles of her feet turn yellow in her first day of life. The baby refuses feeds, cries constantly or cries strangely. The baby has fits, is lethargic or has bluish skin or nails. The baby wheezes, grunts or breathes quickly. She vomits after feeding for over a day. She has a swollen stomach. She has a red, smelly cord stump. Or if she has a fever. If you want to do one good thing for the baby this week, discuss these signs of newborn illness with the family. References Chowdhury, H., Thompson, S., Ali, M., Alem, N., Yunus, M., & Streatfield, P. (2011). Care seeking for fatal illness episodes in Neonates: a population-based study in rural Bangladesh. BMC Pediatrics . Opiyo and English. 2011. What clinical signs best identify severe illness in young infants aged 0-59? A systematic review. Arch Dis Child 96: 1052-59. USAID. Counselling cards for maternal and neonatal health for community health workers Warren. C. (2010) 'Care of the newborn: Community perceptions and health seeking behavior', Ethiop. J. Health Dev. 2010;24 Special Issue 1 WHO, UNICEF. 2009. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children. USAID. 2003. Immunization Essentials: A Practical Field Guide http://www.who.int/immunization/documents/positionpapers/en/ http://www.who.int/mediacentre/factsheets/fs290/en/ http://www.who.int/making_pregnancy_safer/countries/soa.pdfDH. 2007. Maternity matters. London: Department of Health www.dh.gov.uk [pdf file, accessed September 2011] Maternal and Neonatal Health Program. 2001. Birth preparedness and complication readiness: A matrix of shared responsibilities. USAID. Lancet. 2006. The Lancet Neonatal series. WHO (2006), Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice http://whqlibdoc.who.int/publications/2006/924159084X_eng.pdf?ua=1 WHO/UNICEF joint statement: Postnatal 9 41 Make sure the mother gets a After the birth, make sure the mother and her baby get care visits for facility birth on Day 3 and 7 of check-up after the birth. Staff will regular check-ups at the clinic. newborn's life check her health and give the baby vaccines to protect against disease. Check-ups after the birth are just as importance as the ones during the mother's pregnancy. Clinic staff will be able to check that both mother and baby are doing well. PNC visits for home births: Days 1, 3 and 7 of newborn's life. Adjust to fit local conditions. If the mother had her baby at the clinic, she will need to get a check-up twice in the first week of her baby's life. If she had Appropriate home care and timely treatment of complications for newborns' identified as a key strategy in tackling MDG 4. (WHO) her baby at home, she will need three visits in the first week. Some clinics offer home visits. Ask a health worker if this is available in your area. If home visits aren't possible, make sure that the mother and her baby have the time and money to visit the clinic. Find someone to go with them, too. By doing this, you will be helping to keep both mother and baby safe and healthy. If you want to do one good thing for the baby this week, tell the mother why she must visit the clinic after the birth. References Chelmow. D. 2011. Postpartum Haemorrhage: Evidence. Clinical Evidence. 04:1410 1-101 S. Fawcus et al. 2011. Management of Postpartum Haemorrhage. SAJOG. 17:2 Hum Lact. J. 1995. Infant Insufficient Milk Syndrome Associated with Maternal Postpartum Haemorrhage. International Lactation Consultant Association. 11:2 Hutton.E. et al. 2007. Late vs Early Clamping of the Umbilical Cord In Full Term Neonates. JAMA. 297:11 1241-1252 Lombaard. H. 2009. Common Errors and Remedies in Managing Postpartum Haemorrhage. Best Practice & Research Clinical Obstetrics and Gynaecology 23 317–326 Royal College of Obstetricians and Gynacologists. 2009. Prevention and Management of Postpartum Haemorrhage. Green Top Guideline 52 1-24 Sanghvi. H. 2006. Preventing Mortality from Postpartum Haemorrhage in Africa. Uganda Conference Report. Opiyo and English. 2011. What clinical signs best identify severe illness in young infants aged 0-59? A systematic review. Arch Dis Child 96: 1052-59. USAID. Counselling cards for maternal and neonatal health for community health workers Chowdhury, H., Thompson, S., Ali, M., Alem, N., Yunus, M., & Streatfield, P. (2011). Care seeking for fatal illness episodes in Neonates: a population-based study in rural Bangladesh. BMC Pediatrics 11:88. WHO, UNICEF. 2009. WHO child growth standards and the identification of severe acute malnutrition in infants and children. Charlotte, W. “Care of the newborn: Community perceptions and health seeking behavior”. Ethiop. J. Health Dev. 2010;24 Special Issue 1 UNICEF. 2009. Taking Evidence to Impact: Making a Difference for Vulnerable Children Living in a World with HIV and AIDS. WHO, UNICEF. 2009. Home visits for the newborn child: a strategy to improve survival. WHO. 2010. WHO Technical Consultation on Postpartum and Postnatal Care. 9 42 Make sure the mother rests and Once the baby is here, the mother will need time to heal. You Taking time to rest and relax was urged in many midwife messages from a midwife eats well after the birth. This will can help her to do this. convention in Durban. Not getting enough help her heal. If she is faint or dizzy, rest can lead to complications due to get her help at the clinic. Make sure the mother does not do any physical work. She exhaustion and dehydration. will be feeling sore and tired. Physical work can also cause her to bleed more. Ask other family members to do this work. Nearly 34% of maternal deaths in Africa Give the mother your support and encouragement, too. Encourage her to keep breastfeeding. She may find it hard at first, and will need your support. and more than 30% in Asia are due to PPH. (MCHIP-USAID) Also make sure that the mother eats well. Good food will give her the strength and energy to care for her baby. Make sure the family has plenty of fresh fruit, vegetables, meat, lentils, peas and beans ready. These foods will give her plenty of goodness. If you think that the mother is not recovering well, or if she is dizzy or faint, take her straight to the clinic. She may be bleeding heavily. If you want to do one good thing for the baby this week, make sure there is lots of healthy food ready to feed the mother after the birth. References World Health Organization. 2010. WHO Technical Consultation on Postpartum and Postnatal Care. World Health Organization. 2007. WHO Recommendations for the prevention of Postpartum Haemorraghing. Nice. 2010. Weight management before, during and after pregnancy. National Institute for Health and Clinical Excellence. Public health guidance 27. NICE. 2006. Routine postnatal care of women and their babies. National Institute for Health and Clinical Excellence, Clinical guideline, 37. London: NICE. USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. Hill M. 2009. Development week by week. University of New South Wales Embryology. embryology.med.unsw.edu.au [Accessed August 2009] Medline Plus Medical Encyclopedia. www.nlm.nih.gov McGrail A, Metland D. 2004. Expecting: everything you need to know about pregnancy, labour and birth. London: Virago, 28 Medline. 2009. Fetal development. Medline Plus Medical Encyclopedia. www.nlm.nih.gov Visembryo. 2006. Pregnancy timeline. The Visible Embryo Baby Week Newborn Newborn Newborn Newborn SMS Message Make sure the baby gets his mother's first milk. It is full of goodness. If he refuses to eat or has difficulty breathing, go to the clinic. Check the baby for signs of illness. His tummy, hands and feet should be warm. If he's hot, cold, or bluish, get him to the clinic. The baby's cord stump must be kept clean, dry and uncovered. If there's pus or redness, wash with clean water. Take the baby to the clinic. Babies need warmth. Make sure the mother holds her baby naked on her chest covered by a blanket. Cold feet means the baby need more layers. Audio message A newborn baby and his mother will need lots of care. Make sure the mother and the baby see the health worker at least twice this week. The baby’s cord stump needs a lot of care. Before touching the baby’s cord, the mother should wash her hands to keep germs away. She can then sponge the cord stump with clean water and leave it uncovered to dry. A moist cord can get infected. The cord will fall off by itself after about a week. The mother should keep the navel clean once this happens. If the cord gets infected, it will be swollen, red or smelly. The baby should be taken to the clinic. Also take the baby to the clinic if you spot these signs of illness: The baby has a fit, is floppy, or has bluish skin or nails, He is wheezing or breathing quickly, He is very hot or very cold, He has swollen or sunken areas on his head, Partner Notes Three quarters of all newborn deaths occur in the first week of life. Up to two-thirds of newborn deaths can be prevented if known, effective health measures are provided at birth and during the first week of life. (WHO. 2005, The Lancet’s Newborn Survival Series 2004 and UNICEF 2008). If the practice is to give an antiseptic on the cord stump, it’s important to let the mother know that nothing else should be put on. If it is common practice to give newborns eye drops, please mention here. In some countries (such as Senegal), a mother gets Vitamin A after birth before she goes back home from the health facility. Please add this if applicable in your target area. Please choose which term is most applicable (hospital / clinic / health centre). Use the local term for ‘health worker’ WHO/UNICEF joint statement: Postnatal care visits for facility birth on day three and seven of newborn's life. PNC visits for home births: days one, three and seven of newborn's life. He is crying non-stop or crying strangely, He is feeding poorly, He is not passing urine six to eight times a day. If you want to do one good thing for the baby this week, look out for signs of illness. References World Health Organization. 2010. WHO Technical Consultation on Postpartum and Postnatal Care. World Health Organization. 1998. Maternal and Newborn Health Safe Motherhood. Care of the Umbilical Cord: A review of the evidence. World Health Organization. 2006. Infant and Young Child Feeding: An Integrated Course. WHO Technical Consultation. 2004. ‘Towards the development of a strategy for promoting optimal fetal growth’, Report of a meeting (draft), World Health Organization, Geneva. UNICEF. 2004. Low Birth Weight: Country, Regional and Global Estimates; Geneva. National Neonatology Forum of India- WHO Collaborating Centre for Training and Research. 2005. Teaching Aids on Newborn Care. New Delhi. Opio, N., & English, M. (2011). What clinical signs best identify severe illness in young infants aged 0–59 days in developing countries? A systematic review . Arch Dis Child ,1052–1059. Chowdhury, H., Thompson, S., Ali, M., Alem, N., Yunus, M., & Streatfield, P. (2011). Care seeking for fatal illness episodes in Neonates: a population-based study in rural Bangladesh. BMC Pediatrics. USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. WHO (2006), Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice http://whqlibdoc.who.int/publications/2006/924159084X_eng.pdf?ua=1 Three quarters of all newborn deaths occur 1 Keep the baby off the ground, Some babies get a yellowish tinge a few days after they are born. in the first week of life. Up to two-thirds of away from direct sunlight. If his This can be in their skin, eyes, urine, or palms and feet. If you spot newborn deaths can be prevented if known, eyes or urine are yellow, this, encourage the mother to breastfeed – her milk will help to effective health measures are provided at breastfeed him more and take wash the yellowness out. birth and during the first week of life. (WHO. 2005, The Lancet’s Newborn Survival Series him to the clinic. 2004 and UNICEF 2008). If the baby was born early, this yellowness may take over a week to go. If she was born full-term, then it will take less time. If the baby is still yellow at the end of this week, take her to the clinic. She may need treatment. Newborn babies often get sticky eyes. Tell the mother to keep them clean. Wash each eye with its own clean cloth and clean water. If the eyes remain sticky, suggest that the mother takes her baby to the clinic. Staff at the clinic are there to make sure the baby is healthy. The baby needs warmth, so keep him wrapped up. But make sure you don’t swaddle him too tightly. If his feet are cold, he needs more layers. Make sure the baby is kept away from direct sunlight. If you want to do one good thing for the baby this week, keep encouraging the mother to breastfeed. References NICE. 2006. Routine Postnatal Care of Women and Their Babies. National Institute of Health and Clinical Excellence. NICE. 2010. Neonatal jaundice. National Institute of Health and Clinical Excellence. National Neonatology Forum of India- WHO Collaborating Centre for Training and Research. 2005. Teaching Aids on Newborn Care. New Delhi. Opio, N., & English, M. (2011). What clinical signs best identify severe illness in young infants aged 0–59 days in developing countries? A systematic review . Arch Dis Child ,1052–1059. Chowdhury, H., Thompson, S., Ali, M., Alem, N., Yunus, M., & Streatfield, P. (2011). Care seeking for fatal illness episodes in Neonates: a population-based study in rural Bangladesh. BMC Pediatrics. USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. WHO (2006), Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice http://whqlibdoc.who.int/publications/2006/924159084X_eng.pdf?ua=1 In South Africa, postpartum haemorrhage 2 If you see the mother dizzy, weak The mother’s body went through many changes whilst she was (PPH; excessive bleeding after birth) is the and sick, she may be bleeding pregnant. She now needs time to recover and regain her strength. third most common cause of death. Main heavily. Take her to the clinic Make sure she has lots of healthy meals. This will help her get causes of mortality were due to lack of immediately. She needs medical stronger. skilled help and a failure to prevent haemorrhage from occurring. In India 17% of help. maternal deaths are due to PPH, making it The mother will bleed for a time after the birth. Keep encouraging the leading cause of maternal deaths. WHO her to breastfeed. Breastfeeding will help prevent the mother from 2010. losing too much blood. Make sure she has time to rest. Moving around too much could make her bleed more. If she feels dizzy and faint, she may be bleeding heavily. Heavy bleeding is a serious problem. Get her to a clinic quickly. She needs immediate help. If the mother has a fit, she needs help quickly. A fit needs urgent treatment. Where the prevalence of anaemia in pregnancy is over 40%, advise the woman to continue the prophylaxis for three months in the postpartum period (Department of Making Pregnancy Safer 2006) Ask the mother to look out for signs of infection. She needs to go to the clinic if she has stomach pain, a fever or chills, or if she has a smelly discharge. Help her get to the clinic quickly. She may need to continue taking iron pills for another 3 months. Ask her to find out at the clinic if she needs to. If you want to do one good thing for the baby this week, make sure the mother gets plenty of rest. References NICE. 2006. Routine Postnatal Care of Women and Their Babies. National Institute of Health and Clinical Excellence. USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. WHO (2006), Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice http://whqlibdoc.who.int/publications/2006/924159084X_eng.pdf?ua=1 WHO. (2012). Guideline: Daily iron and folic acid supplementation in pregnant women. http://apps.who.int/iris/bitstream/10665/77770/1/9789241501996_eng.pdf?ua=1 [Accessed on 21 May 2014] When a baby suckles ineffectively, transfer of See how much the baby has grown The baby needs lots of care from the mother and the whole family 3 milk from mother to baby is inefficient. As a on breastmilk alone. He needs to grow strong and healthy. result: the breast may become engorged, or nothing else, not even water. Tell may develop a blocked duct or mastitis his mother to feed him 8-10 times Encourage the mother to breastfeed her baby as much as he wants. because not enough milk is removed; a day. consequently the baby’s intake of breastmilk Breastmilk is the best food for the new baby. It will help him get may be insufficient, resulting in poor weight stronger. If the baby is feeding eight to 10 times a day, the mother gain. WHO Infant and Young Child Feeding can be sure that he is getting enough milk. 2006 Encourage the mother to let her baby feed at the breast for as long as he wants. The longer the baby feeds, the more rich hind milk he will get. The hind milk helps the baby gain weight and grow bigger. Make sure the baby is given nothing else, not even water. Learning to breastfeed can take time. The mother may have problems. Ask her to talk to her health worker. The health worker will be able to show the mother some techniques to feed her baby well. If you want to do one good thing for the baby this week, ask the mother to talk to her health worker about any breastfeeding problems. References World Health Organization. 2010. WHO Technical Consultation on Postpartum and Postnatal Care. World Health Organization. 2003. Kangaroo Mother Care: A Practical Guide. MCHIP. 2008. Community-Based Care for Low Birth Weight Newborns: The Role of Community Skin-to-Skin Care. Washington, DC., http://www.mchip.net/sites/default/files/KMC_Meeting_Report_08-25-08.pdf USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. 4 Check how many nappies the baby wets each day. If it's less than 6-8 a day, it means he needs more milk. Breastmilk is all he needs. The mother may worry that she is not making enough milk to feed her baby, or that her baby is not feeding well. Reassure her by looking out for these three signs that show that her baby is feeding well. One; ask the mother to count the number of wet nappies her baby has. Her baby should make six to eight wet nappies a day. This shows that her baby is drinking enough milk. If babies do not wear nappies, change accordingly. WHO recommendation: Exclusive breastfeeding for 6 months. Introduction of solids at 6 months + continued breastfeeding for 2 years. Globally less than 40% of infants under six months of age are exclusively breastfed. Adequate breastfeeding support for mothers and families could save many young lives. WHO Factsheet 2011 Two; after a feed, look at the baby. If her tummy is rounded, she seems settled and has a healthy colour, then she is getting plenty of milk. Three; the mother should feed whenever the baby wants. This will be about eight to ten feeds a day. If the baby is refusing feeds or has lots of short feeds, then there may be problem. If you spot these signs, help the mother get her baby to the clinic. The staff there will be able to check if the baby is ill. If you want to do one good thing for the baby this week, ask the mother to count how many wet nappies her baby makes. References World Health Organization. 2006. Infant and Young Child Feeding: An Integrated Course. 5 Remind the mother to take her baby for his vaccinations this week. Vaccines help protect the baby from disease. They will keep Babies can get ill easily. They are not as strong as adults. Vaccines protect the baby against diseases like TB and polio. Make sure the baby is taken to the clinic for his vaccines. This week, Immunisation prevents three million child deaths each year. Expanded Programme for Immunisation (EPI) is part of WHO strategy to tackle MDG 4 (WHO) him safe. he is due for his first dose of a vaccine which will help protect him against diphtheria, tetanus, whopping cough and hepatitis B. This vaccine will be given as an injection. Over the following years, see that the baby gets all the doses of the vaccines. The vaccines can’t cure the baby once he has these diseases, so he needs to get them on time. Make sure the mother is able to take the baby to the clinic for his vaccines. Encourage her to take her baby even if he is ill. Explain to her how it will help keep her baby safe. If she is very worried, you could offer her extra support by going with her. Vaccinations at 6 weeks: Bangladesh: DTP, Hib, HepB, OPV India: DTP, HepB, OPV South Africa: DTP, Hib, IPV, OPV, Hep B, Rotavirus, Pneumo conj In some countries (eg Senegal), mothers are given Vitamin A and deworming treatment postpartum. Please suggest these if applicable in your target area. Adapt to vaccine schedule in each country. If you want to do one good thing for the baby this week, make sure he is taken to the clinic to get his vaccine. References USAID. 2003. Immunisation Essentials: A Practical Field Guide. MCHIP/USAID. (n.d.). Immunisation Ready Reference for Health Workers. Retrieved November 7, 2011, from MCHIP: http://www.mchip.net/node/510 WHO. 2006. Tetanus vaccine: WHO Position Paper. Weekly epidemiological record 20. USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. Summary of WHO position papers – recommended routine immunisations for children (Tables 1 & 2) http://www.who.int/immunization/policy/Immunization_routine_table1.pdf http://www.who.int/immunization/policy/Immunization_routine_table2.pdf Thrush is common in young babies. This 6 Does the baby have white Some breastfeeding women and their babies get an infection called message empowers the guardian with patches inside his mouth? It thrush. Thrush can affect the mother’s nipples and her baby’s practical information and advice. could be a yeast infection. Both mother and baby may need treatment at the clinic. mouth. The infection can be passed back and forth between them. If the baby has thrush, he will have small, white patches inside his mouth. Thrush will usually affect his tongue and the sides of his mouth. If the patches are only on his tongue, it is possible that this may just be left-over milk. A baby with thrush may pull away when feeding. This is because his mouth is sore. If you notice these signs, take both the mother and her baby to the clinic. Clinic staff will be able to give the baby and his mother the treatment they need. Encourage the mother to continue breastfeeding. Her breastmilk is still full of goodness. If you want to do one good thing for the baby this week, talk to the mother about the signs of thrush. Research UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction. Family planning: the unfinished agenda. The Lancet. 2006. The Lancet sexual and reproductive series. WHO. 2005. Report of a WHO Technical Consultation on Birth Spacing USAID/ACCESS. 2008. THE LACTATIONAL AMENORRHEA METHOD (LAM): A Postpartum Contraceptive Choice for Women Who Breastfeed. 7 A healthy baby is curious, gains weight and turns towards sounds. If the mother is worried about her baby, she can get help at the clinic. It is easy to worry about a new baby. Here are a few signs of a happy and healthy baby. Share them with the mother. A healthy baby is a curious one. It is a good sign if the baby notices when you are talking to him, or looks at something you are holding. Sometimes he may be quiet – this shows that he is watching what is going on around him. You may notice that he is starting to get heavier to pick up! This shows that he is getting enough to eat. A healthy baby feeds well. If the baby does fall ill, tell the mother that it is best to take him to the clinic for the right treatment, and not to a traditional healer. Cures offered by these healers will not always be safe for a baby. Babies develop at different speeds. Encourage the mother to take the baby to the clinic for regular check-ups. The health workers will monitor the baby’s development. If you want to do one good thing for the baby this week, look out for the signs of a healthy baby. References A A Opaneye. 1998. “Traditional medicine in Nigeria and modern obstetric practice: need for cooperation”, Central African Journal of Medicine, 44(10):258-61. Chuang, Chao-Hua et al. 2006 . “Herbal Medicines Used During the First Trimester and Major Congenital Malformations: An Analysis of Data from a Pregnancy Cohort Study”, Drug Safety, Volume 29, Number 6, pp. 537-548(12). Thein , Koh et al. 1995. “Risk factors for birth defects in Singapore: a case control study”. Annals, Academy of Medicine, Singapore. 24(3):421-7. Opio, N., & English, M. (2011). What clinical signs best identify severe illness in young infants aged 0–59 days in developing countries? A systematic review . Arch Dis Child ,1052–1059. Chowdhury, H., Thompson, S., Ali, M., Alem, N., Yunus, M., & Streatfield, P. (2011). Care seeking for fatal illness episodes in Neonates: a population-based study in rural Bangladesh. BMC Pediatrics . 8 See that the mother gives her Here are some ways to make sure the baby continues to grow bigger If soap is not readily available, mention where the mother can get some from, or baby ONLY breastmilk and no and stronger. alternatives she could use. water. Water can carry germs and make the baby unwell. Breastmilk One; keep encouraging the mother to breastfeed. Remind her that is safe. her milk is giving her baby all she needs to grow. It is also helping to protect the baby from illness and disease. Two; make sure that the baby has all of her vaccinations at the right time. The vaccines will help to protect her from lots of diseases such as polio. Talk to a health worker about what vaccinations the baby still needs. Three; make sure the baby's home is clean and that the whole family washes their hands after using the toilet, touching animals and changing nappies. Hand washing with plenty of soap and clean water helps to keep germs away. Encourage the mother to wash her hands before she starts cooking. Tell her to check that food is washed before it is prepared, and that utensils and plates are washed well after use. All this will keep the whole family healthy. If you want to do one good thing for the baby this week, share these tips with the mother. References USAID. 2006. Immunisation Essentials: A Practical Field Guide 2003 World Health Organization. Infant and Young Child Feeding: An Integrated Course. UNICEF. 2011. Water, Sanitation and Hygiene Annual Report 2010 WHO. 2000. Food borne disease: a focus for health education. WHO. 2003. Healthy Villages – A Guide for Communities and Community Health Workers. WHO. 2001. Water for Health: Taking Charge. World Health Organization. 2006. Infant and Young Child Feeding: An Integrated Course. USAID. 2003. Immunisation Essentials: A Practical Field Guide WHO. 2001. Water for Health: Taking Charge. WHO. 2010. Nutrition health topics: exclusive breastfeeding. World Health Organization 9 Breastfeeding can help to delay pregnancy. Encourage the mother to find out from the health worker how it works. Pregnancy and birth are very hard on the mother’s body. She needs time to recover. WHO recommendations: Spacing of two years between the birth of a baby and getting pregnant again. It is best for her to wait two years before she gets pregnant again. This will give her body time to recover and regain the nutrients it has lost. Having a baby too soon will lead to her next child being born early and weak. MCHIP recommendations: three years birth to birth interval. Encourage the mother to wait two years until she tries for another baby. Explain to her family why this will be best. Fit to the contraceptive practices in your country. Breastfeeding is the best way right now for the mother to space her pregnancies. Encourage her to breastfeed her baby whenever the baby wants until her baby is six months old. No other food should be fed to the baby. Doing this will help to delay the mother's period and prevent her from getting pregnant. You can help the mother by supporting her in exclusively breastfeeding her baby until she is six months old. If you want to do one good thing for the baby this week, explain to the mother’s family why waiting two years for another baby is best. Please choose the recommendation followed by your country. Lactation Amenhorrea Method (LAM) is an effective method of family planning and recommended in many countries. If it is not recommended in your area, please remove. References WHO/UNICEF. 2009. Diarrhoea: why children are still dying and what can be done MOST. 2005. Diarrhoea Treatment Guidelines. 10 See that the mother eats meat, fruits and vegetables and takes some time every day to rest. This will help keep her strong for her baby. Eating well helps the mother gain back her strength. A breastfeeding mother needs iron. She may need to carry on taking her iron pills for another 2 months. Make sure she asks her health worker if she needs them. The mother can also get iron from meat, fish, lentils, beans, peas and eggs. See that she has enough of these foods. Coffee, tea and milk may prevent the mother absorbing the iron in these foods. Encourage her to limit these drinks to once a day. These drinks can be had two hours before or after having iron. Towards the end of her pregnancy, the mother had to eat a couple of extra mouthfuls at each meal. This gave her added strength. Whilst she is breastfeeding, she will still need this added food. Make sure she eats two extra mouthfuls at every meal. Please suggest food items that are easily available in your area. In some countries (such as Senegal), mothers are given Vitamin A and deworming treatment postpartum. Please suggest these if applicable in your target area. Adjust if iron and folic acid are given postpartum. Delete instructions to eat meat and fish in vegetarian communities. Iron deficiency anaemia is among the most important contributing factors to maternal and child mortality, and to the global burden of disease. UNICEF/WHO 1999 If you want to do one good thing for the baby this week, make sure the mother asks her health worker about iron and folic-acid pills. References Nice. 2010. Weight management before, during and after pregnancy. National Institute for Health and Clinical Excellence. Public health guidance 27. UNICEF/WHO. 1999 Prevention and Control of Iron Deficiency Anaemia in Women and Children. World Health Organization. 2006. Infant and Young Child Feeding: An Integrated Course. World Health Organization/ Food and agriculture organiztion. 2006. FAO/WHO technical consultation on national food-based dietary guideline 11 Crying is normal for babies, but if the baby is crying non-stop or cries strangely, get him checked All babies cry – it is the only way they can communicate. Some babies may cry more than others! If the baby does not wear nappies, plus adjust accordingly. at the clinic. He may be ill. By knowing why the baby cries, the mother can help soothe and settle him. There are many reasons why babies cry. Hunger is sometimes the reason. Encourage the mother to try feeding him. She may find that her baby quiets once his tummy is full of milk! This message gives the guardian and the mother practical tips. This will boost their confidence in their ability to care for the baby. Another reason may be that the baby is uncomfortable. Ask the mother to check how many layers of clothing he is wearing. Usually he needs just one more layer than you. Ask her to check that none of his clothes are too tight or that they are rubbing him. Changing his nappy as soon as it is soiled also helps. This will keep him feeling clean and dry. Sometimes, all the baby wants is a cuddle. Encourage the mother to wrap the baby in a blanket and cuddle him. This will make him feel snug and secure. Singing to him and rocking him gently may also help him to settle. Remind her not to swaddle him to tightly when she wraps him. If these don't work, take the baby to the clinic for help. If you want to do one thing for the baby this week, share these tips with the mother. References St James-Roberts. 2008. Infant crying and sleeping: helping parents to prevent and manage problems. Primary Care 35(3):547-67 NCCPC. 2006. Postnatal care: Routine postnatal care of women and their babies. National Collaborating Centre for Primary Care. www.nice.org.uk USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. 12 If the baby has a fever, shivering and rapid breathing, take him and his mother to the clinic. The baby may be ill. Keeping a baby healthy can be hard work. Sometimes she will be sick. But by looking out for signs of illness you can help her get treatment fast. Here are three signs you can look out for. 'Appropriate home care and timely treatment of complications for newborns' identified as a key strategy in tackling MDG 4 Source: WHO Factsheet One; a fever is a sign of infection. If the baby is feverish she will need treatment at the clinic. You can check the baby’s temperature by feeling her tummy, hands and feet. They should all be warm, not too hot or cold. Two; a baby who cries non-stop could be ill. If the mother says that her baby’s pattern of crying has changed, or that it sounds strange, take the baby to the clinic for a check-up. It is better to be safe, than sorry. Three; a baby who starts refusing feeds is probably unwell. If the mother says that her baby is not feeding as much as normal, help her to get her baby checked at the clinic. A healthy baby will feed well. If you want to do one good thing for the baby this week, talk to the mother about these signs of illness. References The Lancet. 2004. Executive Summary of Lancet Neonatal Survival Series. World Health Organization. 2010. Countdown to 2015. Opio, N., & English, M. (2011). What clinical signs best identify severe illness in young infants aged 0–59 days in developing countries? A systematic review . Arch Dis Child ,1052–1059. Chowdhury, H., Thompson, S., Ali, M., Alem, N., Yunus, M., & Streatfield, P. (2011). Care seeking for fatal illness episodes in Neonates: a population-based study in rural Bangladesh. BMC Pediatrics . USAID/BASICS/ Ministry of Health, Louga, Senegal. (n.d.). Counseling Cards for Maternal and Neonatal Health. Expressing breastmilk and cup-feeding is 13 The mother can express If the mother is going out without her baby, she won't be able to often a safer alternative than using breastmilk for someone else to breastfeed whenever her baby wants. Instead, she could express commercial milks or other products, if water feed the baby with a spoon. Keep some milk before she leaves. supplies are not clean. expressed milk in a cool place for up to 6 hours. Encourage the mother to try expressing her milk into a clean cup. The milk will stay fresh for up to eight hours. Advise the mother to try expressing milk in the morning when her milk supply is highest. If she struggles, suggest that she puts a cloth soaked in warm, clean water on her breast. This may make it easier to get her milk flowing. She could also try massaging her breasts. The mother may be nervous about leaving her baby, so support her and reassure her that her baby will be well-looked after. This will give her the confidence to go out. If you want to do one good thing for the baby this week, talk to the mother about expressing her milk. References World Health Organization. 2006. Infant and Young Child Feeding: An Integrated Course. WHO/UNICEF. 1993. Breastfeeding counseling: a training course. 14 Ask the mother to put her baby to sleep under an insecticidetreated net. Make sure she keeps a spare net in case one gets damaged. Even though the baby is getting bigger and stronger now, she is still vulnerable to mosquito-borne illnesses like malaria and dengue. But there are ways to help keep her safe. Share these tips with the mother. Mosquitoes breed in stagnant water. Pouring old cooking oil on any puddles or small ponds near the home helps to keep them away. Ask the mother to check inside the home for any vases or bowls full of water. These will need to be emptied. Dark colours also attract mosquitoes. Advise the mother to dress the baby in long, light-coloured clothes. This will help prevent bites. We have suggested asking an NGO for a net. If nets are available elsewhere, please mention this. If Intermittent Preventative Treatment for infants is given in your country, please add information about it. From the end of the neonatal period and through the first five years of life, the main causes of death are pneumonia, diarrhoea and malaria. Source: WHO: Children - reducing mortality. 2011 Make sure that mother and baby sleep under an insecticide-treated net every night. Make sure she keeps a spare net in case one gets damaged. If you want to do one good thing for the baby this week, take these steps to protect her from mosquitoes. References WHO (2013a). World Malaria Report http://www.who.int/malaria/media/world_malaria_report_2013/en/ WHO (2013b). Malaria in Pregnant Women http://www.who.int/malaria/areas/high_risk_groups/pregnancy/en/ Arogundade., E. D. et al. 2011. Relationship between care-givers' misconceptions and non-use of ITNs by under-five Nigerian children. [Online]. Available on: http://www.malariajournal.com/content/10/1/170 [Accessed on 29 January 2014] CDC. 2012. Intermittent Preventive Treatment of Malaria for Pregnant Women (IPTp). [Online]. Available on: http://www.cdc.gov/malaria/malaria_worldwide/reduction/iptp.html [Accessed on 29 January 2014] Doctors without borders., 2012. Malaria. [Online]. Available on: http://www.msf.org.uk/malaria [Accessed on 28 January 2014] East African Community., 2014. Malaria Prevention and Control. [Online]. Available on: http://www.eac.int/health/index.php?option=com_content&id=95%3Amalaria-prevention-andcontrol&Itemid=32 [Accessed on 29 January 2014] Isa AY and Nwobodo EL (2009) 'Awareness and utilization of insecticide-treated mosquito nets among pregnant mothers at a tertiary health institution in north-western Nigeria' Niger J Med. 2009 Apr-Jun;18(2):175-8. http://www.ncbi.nlm.nih.gov/pubmed/19630324 Falade et al. (2005/06). The influence of cultural perception of causation, complications and severity of childhood malaria on determinants of treatment and preventive pathways. Int Q Community Health Education 24 (4). http://www.ncbi.nlm.nih.gov/pubmed/17686690 Morenkeji (2009). Perception and management of Malaria in secondary schools in a Nigerian city. Pakistan Journal of Medical Sciences 25 (3). http://www.pjms.com.pk/issues/aprjun209/article/SC1.html Mwenesi, H., Harpham, T., and Snow, R.W. (1995) Child malaria treatment practices among mothers in Kenya. Social Science and Medicine 40: 1271-1277. Nuwaha (2002). People’s perception of malaria in Mbarara, Uganda. Tropical Medicine and International Health 7 (5) http://onlinelibrary.wiley.com/doi/10.1046/j.1365-3156.2002.00877.x/full NHS., 2013. Can I take Malaria tablets if I am pregnant? [Online]. Available on: http://www.nhs.uk/chq/Pages/2475.aspx?CategoryID=54 [Accessed on 29 January 2014] Nosten., F. and White., N., 2007. Artemisinin-Based Combination Treatment of Falciparum Malaria. [Online]. Available on: http://www.ncbi.nlm.nih.gov/books/NBK1713/pdf/pg181.pdf [Accessed on 28 January 2014] Roll Back Malaria., 2010. Economic costs of malaria. [Online]. Available on: http://www.malariaconsortium.org/userfiles/file/Malaria%20resources/RBM%20Economic%20costs%20of%20malaria.pdf [Accessed on 28 January 2014] Roll Back Malaria., 2012. Annual Report 2012. [Online]. Available on: http://www.rollbackmalaria.org/AnnualReport2012/index.html. [Accessed on 28 January 2014] Rhee M et al. (2005). ' Use of insecticide-treated nets (ITNs) following a malaria education intervention in Piron, Mali: a control trial with systematic allocation of households', Malaria Journal 2005, 4:35 doi:10.1186/1475-2875-4-35 http://www.malariajournal.com/content/4/1/35 Sangaré LR, Weiss NS, Brentlinger PE, Richardson BA, Staedke SG, et al. (2012) Determinants of Use of Insecticide Treated Nets for the Prevention of Malaria in Pregnancy: Jinja, Uganda. PLoS ONE 7(6): e39712. doi:10.1371/journal.pone.0039712 http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0039712 Welch K and Fuster M (2012) 'Barriers in access to insecticide treated bed nets for malaria prevention: An analsyis of Combodian DHS data', J Vector Borne Dis. 2012 Mar;49(1):1-7. http://www.ncbi.nlm.nih.gov/pubmed/22585235 WHO., 2003. Fixed-Dose Combinations for HIV/AIDS, Tuberculosis, and Malaria. [Online]. Available on: http://apps.who.int/medicinedocs/en/d/Js6172e/ [Accessed on 29 January] WHO., 2012a. 10 Facts on Malaria in Africa. [Online]. Available on: http://www.afro.who.int/en/clusters-a-programmes/dpc/malaria/features/2287-10-facts-on-malaria-in-africa.html [Accessed on 28 January 2014] WHO., 2012b. Malaria. [Online]. Available on: http://www.salute.gov.it/imgs/C_17_pubblicazioni_1879_ulterioriallegati_ulterioreallegato_0_alleg.pdf [Accessed on 28 Janaury 2014] WHO., 2012c. Intermittent Preventive Treatment of malaria in pregnancy using Sulfadoxine-Pyrimethamine (IPT-p-SP). [Online]. Available on: http://www.who.int/malaria/iptp_sp_updated_policy_recommendation_en_102012.pdf [Accessed on 29 January 2014] WHO. (2009). Dengue – Guidelines for diagnosis, treatment, prevention and control. http://whqlibdoc.who.int/publications/2009/9789241547871_eng.pdf?ua=1 [Accessed on 23 May 2014] WHO. 2014. Climate change and infectious diseases. http://www.who.int/globalchange/publications/climatechangechap6.pdf [Accessed on 23 May 2014] Diarrhoea remains the second leading cause Encourage the family to stay 15 Washing hands is one of the best and easiest things to do to keep of death among children under five globally. healthy by washing their hands. Set germs away from the baby so he doesn't get diarrhoea or other Nearly one in five child deaths – about 1.5 up a washing stand with soap and infections. million each year – is due to diarrhoea. It kills water near where food is prepared. more young children than AIDS, malaria and Ask the mother and the rest of the family to make it a habit to wash measles combined. Source: UNICEF/WHO 2009. their hands with clean water and soap. They should wash their hands after using the toilet, after touching animals or changing nappies. Tell them to wash their hands before preparing food, too. Toilets and latrines can be full of germs if they are not kept clean. See that they are cleaned often. This will help to prevent sickness. Encourage the mother to wash her hands before she expresses any milk. The milk then needs to go in a cup that has been cleaned with boiling water. If the baby has loose and watery stools, he may have diarrhoea. Encourage the mother to breastfeed her baby. Breastmilk will help him get better. If his diarrhoea lasts over a day, take the mother and her baby to the clinic for ORS and zinc treatment. If you want to do one good thing for the baby this week, set up a wash stand in your home. References UNICEF. 2012. Diarrhoea. http://www.unicef.org/health/index_43834.html. [Accessed on 3 June 2014] WHO. 2011. Zinc supplementation in the management of diarrhoea. http://www.who.int/elena/titles/bbc/zinc_diarrhoea/en/. [Accessed on 3 June 2014] WHO. 2013. Diarrhoeal Disease. http://www.who.int/mediacentre/factsheets/fs330/en/ [Accessed on 3 June 2014] WHO recommendations: Spacing of 2 years The baby still needs only 16 Friends, family or the mother herself may have started thinking between birth of baby and getting pregnant breastmilk. The mother can make about weaning the baby onto solids. But encourage the mother to again as much milk as the baby needs. If he needs more he suckles more. only feed her baby breastmilk until her baby is six months old. Here are three reasons why. One; the mother’s milk is still full of goodness that will protect the baby from illness. It has all the fats, minerals and vitamins the baby needs to keep growing. Other foods, including water, can make the baby ill. Two; the mother’s body knows exactly what the baby needs and can change the amount and type of milk it makes. This means that the baby will always have what she needs. Three; breastfeeding is a natural family planning method. By feeding MChip recommendations: 3 years birth to birth interval. Please choose recommendation followed by your country. her baby only breastmilk and nothing elsefor six months, the mother can help to delay her period. This will help prevent pregnancy. It is best to space babies as it will give the mother time to recover and care for her baby. Two years is the ideal time. If you want to do one good thing for the baby this week, support the mother in continuing to breastfeed. References World Health Organization. 2005. Report of a WHO Technical Consultation on Birth Spacing. WHO/UNICEF. 1993. Breastfeeding counseling: a training course. WHO. 2006. Infant and young child feeding counselling : an integrated course. 17 Ask the mother to put the baby to sleep on her back. It's the safest way as it helps the baby breathe. The baby should be sleeping better, although he still might not be sleeping through the night. There are ways to help the baby sleep better. Share these tips with the mother: One; make sure he is comfortable and safe. He should be wearing just one more layer than you. In the summer he will only need a light cover, while in winter he will be nice and warm with a thicker blanket. His tummy, hands and feet shouldn’t be too hot or cold. Two; put the baby to sleep on his back without a pillow. This will help him to breathe through the night. Also, see that the mattress he lies on fits the bed well so that he can’t fall down the sides. The baby will be perfectly fine sleeping with his mother if she prefers. She will just need to be careful. Three; make sure the baby sleeps under an insecticide-treated net every night. Find out where the mother can get one. If you want to do one good thing for the baby this week, put the baby to sleep on his back under an insecticide-treated net. References Sudden Infant Death Syndrome (SIDS) may not be recognised and data may not be collected in many low-resource settings. This message will help to ensure that the baby sleeps safely every night. Creery D and Mikrogianakis A. 2006. Sudden infant death syndrome. BMJ Clinical Evidence. clinicalevidence.bmj.com DH. 2009. Reduce the risk of cot death. Department of Health. www.dh.gov.uk[Accessed March 2009] FSID. 2010. Cot death facts and figures. Foundation for the Study of Infant Deaths. fsid.org.uk [Accessed March 2011] FSID. 2009a. Babyzone: how to keep your baby safe and healthy. Foundation for the Study of Infant Deaths. FSID. 2009b. What is cot death? Foundation for the Study of Infant Deaths. GP Notebook. n.d. SIDS Risk factors. www.gpnotebook.co.uk NHS. 2010. Sudden infant death syndrome. NHS Choices, Health A-Z.www.nhs.uk [Accessed March 2011] Patient UK. 2009. Reducing the risk of cot death. 18 Babies get colds easily. Breastmilk will help her recover. Talk to clinic staff before giving traditional remedies. Some may be harmful. When a baby has a cold she may have a runny nose, a cough and red, watery eyes. A fever, sore throat and earaches are also common. It can be upsetting to see. But there are things you can do to help the mother get her baby feeling happy and healthy again. A cold is a viral infection that affects the nose, throat and sinuses. There are more than 200 different cold viruses. While adults usually have two to four colds a year, children can catch as many as seven to 10. Encourage the mother to breastfeed her. Breastmilk will help to make her strong again. Suggest the mother tries sitting her baby upright when feeding. This will help her to breathe if she has a stuffy nose. Source: NHS Choices 2011 Suggest to the mother to let the baby sleep upright too. She can do this by propping the end of the bed up with pillows or folded blankets underneath the mattress. The mother will need to wipe the baby's nose often. Advise the mother to check with a health worker before giving the baby any traditional medicines. Many babies get colds, but if the baby is very unwell, or has a fever, take her to the clinic. She may need extra treatment. If you want to do one good thing for the baby this week, look out for signs the baby has a cold. References Arroll B. 2008. Common cold. BMJ Clinical evidence. NHS. 2009a. Common cold. NHS Choices, Health A-Z. DH. 2009. Department of Health. Birth to five: Chapter 8 Treating illnesses, infections and injuries. 19 Tell the mother that if the baby has loose, watery stools (diarrhoea) for over a day, he needs clinic treatment and lots of breastfeeds. The baby is growing bigger and stronger every day, but he can still get ill. You can help make sure he is healthy by looking out for these signs. If you can see them, then the baby is healthy and doing well! 'Appropriate home care and timely treatment of complications for newborns' identified as a key strategy in tackling MDG 4 Source: WHO Factsheet A baby who breastfeeds well is a good sign. He will put on weight and grow. Without his mother’s milk he would be small and weak. If the mother wants some time to herself, suggest she express some milk into a clean cup. This way, you can take a turn feeding the baby. Other signs that the baby is doing well are his cheeky personality and his playful nature. If he is curious and enjoys playing and being entertained, then he is full of health! Another good sign is if he is sleeping for about 15 hours a day. He won’t sleep through the whole night, but he will sleep better than he did when he was a newborn. If you want to do one good thing for the baby this week, talk to the mother about these signs of a healthy baby. References WHO. 2006. Infant and young child feeding counseling: an integrated course. 20 Make your home safe. See that there are no small objects on the floor that the baby can put in his mouth. Keep sharp objects out of reach. Now is around the time when babies become very curious. They will start to put lots of things into their mouths. Now that the baby is mouthing objects, you need to be extra careful about what is around the house. Make sure that anything on the floor is too big for him to swallow. If not, put it in a safe place. This will help to prevent choking. Soon, the baby may start teething. This can cause him to drool a lot. It can make his chin very sore. Putting shea butter or coconut oil on Change shea butter and coconut oil if it is not easily available. It is very common for babies to start exploring their world by putting things in their mouths. This message explains why they do this, and also gives useful, practical advice. his chin can help protect his chin and relieve his discomfort. Clean off any drool with a very soft cloth. This will stop his skin from being irritated even more. Sucking on a clean finger can also help relieve the pain of the tooth coming through. If you want to do one good thing for the baby this week, make sure there is nothing on the floor that the baby could swallow. References WHO 2010. Causes of Child Mortality in 2010 BDHF. 2010. Children's teeth British Dental Health Foundation. www.dentalhealth.org CKS. 2009. Clinical topic: teething. www.cks.nhs.uk 21 Having a baby too soon can cause the baby to be born weak. Ask the mother to seek advice at the clinic about family planning methods. Several months have passed since the baby arrived. The family may be thinking about the mother having another baby. But now is still not quite the right time for the mother to fall pregnant again. Encourage them to wait a little longer. If the mother gets pregnant again now, her next baby may be born weak and early. This is because her body won’t have had time to replace all the nutrients it lost during her last pregnancy. WHO recommendations: Spacing of two years between the birth of a baby and getting pregnant again. MChip recommendations: Three years birth to birth interval. Please choose the recommendation followed by your country. Spacing pregnancies by at least two years is the best way of making sure that future babies are born healthy. The ideal way to space babies is by using family planning methods. There are many different options the mother can choose from. Offer her your support and encourage her to talk to a health worker. Perhaps you could go with the mother, too. This will give her greater support. If you want to do one good thing for the baby this week, encourage the mother to talk to a health worker about birth spacing. References UNDP/UNFPA/WHO/World Bank Special Programme of Research Development and Research Training in Human Reproduction. Family planning: the unfinished agenda The Lancet Sexual & reproductive health series. 2006 World Health Organization. 2005. Report of a WHO Technical Consultation on Birth Spacing. WHO recommendation: Exclusive 22 The baby still needs only With the baby growing so fast, both you and the mother may feel breastfeeding for six months. Introduction of breastmilk. Don't be tempted to give him any other foods or liquids until he is six months old. that he is finally ready for solids. But at the moment his mother’s breastmilk is still giving him all he needs. He won’t need solids yet. solids at six months and continued breastfeeding for two years. By waiting a little longer, you and his mother will give him time to get fully ready for solid food. This will make introducing solids much more enjoyable for him. If he can hold his head up when you carry him and he can look around, it is a sign that he ready for solids. Taking an interest in what you eat, and even trying to take some, is another sign. Wait for these signs before feeding him solids. If the mother has questions about feeding her baby solid food, encourage her to ask her health worker. They will give her useful advice. If you want to do one good thing for the baby this week, encourage the mother to breastfeed for another three weeks. References WHO. 2000. Complimentary Feeding: Family Foods for Breastfed babies. WHO. 2006. Infant and young child feeding counseling : an integrated course. 23 When the baby shows interest in your food and can hold his head steady, he may be ready to try mashed foods. Look out for these signs. The mother may now feel that the time is right to have another baby. But it is still best for her to wait until her current baby is two years old. Here are three reasons why she should wait to have another baby. One; having another baby too early can put the mother at risk. Pregnancy can be hard on the mother’s body. She needs plenty of time to recover. Two; waiting two years will mean that the mother has healthier babies. A two year break will give her body chance to store up all the strength and nutrients it needs to help her grow a strong, WHO recommendations: Spacing of two years between the birth of a baby and getting pregnant again. MCHIP recommendations: three years birth to birth interval. Please choose the recommendation followed by your country. healthy baby. If she gets pregnant now, she will be more likely to have an early birth. Three; waiting will give the whole family time to start saving money again. By waiting and saving money for two years, the family will find it easier to afford trips to the clinic and treatment. If you want to do one good thing for the baby this week, talk to the whole family about why it is best for the mother to wait before having another baby. References UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction. Family planning: the unfinished agenda The Lancet Sexual & reproductive health series. 2006 World Health Organization. 2005. Report of a WHO Technical Consultation on Birth Spacing. Diarrhoea remains the second leading cause 24 Are the baby's stools suddenly The baby’s stools are a good way of checking that he is healthy. watery? He may have diarrhoea. Babies produce different amounts of stools. Some breastfed babies of death among children under five globally. Nearly one in five child deaths – about 1.5 Tell the mother to breastfeed him pass stools four times a day or more, while others pass stools every million each year – is due to diarrhoea. It kills more often and check with the other day. Tell the mother to watch what is normal for her baby. more young children than AIDS, malaria and measles combined. UNICEF/WHO 2009. health worker. This way she will be able to tell when something changes. The baby may pass stools at about the same time every day. His stools will be soft and light-coloured, usually yellow. They will also smell slightly sweet. Green and frothy stools mean that the baby is not getting enough of the rich hind milk. If the mother notices this, encourage her to try and feed her baby for longer on one breast. Loose and watery stools mean the baby has diarrhoea. If the mother spots this, she must breastfeed her baby often. If the diarrhoea last more than a day, the mother should take her baby to the clinic for treatment. If you want to do one good thing for the baby this week, ask the mother to keep an eye on her baby’s stools. References BC UK Amir L. 1991. Candida and the lactating breast: predisposing factors. J Hum Lact, 7 (4); 177-181 Horowitz BJ, Edelstein SW et al. 1984. Cited in: Hoover K, 2002. The Link Between Infants' Oral Thrush and Nipple and Breast Pain in Lactating Women www.hooverfam.net [Accessed September 2009] Jones W, Sachs M. 2009. Thrush and breastfeeding. Paisley: The Breastfeeding Network. www.breastfeedingnetwork.org.uk [Accessed September 2009] Rashid S, Collins M, Corner J et al. 1984. Survival of Candida albicans on fabric after laundering.Br J Vener Dis 60; 277 UNICEF. 2012. Diarrhoea. http://www.unicef.org/health/index_43834.html. [Accessed on 3 June 2014] WHO. 2011. Zinc supplementation in the management of diarrhoea. http://www.who.int/elena/titles/bbc/zinc_diarrhoea/en/. [Accessed on 3 June 2014] WHO. 2013. Diarrhoeal Disease. http://www.who.int/mediacentre/factsheets/fs330/en/ [Accessed on 3 June 2014] 'Appropriate home care and timely treatment 25 Look out for signs of illness. If the There are many reasons why babies vomit. They may vomit of complications' identified as a key strategy baby vomits more than 5 times because they have a cold or an infection. They can also vomit after in tackling MDG 4 during a day, go to the clinic. She needs plenty of extra breastfeeds. crying or coughing for a long time. The most likely cause is a stomach virus, which can also cause diarrhoea. Source: WHO Factsheet If the baby is vomiting, she needs plenty of fluids. Encourage the mother to continue breastfeeding her. The milk will help the baby fight off the infection. Advise her to give her baby lots of short feeds. This will give her baby lots of the watery foremilk. If the baby is still vomiting for over a day, or vomits more than five times, she must be taken to the clinic for the right treatment. Help the mother to get to the clinic with her baby. You can help keep the baby and the whole family free from vomiting. Make sure everyone washes their hands before and after eating, and clean the area where the baby plays. Keeping her toys clean will also help. If you want to do one good thing for the baby this week, make sure everyone washes their hands. References NICE. 2009. National Institute of the Health and Clinical Excellence. Diarrhoea and vomiting caused by gastroenteritis: diagnosis, assessment and management in children younger than five years. www.nice.org.uk MOST. 2005. Diarrhoea Treatment Guidelines. 26 Tell the mother breastmilk is still the baby's main source of food, even after he starts eating soft food. It protects him from illness. Let the mother know how important it is to keep breastfeeding her baby. The mother’s breastmilk changes to suit the growing baby. It has changed a lot since he was a newborn. Once he starts eating solids, it will change and adapt again. By continuing to drink his mother’s milk, the baby will get all the nutrients he needs, along with protection from illness. The solid food he eats will give him just a little bit extra on top. The energy needs from complementary foods for infants with “average” breast milk intake in developing countries (WHO/UNICEF, 1998) are approximately 200 kcal per day at 6-8 months of age, 300 kcal per day at 9-11 months of age, and 550 kcal per day at 12-23 months of age. By letting the baby continue to suckle until he is two years old, the mother will be able to help make sure that her baby is happy and healthy. If you want to do one good thing for the baby this week, encourage the mother to continue breastfeeding after she introduces solids to her baby. References WHO. 2000. Complimentary Feeding: Family Foods for Breastfed babies. WHO. 2006. Infant and young child feeding counseling: an integrated course. 27 Now the baby is 6 months, he can have some soft, mashed foods. Give him mashed fruit, vegetables or thick porridge 2-3 times a day. It is now time to start introducing solids to the baby. Encourage the mother to go slowly. Eating solids is a very new experience for the baby. Suggest that the mother starts with mashed food. Porridge is a good first food. Soft fruits such as banana and mango mashed well are also good options to start with, slowly moving on to lentils, beans and meat. Advise the mother to mash them with some clean water or breastmilk to make them into a paste. This will make it easier for the baby to swallow. Food should be thick enough to stick to a spoon, or feed by hand. The baby will only need a small amount of solid food. Make sure the mother gives some to her 2-3 times a day. A couple of spoonfuls will be enough for now, gradually increasing to around 3 Please suggest food items that are easily available in your area. The energy needs from complementary foods for infants with “average” breast milk intake in developing countries (WHO/UNICEF, 1998) are approximately 200 kcal per day at 6-8 months of age, 300 kcal per day at 9-11 months of age, and 550 kcal per day at 12-23 months of age. coffee cups over the next few months. Encourage the mother to keep offering her breast. Her milk is still an important food for the baby. Once the baby starts eating solids, her stools will change. They will become darker and smellier. The more foods the baby eats, the more different her stools will be. If you want to do one good thing for the baby this week, help the mother to start introducing a couple of spoonfuls of soft, mashed food two to three times a day. References WHO. 2000. Complimentary Feeding: Family Foods for Breastfed babies. 2000 WHO. 2006. Infant and young child feeding counselling : an integrated course. 28 Protect the baby from diarrhoea. Make sure his food is well-cooked and fresh. Give him only clean, safe water. Now that the baby is eating solid food it is important that the food is kept safe and clean. This will help to prevent him and the rest of the family from becoming sick. Here are three things you can do to keep food safe for the baby and the family. One; make sure that all food is washed before it is cooked. Fruit, vegetables and meat need washing in clean water. This will remove germs. Make sure the family washes their hands before preparing food, too. Two; make sure the only fresh food is fed to the family and to the baby. Food that is stale or old will be full of germs. Check that old food is thrown away. Three; tell the family to cook food well. Food that has not been cooked all the way through still contains germs. Meat should be cooked until it is no longer pink in the middle. Fish should be cook until it flakes. If the baby is fed eggs, make sure they are cooked until they are firm in the middle. If you want to do one good thing for the baby this week, share these tips with the family to keep food safe for the baby. References WHO. 2000. Complimentary Feeding: Family Foods for Breastfed babies. WHO. 2006. Infant and young child feeding counseling: an integrated course. Nearly 2 million children die from diarrhoea every year. (WHO. 2010). This is why it is so important to keep food, utensils and hands clean. WHO. 2000. Food borne disease: a focus for health education. UNICEF. 2012. Diarrhoea. http://www.unicef.org/health/index_43834.html. [Accessed on 3 June 2014] WHO. 2011. Zinc supplementation in the management of diarrhoea. http://www.who.int/elena/titles/bbc/zinc_diarrhoea/en/. [Accessed on 3 June 2014] WHO. 2013. Diarrhoeal Disease. http://www.who.int/mediacentre/factsheets/fs330/en/ [Accessed on 3 June 2014] 29 Teething can be painful. Rub a clean finger over his gums to numb the pain. Some cream on his chin will protect it from drool. Teething can be painful and uncomfortable for the baby. Here are some things you can do to help the baby and her mother cope. Some babies get a red rash where they have been dribbling. Try wiping it off with a very soft cloth. You can then put shea butter or coconut oil on her chin. This will help to protect her skin. To ease her pain, try rubbing a clean finger along her gums. This may help to soothe her. A cold spoon would also be good. If the mother is having trouble feeding, encourage her to express her milk instead. This way she will still be able to give her baby the food she needs. You could also feed the baby cold, soft food such as yoghurt or porridge. If the baby is in a lot of pain, make sure the mother takes her to the clinic. Clinic staff may be able to give her pain relief. If you want to do one good thing for the baby this week, follow these tips to ease teething pain. If shea butter or coconut oil are not widely available, please change these recommendations. Teething is something every parent will have to go through. This message gives advice that will be useful to everyone receiving the messages. References Macknin ML, Piedmonte M, Jacobs J, Skibinski C. 2000. Symptoms associated with infant teething: A prospective study. Pediatrics 105:747-52 McIntyre GT and McIntyre GM. 2002. Teething troubles? British Dental Journal192(5):251-5. www.nature.com/bdj NHS. 2010. Teething. NHS Choices, Health A-Z. www.nhs.uk Wake M, Hesketh K, Lucas J. 2000. Teething and tooth eruption in infants: A cohort study. Pediatrics 106:1374-9 30 Make sure the mother doesn't feed tea, coffee, sugary or salty foods to her baby. They have no goodness and won't help the baby grow. Nappy rash is very common in babies. A baby with nappy rash will have a red, inflamed bottom. If you or the baby’s mother spot nappy rash, you need to make sure that his bottom is kept clean. Check that his nappy is changed as soon as he wets it and that his bottom is cleaned and dried afterwards. Usually a nappy rash will go after about three or four days. If it doesn’t clear up, help the mother take her baby to the clinic. A health worker may give the baby a cream to reduce the rash. You can help prevent the baby getting nappy rash. Make sure that If babies do not commonly wear nappies in your country, please adapt this message. Gives practical advice that will empower the guardian. his nappy is changed often and that his bottom is cleaned and dried. Also encourage the mother to let him have some time with no nappy on. This will allow his skin to breathe and recover from any irritation. If you want to do one good thing for the baby this week, make sure his nappy is changed often. References Baer EL, Davies MW, Easterbrook KJ. 2006. Disposable nappies for preventing napkin dermatitis in infants. Cochrane Database of Systematic Reviews (3): CD004262. CKS. 2009. Nappy rash. Clinical Knowledge Summaries, Clinical topic. Dib R, Kazzi AA. 2010. Pediatrics, diaper rash. eMedicine. NHS. 2010. Nappy rash. NHS Choices, Health A-Z. WHO recommendations: Spacing of two years 31 The mother may want to have The family may want the mother to have another baby now. But between the birth of a baby and getting another baby now, but spacing spacing babies by two years is the best way for the mother and pregnant again. babies by 2 years is the best way future babies to stay healthy. MChip recommendations: three years birth to for future babies to stay healthy. You can help the mother by explaining to the family why waiting is birth interval. best. Tell them that waiting until the baby is two years old will give Please choose the recommendation followed by your country. the mother more time to recover from labour and birth. This will If other types of contraception are available help her to grow strong babies in the future. Having another baby locally, please amend. too soon could cause them to be born early and weak. Family planning methods can help the mother to space her pregnancies. Encourage her to go to the clinic to find out about the different options. Explain to her that it will be worth it for healthy babies. If you want to do one good thing for the baby this week, encourage the mother to find out about the various methods of family planning. References UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction. Family planning: the unfinished agenda The Lancet Sexual & reproductive health series. 2006 World Health Organization. 2005. Report of a WHO Technical Consultation on Birth Spacing. Worms are parasites that live in human bowels 32 Tell the mother to clean the With the baby becoming more active every day, it is important you baby's play area with soap make sure that the area he plays in is kept safe and clean. This will help (intestines). Some worms are big enough to see with the naked eye, some worms are very and water, to protect him to keep him healthy - and prevent nasty accidents. small and are harder to see. Some worms can from germs. Always keep an Make sure that the baby plays away from water. Water that has not enter the body through the mouth as worm eggs; others enter through the skin as larvae. It eye on the baby as he plays. been boiled is full of dirt and germs. Playing in it could make the baby sick. His play area should also be far away from latrines and animal stools. These areas are very dirty. The baby may love playing with animals, but wash his hands well with clean water and soap afterwards. This will get rid of any germs. The floor can also be home to many germs. If you can, make it safe for the baby to play on by cleaning the floor well with clean water and soap. Or, you could lay down a clean sheet or blanket for the baby to play on. This will give him somewhere safe to play. If you want to do one good thing for the baby this week, find him somewhere clean to play. is therefore important for children to develop the habit of washing hands properly, keeping nails short and clean and always wearing footwear when playing in the ground (soil). (WHO. Urbani school health kit) References WHO. 2005. The evidence is in: deworming helps meet the Millennium Development Goals. World Health Organization. WHO. Urbani School Health Kit: A Lively and Healthy Me: A Campaign on Preventing and Controlling Worm Infections for Health Promoting Schools. (date unknown) Not all illnesses need to be treated at the 33 An ill baby will need plenty of All babies get ill at some point. When the baby is ill she will need clinic. Good guidelines for treatment in the food. Encourage the mother special care. home can help the family deal with every day to breastfeed often. Her milk Encourage the mother to let her baby sleep when she wants. The baby illnesses. But this message also highlights when will help her baby to fight off will probably have lots of short sleeps. This can be tiring for the it is necessary to take the baby to the clinic. the illness. mother, so encourage her to nap with her baby. The baby will also need plenty of food. Encourage the mother to breastfeed often. Her milk will help her baby to fight off the illness. With an ill baby the mother may not have time to get all her work done. Explain this to the family and share out the work. This will give the mother time to care for her baby. If the baby does not get better, or if she gets a fever, refuses to feed, grunts or cries strangely, help the mother take her baby to the clinic. If you want to do one good thing for the baby this week, think about these tips for helping an ill baby. References WHO. Nutrition Topic: Exclusive Breastfeeding. 2010 WHO.2011. Essential Interventions, Commodities and Guidelines for Reproductive, Maternal, Newborn and Child Health. 34 Encourage the mother to trust her instincts. She will know when something is wrong with her baby. Make With the baby on the move there are likely to be a few more bumps and bruises! But there are things you can do to make the house as safe as possible. Add additional safety issues in your area. 5% of under-five deaths are caused by injuries. WHO 2010. Causes of Child Mortality in 2010 sure she takes her to the clinic. One; encourage the whole family to check the house every day for things the baby could pick up. Look out for small objects that he could swallow, such as coins. Also check for sharp or dangerous objects. Poisons or anything that is not safe to eat or drink, like detergents and kerosene, should be kept well away. Make sure that they are put away after use and are stored in a locked container. Two; check that there is nothing in the house that could fall on the baby. Also look out for objects with cords or ribbons she could become entangled in. Three; make sure that the baby is kept away from fire and cooking areas. Put a barrier up in front of the oven or stove. If the baby gets burnt, pour some cold water on the burn and take him to the clinic immediately. Do not apply anything on the burn without consulting a doctor. Four; make sure the baby is kept away from water. Water containers should also be kept away and covered. This will help prevent accidents. Always keep an eye on the baby. If you’re not around make sure a responsible person is keeping an eye on the baby. If you want to do one good thing for the baby this week, get the whole family to make the house safe References World Health Organization. 2008. Tackling injuries, the leading killers of children. Regional Office of Europe-World Health Organization. WHO/UNICEF, 2008, World report on child injuries. http://whqlibdoc.who.int/publications/2008/9789241563574_eng.pdf?ua=1 35 The baby can now eat soft thick food 3-4 times a day. Try mashing potato with meat, eggs, fish or beans. He still needs breastmilk. Now that the baby has been eating solids for a while, she may enjoy more filling or stronger flavoured foods. Make sure the family buys some meat, fish, eggs, peas and lentils. Remind the mother to cook and mash them well into a soft thick porridge - like thick honey that clings to a spoon when it's turned over. Start encouraging the mother to give her baby 3 to 4 small cups of solids about 3 times a day now. Suggest that she feed her some food at family mealtimes, as well as one or two snacks. Bread or pieces of fruit make good snacks. The baby may also enjoy drinking clean water and coconut water now, as well as breastmilk. These will refresh her. Explain to the mother that Delete instructions to eat meat and fish in vegetarian communications Suggest food available locally that would be suitable for a baby’s first foods. The energy needs from complementary foods for infants with “average” breast milk intake in developing countries (WHO/UNICEF, 1998) are approximately 200 kcal per day at 6-8 months of age, 300 kcal per day at 9-11 months of age, and 550 kcal per day at 12-23 months of age. tea, coffee or sugary drinks are not the best drinks to give. They have no goodness. If you want to do one good thing for the baby this week, encourage the mother to give her baby some tasty new food. References WHO. 2000. Complimentary Feeding: Family Foods for Breastfed babies. WHO. 2000. Food borne disease: a focus for health education. WHO. 2006. Infant and young child feeding counseling: an integrated course. 36 Keep the baby away from anyone with TB. If a family member has chest pain and cough, get them checked for TB. Get the baby checked too TB can be dangerous for babies. You can help the baby to stay safe by looking out for signs of TB. A baby with TB will have a cough and he may not gain weight. He may also get lots of chest infections or have swollen glands and a fever. He may have difficulty breathing. If you or the mother sees any of these signs, take him to the clinic. While you are there, you and the mother may need to get tested for TB, too. TB that is spotted early can be treated. Make sure the mother gives all the medicine. The baby will need it for six to nine months. He should have the medicine even if he gets better. You can help prevent the baby from catching TB. Check that he had the TB vaccine when he was born. If he didn’t, help the mother take her baby to the clinic to get it. Also make sure that anyone in the family with signs of TB gets tested. If a family member has TB, the baby can get medicine from the clinic to prevent catching TB, too. If you want to do one good thing for the baby this week, make sure that the family is screened for TB. An estimated 1.7 million people died from TB in 2009. WHO. 2011 Global TB Control. References WHO (2013) Global Tuberculosis Report. http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf?ua=1 WHO (2014) Guidance for national tuberculosis programmes on the management of tuberculosis in children, Second edition; http://apps.who.int/iris/bitstream/10665/112360/1/9789241548748_eng.pdf?ua=1&ua=1 WHO (2013) Guideline: Nutritional care and support from patients with Tuberculosis; http://apps.who.int/iris/bitstream/10665/94836/1/9789241506410_eng.pdf?ua=1 WHO (2012) Recommendations for investigating contacts of persons with infectious tuberculosis in low- and middle-income countries http://apps.who.int/iris/bitstream/10665/77741/1/9789241504492_eng.pdf?ua=1 WHO (2013) Systematic screening for active tuberculosis: principles and recommendations. http://apps.who.int/iris/bitstream/10665/84971/1/9789241548601_eng.pdf?ua=1 WHO (2009) WHO policy on TB infection control in health-care facilities, congregate settings and households. http://whqlibdoc.who.int/publications/2009/9789241598323_eng.pdf?ua=1 Liefooghe R et al. (1997) From their own perspective. A Kenyan community's perception of tuberculosis Tropical Medicine & International Health, 2(8): 809–821, http://onlinelibrary.wiley.com/doi/10.1046/j.1365-3156.1997.d01-380.x/abstract Complications that arise from animal bites or 37 If the baby gets bitten or A playful baby may get scratches and bites. Seeing the child hurt may scratches are uncommon, but if they do occur scratched by an animal, get worry you and the mother, but many injuries can be treated at home. they can be serious. One possible complication her checked at the clinic. is a bacterial infection that spreads through the Clinic staff can help prevent If the cut or bite is on an exposed part of the baby's body, place a clean bloodstream, known as sepsis (NHS Choices 2010). Rabies is a preventable viral disease of infection. cloth over it and bandage it up. Otherwise leave it open to the air. mammals most often transmitted through the bite of a rabid animal. The rabies virus infects If the wound is bleeding, apply a clean cloth to it and press with your the central nervous system, ultimately causing fingers. Bandage the wound and then make sure the mother takes her disease in the brain and death. Once a person baby to the clinic. begins to exhibit signs of the disease, survival is rare. To date, less than 10 documented cases of human survival from clinical rabies have If the bleeding doesn't stop after a few minutes, tell the mother to go been reported and only two have not had a to the clinic right away. The wound may need stitches. history of pre- or post-exposure prophylaxis (CDC 2011). If rabies is not an issue in your Check with the mother that the baby has had all his vaccinations. A bite area, please remove reference to it. If there are poisonous insects in your area that you or scratch can become infected. would like to mention, please add to this message. If the baby is bitten by an animal, help the mother take her baby straight to the clinic. Animal bites can be dangerous and put the baby at risk of rabies. If you want to do one good thing for the baby this week, ask the mother if her baby has had all his vaccinations. References CKS. 2011. Clinical topic: Bites – human and animal. NHS Clinical Knowledge Summaries. www.cks.nhs.ukNHS. 2010. Bites, human and animal. NHS Choices, Health A-Z. www.nhs.ukwww.cdc.com 38 Make sure the mother can Measles is spread through coughs and sneezes. The baby can catch it if Fit to local vaccination schedule take her baby to the clinic she is near an infected person. But there are things you can do to keep Immunisation prevents three million child deaths each year. this week. It is time for the the baby safe. Expanded Programme for Immunisation (EPI) is baby to have her next set of Make sure the baby gets the measles vaccine. She can get the measles part of WHO strategy to tackle MDG 4 (WHO) vaccines and Vitamin A. vaccine now. Remind the mother to take her baby to the clinic to get it. Fit to local measles immunisation schedule. Check that she has the time and money to go. You can also help to keep the baby safe by looking out for signs of Measles is one of the leading causes of death measles. By spotting them early you can help the baby get the treatment she needs. The signs of measles are similar to a cold. The baby will have a runny nose, a cough and a sore throat. Red, blotchy rashes will appear after a few days on her face and neck. If you see these signs, get the baby to the clinic quickly. Clinic staff will help. If you want to do one good thing for the baby this week, remind the mother to take her baby to get the measles vaccine. among young children even though a safe and cost-effective vaccine is available. An estimated 164 000 people died from measles in 2008 – mostly children under the age of five. Source: WHO Factsheet 2010 References Summary of WHO position papers – recommended routine immunisations for children (Tables 1 & 2) http://www.who.int/immunization/policy/Immunization_routine_table1.pdf http://www.who.int/immunization/policy/Immunization_routine_table2.pdf 39 If the mother is tired, help her with baby care. Tell her to rest when her baby naps. See that she eats well and drinks lots of safe water. You can help the mother to get her baby to sleep well. Try helping the mother to create a bedtime routine. A bedtime routine will help get the baby in the mood for sleep. Suggest playing a quiet game with the baby before bed, or telling her a story. Encourage the mother to do this at the same time every day. You can also start teaching the baby how to fall asleep by herself. This will help her learn how to sleep through the night. Make sure the mother does the usual bedtime routine with the baby and puts her to bed. Then make sure she leaves the baby and waits. You and the mother can keep checking her at intervals. If the baby doesn’t settle, the mother can go to her, but encourage the mother not to make a fuss of her. This will help her to stay feeling sleepy. If you want to do one good thing for the baby this week, talk to the mother about creating a bedtime routine. Bedtime can become stressful for parents. Bed-time routines are an ideal way to make the process easier. References BC UK Davis KF, Parker KP, Montgomery GL. 2004. Sleep in Infants and Young Children: Part One: Normal Sleep. Journal of Pediatric Health Care 18: 130-7 Ficca G, Fagioli I, Salzarulo P. 2000. Sleep organization in the first year of life: developmental trends in the quiet sleep-paradoxical sleep cycle. J Sleep Res9(1):1-4 Hames P. 1998. NCT book of sleep. NCT Publishing, London Mindell JA, Kuhn B, Lewin DS et al. 2006. Behavioral Treatment of Bedtime Problems and Night Wakings in Infants and Young Children. Sleep 29(10): 1263-1276 40 Tell the mother to keep her family safe by disposing of To keep the baby healthy, check that the whole house is clean. This will help keep germs away while he plays. If housing does not usually have proper flooring, please make necessary changes. stools away from the home and washing her hands afterwards. Stools contain germs. Make sure that the family washes the floors. This will remove germs. Check that plenty of soap and water is used. Also encourage the whole family to wash their hands when they come home. Set an example and do it yourself, too. Explain to the family that using a toilet is the cleanest way to dispose of stools. Encourage them to use it if they have one. Make sure that they wash their hands well after using it. If the baby plays outside, you can make it a safe, clean area to play in. Check that he plays away from latrines and animal stools. These areas are full of germs and could make the baby sick. Wash his hands with soap and clean water if he touches any animals. Watery areas are also unclean for the baby. Riverbeds can contain worms. It is best to keep him away from puddles and rivers, too. If you want to do one good thing for the baby this week, follow these tips to give the baby somewhere clean to play. Worms are parasites that live in human bowels (intestines). Some worms are big enough to see with the naked eye, some worms are very small and are harder to see. Some worms can enter the body through the mouth as worm eggs; others enter through the skin as larvae. It is therefore important for children to develop the habit of washing hands properly, keeping nails short and clean and always wearing footwear when playing in the ground (soil). (WHO. Urbani school health kit) References UNICEF. 2011. Water, Sanitation and Hygiene Annual Report 2010. 41 Diarrhoea can dehydrate the baby. Protect him by giving him lots of clean water. Get zinc and ORS from the clinic to prevent dehydration. The baby will need extra care when it is hot. Heat rash and dehydration can become a problem. Follow these tips to keep the baby comfortable. Stay indoors during hot days and check that the baby is dressed in cool cotton clothes. Check her temperature during the day. Take a layer off her if she is too hot. Make sure that she drinks enough, too. Encourage the mother to offer her breast more, or give the baby clean water or coconut water. This will prevent dehydration. If the baby does get a heat rash, you can help soothe it. Wipe the area with a soft wet cloth and let the air dry the skin. Advise the mother to leave the baby’s nappy off for a while. You could also suggest going to a health worker if it does not get better. If you want to do one good thing for the baby this week, discuss with the mother how to keep the baby cool in hot weather. References UNICEF. 2011. Water, Sanitation and Hygiene Annual Report 2010. Annually, safer water could prevent: - 1.4 million child deaths from diarrhoea; - 500 000 deaths from malaria; - 860 000 child deaths from malnutrition WHO.2008 This message gives the mother and guardian useful, practical tips that will empower them. The Lancet. 2004. Executive Summary of Lancet Neonatal Survival Series. World Health Organization. 2010. Countdown to 2015. UNICEF. 2012. Diarrhoea. http://www.unicef.org/health/index_43834.html. [Accessed on 3 June 2014] WHO. 2011. Zinc supplementation in the management of diarrhoea. http://www.who.int/elena/titles/bbc/zinc_diarrhoea/en/. [Accessed on 3 June 2014] WHO. 2013. Diarrhoeal Disease. http://www.who.int/mediacentre/factsheets/fs330/en/ [Accessed on 3 June 2014] 42 Ask the mother to open the Ear infections can be quite common in babies. They can be painful and Ear infections are common. This is why a description of ways to prevent them is windows when cooking, and uncomfortable. extremely useful. the family to smoke outside the house. Smoke can make it hard for the baby to breathe. The baby may have an infection if he starts refusing feeds or pulling at his ear. If the infection is really bad, there may be a bad smell coming from an ear, too. If you think the baby has an ear infection, help the mother to take him to the clinic. Clinic staff will give him treatment and pain relief. If the mother wants to use other treatment, explain why it is best not to. Oil or other herbal remedies could make the infection worse. You can help prevent the baby from getting an ear infection. If the baby has a cold, encourage the mother to breastfeed. Her milk will help to protect him. She could also try feeding him in an upright position. You could also open windows and doors during the day, and ask smokers to go outside. Smoke can make it easier for the baby to get an infection. If you want to do one good thing for the baby this week, make the house as smoke-free as possible. References WHO. 2001. Model chapter for textbooks, Integrated Management of Childhood illnesses. Geneva: WHO. CKS. 2009. Clinical topic: Otitis media – acute. NHS Clinical Knowledge Summaries. www.cks.nhs.uk [Accessed February 2011] NHS. 2010. Otitis media. NHS Choices, Health A-Z. www.nhs.uk [Accessed February 2011] 43 If the baby has fever, bathe her in cool water. She needs plenty of breastmilk. If the fever lasts more than a day, take her to the clinic. A fever is a sure sign of illness. You will be able to tell if the baby has a fever by feeling her tummy, hands and feet. If they are hot, this means the baby is feverish. A baby with a fever may be irritable, unsettled and unwilling to feed. If you spot these signs, help the mother take her baby to the clinic. The baby may need treatment. In the meantime, encourage the mother to breastfeed her baby. Also offer her clean water and coconut water, too. A feverish baby will need plenty to drink. 'Appropriate home care and timely treatment of complications' identified as a key strategy in tackling MDG 4. Source: WHO Factsheet Sponging the baby’s face and body with a clean, wet cloth will help to cool her. Let her rest when she wants. If the fever does not go down, the mother needs to take her baby to the clinic now. Make sure she can go. If you want to do one good thing for the baby this week, look out for signs of fever. References The Lancet. 2004. Executive Summary of Lancet Neonatal Survival Series. World Health Organization. 2010. Countdown to 2015. 44 If the baby's eyes are sticky or pink, he may have an eye infection. Bathe his eyes in cool clean water. Get him checked at the clinic. Lots of babies get problems with their eyes. If you spot a yellow discharge from the eye, or if the eye looks pink and watery, get the mother to take her baby to the clinic. Make sure she can go – if the baby’s eye is infected it will need treatment. Eye infections can spread easily. Explain this to the rest of the family and make sure that no one uses the baby’s cloths or towels. Once the baby’s eye infection is better, make sure the cloths and towels are washed in boiling hot water to clean them. This will help stop germs from spreading. You can help the mother care for her baby’s sore eyes by washing the eyes in clean water daily. Use a separate cloth for each eye. Wash your hands before and after doing this. If you want to do one good thing for the baby this week, keep the baby away from smoke and dust. Children are prone to eye infections. If left untreated, severe cases can permanently damage the eye. CKS 2007 Approximately 75% of the cases of blindness could have been prevented or treated. Preventable causes include corneal scarring from vitamin A deficiency, measles, neonatal conjunctivitis, and harmful traditional eye treatments. USAID 2007. References USAID. 2007. The USAID Child Blindness Program. CKS. 2007. Clinical topic: Conjunctivitis – infective. NHS Clinical Knowledge Summaries. CKS. 2009. Clinical topic: Conjunctivitis – allergic. NHS Clinical Knowledge Summaries NHS. 2010a. Conjunctivitis, allergic. NHS Choices, Health A-Z. NHS 2010b. Conjunctivitis, infective. NHS Choices, Health A-Z. 45 Wash fruit and vegetables to remove dirt and germs. Use boiled water and wash them well before feeding them to the baby. The baby is growing up. But it is still important to keep her clean and healthy. This will help to keep illness away. Washing hands is still the best way of removing germs. Make sure the whole family washes their hands when they come home, after using the toilet, after touching animals or after changing nappies. Encourage them to use plenty of soap and clean water. The baby’s hands will also Handwashing interventions reduced the incidence of diarrhoeal diseases by 32% in low and middle income countries Source: Ejemot et al. 2009 The home-setting is considered the first place in which foodborne diseases develop due to poor personal and/or environmental hygiene need washing. Encourage the family to wash food well, too. Food that has not been washed is covered with dirt and germs. By washing meat, vegetables and fruits before preparing it, lots of the germs will be removed. Food also needs to be cooked fresh for the baby. Old food can contain lots of germs that will make her sick. Check that meat is cooked until it is no longer pink and eggs are cooked until they are firm. If you want to do one good thing for the baby this week, encourage the family to wash their hands often. with an increased risk of infection (Istituto Superiore di Sanità 2003; Comodo et al. 2000; Fara and Proietti 2000; Griffith et al. 1998; Istituto Superiore di Sanità 2006; Kagan et al. 2002; Redmond and Griffith 2003; Scott 2001) References UNICEF. 2011. Water, Sanitation and Hygiene Annual Report 2010. WHO. 2000. Food borne disease: a focus for health education. WHO. 2003. Healthy Villages – A guide for communities and community health Workers. WHO. 2001. Water for Health: Taking Charge. 46 Try giving the baby soft fruit that he can feed himself. Now he is eating solid foods, he may get constipated. Fruit can soften stools. Changes in the baby's stools can be a sign of illness. Encourage the mother to look out for them. Her baby may need treatment. Loose, watery stools are a sign of diarrhoea. The baby will lose lots of fluids. Encourage the mother to keep breastfeeding. You could also offer the baby clean water or coconut water. Suggest that the mother gets treatment for her baby from the clinic, too. The solution will help the baby replace the salts, sugars and fluids that he has lost. If the baby still has diarrhoea after a day, help the mother take her baby to the clinic. The clinic will offer ORS and zinc to treat the baby’s diarrhoea. Constipation is when the baby struggles to pass stools. He may have to strain a lot. His stools will be small and hard. If the baby doesn’t pass any stools for two days, he needs to go to the clinic for treatment. A constipated baby needs lots of fluids, too. Offer clean water. You can also give the baby fruits and vegetables. This will help to get things moving. If you want to do one good thing for the baby this week, encourage the mother to look out for changes in her baby's stools. References UNICEF. 2012. Diarrhoea. http://www.unicef.org/health/index_43834.html. [Accessed on 3 June 2014] Helps the mother understand what changes in her baby's stools are abnormal and when to seek treatment. This empowers her with knowledge and also helps ensure that sick babies get the treatment they need. Nearly two million children die from diarrhoea every year. Source: WHO Factsheet, WHO 2012. Children: Reducing mortality WHO. 2011. Zinc supplementation in the management of diarrhoea. http://www.who.int/elena/titles/bbc/zinc_diarrhoea/en/. [Accessed on 3 June 2014] WHO. 2013. Diarrhoeal Disease. http://www.who.int/mediacentre/factsheets/fs330/en/ [Accessed on 3 June 2014] 47 Keep the house safe for the crawling baby. Keep water buckets, small or sharp objects, detergents, kerosene or medicine away from the baby There are lots of things you can do to help keep an active baby safe. Put a barrier in front of the stairs or fire. To prevent burns, keep lighters and matches far out of the baby’s reach. Also make sure that cigarettes are put out. When cooking is going on, offer to look after the baby. You can also protect the baby against accidental poisoning. Make sure that all detergents, medicines, kerosene, and poisons are in well-sealed containers. Keep them on a high shelf so that the baby cannot reach. If you think that the baby may have swallowed something, take her and her mother straight to the clinic. Take a container of whatever she has swallowed with you if you can. Try to keep the floor clear of small objects that the baby could swallow, too. Cups and plates that are breakable should also be kept safely away. If you want to do one good thing for the baby this week, follow these tips to keep the baby safe from injury. 5% of under-five deaths is caused by injuries. WHO 2010 The most common agents involved in childhood poisonings in low-income and middle-income countries are hydrocarbons used for fuel and lighting, such as paraffin oil (also known in some countries as kerosene). (WHO/UNICEF, 2008, World report on child injuries) References World Health Organization. 2008. Tackling injuries, the leading killers of children. Regional Office of Europe-World Health Organization. WHO/UNICEF, 2008, World report on child injuries. http://whqlibdoc.who.int/publications/2008/9789241563574_eng.pdf?ua=1 48 If a family member has TB, take your baby to the clinic for preventive medicine. This will prevent him from catching TB, too. Chickenpox is a common childhood illness. Make sure you look out for signs of it. Infected babies usually get spots on their face, chest and head. This can spread to other parts of the body. An infected baby may also have a fever. Help the mother get her baby to the clinic as soon as these spots appear. A health worker will confirm whether it is chickenpox. The spots will be very itchy, but try to prevent the baby from Chickenpox is a mild and common childhood illness that most children catch at some point. NHS Choices. 2012. Among children 1-14 years of age, case fatality rate is one per 100,000 cases. MCHIP. Immunisation Essentials. 2003. scratching. You can help soothe the irritation by getting some calming cream from the clinic. A baby with chickenpox will be infectious until the spots dry up. This normally takes about 10 days. Help keep other children safe by advising the mother to keep her baby away from them. If you want to do one good thing for the baby this week, discuss signs of chickenpox with the mother. References CKS. 2008. NHS Clinical Knowledge Summaries. Clinical topic – Chickenpox.www.cks.nhs.uk [Accessed February 2010] HPA. n.d. Health Protection Agency. Chickenpox – varicella zoster: general information. www.hpa.org.uk [Accessed February 2010] HPA. 2006. Health Protection Agency. Guidance on infection control in schools and other childcare settings. www.hpa.org.uk [pdf file, accessed February 2010] NHS. 2010. NHS Choices, Health A-Z. Chickenpox. www.nhs.uk [Accessed February 2010] [Accessed May 2011] NHS. 2009a. Safety for babies. NHS Choices, Birth to five. www.nhs.uk[Accessed May 2011] NHS. 2009b. Leg and foot problems in children . NHS Choices, Birth to five.www.nhs.uk [Accessed March 2011] RoSPA. 2010. Should my child use a baby walker? Royal society for the prevention of accidents. www.rospa.com [Accessed May 2011] Scott O. 2010. Delay in Walking. Patient UK. www.patient.co.uk [Accessed May 2011] Sheridan M. 2008. From birth to five years: children's developmental progress. London: Routledge This message sympathises with a common 49 If the baby has diarrhoea, Looking after a baby can be stressful for the mother. Here are some experience of mothers. This increases trust in give her 1/4 cup of clean things you can do to help. the messages, and also gives the guardian water after every loose stool. The mother will feel much better if she gets plenty of sleep. Give her practical things to do to help. The mother should keep breastfeeding, too. more time to rest by looking after her baby for a while. Encourage her to go to bed as soon as her baby is asleep, too. If the baby takes a long time to settle, make sure the mother sticks to a bedtime routine. The mother will also feel better if she eats well. Make sure she has three meals a day and two snacks. She will need all that food to give her the energy to look after her baby. You could also help the mother by letting her know that you are there to talk to. Talking to someone will help ease any worries she has. If you want to do one good thing for the baby this week, follow these tips to make the mother’s life less stressful. References Nice. 2010. Weight management before, during and after pregnancy. National Institute for Health and Clinical Excellence. Public health guidance 27. World Health Organization/ Food and agriculture organization. 2006. FAO/WHO technical consultation on national food-based dietary guidelines. MIND. 2006. How to look after yourself. National Association for Mental Health.www.mind.org.uk UNICEF. 2012. Diarrhoea. http://www.unicef.org/health/index_43834.html. [Accessed on 3 June 2014] WHO. 2011. Zinc supplementation in the management of diarrhoea. http://www.who.int/elena/titles/bbc/zinc_diarrhoea/en/. [Accessed on 3 June 2014] WHO. 2013. Diarrhoeal Disease. http://www.who.int/mediacentre/factsheets/fs330/en/ [Accessed on 3 June 2014] 50 Make sure the baby gets deworming treatment from the clinic after his 1st birthday. Worms can make the baby very sick. Encourage the mother to talk to clinic staff about what other vaccinations her baby needs in the future. As the baby gets older, he will need the DTP, measles and polio vaccines. These doses will give him greater protection against disease. Remind the mother why vaccinations are important. Now that the baby is very active, he will probably play more in the dirt and mud outside. In some areas, worms can be a problem. They live in the soil and can make the baby sick. To protect him, make sure the mother dresses him in thick socks or shoes, and washes his hands often. Encourage the mother to clean his nails, too. Worms can make the anus (back passage) itchy and if the baby scratches, he will get their eggs under his nails. He could later swallow them. Luckily, when the baby turns one he can get deworming treatment. If you want to do one good thing for the baby this week, talk to the mother about vaccinations and deworming treatment. Change to fit local deworming practices Fit to local vaccination programmes. Worms are parasites that live in human bowels (intestines). Some worms are big enough to see with the naked eye, some worms are very small and are harder to see. Some worms can enter the body through the mouth as worm eggs; others enter through the skin as larvae. It is therefore important for children to develop the habit of washing hands properly, keeping nails short and clean and always wearing footwear when playing in the ground (soil). (WHO. Urbani school health kit) References WHO. 2005. The evidence is in: deworming helps meet the Millennium Development Goals. World Health Organization. WHO. Urbani School Health Kit: A Lively and Healthy Me: A Campaign on Preventing and Controlling Worm Infections for Health Promoting Schools. (date unknown) http://www.who.int/immunisation/documents/positionpapers/en/ Summary of WHO position papers – recommended routine immunisations for children (Tables 1 & 2) http://www.who.int/immunization/policy/Immunization_routine_table1.pdf http://www.who.int/immunization/policy/Immunization_routine_table2.pdf 51 The baby is almost one-yearold! Feel proud of all the help and support you have given the mother this year. Good luck with next year! Here are three things you can keep in mind to keep the mother and her baby happy and healthy in the future. One; remind the family that traditional or herbal remedies can still be harmful for the baby. She may be older and stronger now, but the clinic is still the best place to get her treated. Two; keep encouraging the mother to breastfeed. The baby will gradually eat more and more solid food. She will be able to have chopped or mashed family food that she can pick up with her hands. But her mother’s milk will still have lots of goodness. The mother can breastfeed her baby until she is two years old. Three; explain the importance of birth spacing to the family. Now that the baby is one year old, the family may want the mother to have another baby. But it is best if the mother waits another year before becoming pregnant again. This is the best way for her to have healthy babies and to stay strong for them. Good luck for the future! References WHO. 2000. Complimentary Feeding: Family Foods for Breastfed babies. A A Opaneye. 1998. “Traditional medicine in Nigeria and modern obstetric practice: need for cooperation”, Central African Journal of Medicine, 44(10):258-61. Chuang, Chao-Hua et al. 2006 . “Herbal Medicines Used During the First Trimester and Major Congenital Malformations: An Analysis of Data from a Pregnancy Cohort Study”, Drug Safety, Volume 29, Number 6, pp. 537-548(12). Thein , Koh et al. 1995. “Risk factors for birth defects in Singapore: a case control study”. Annals, Academy of Medicine, Singapore. 24(3):421-7. Opio, N., & English, M. (2011). What clinical signs best identify severe illness in young infants aged 0–59 days in developing countries? A systematic review . Arch Dis Child ,1052–1059. Chowdhury, H., Thompson, S., Ali, M., Alem, N., Yunus, M., & Streatfield, P. (2011). Care seeking for fatal illness episodes in Neonates: a population-based study in rural Bangladesh. BMC Pediatrics . UNDP/UNFPA/WHO/World Bank Special Programme of Research Development and Research Training in Human Reproduction. Family planning: the unfinished agenda The Lancet Sexual & reproductive health series. 2006 World Health Organization. 2005. Report of a WHO Technical Consultation on Birth Spacing.