UNIVERSITY HEALTH SERVICE PATIENT PARTICIPATION
advertisement

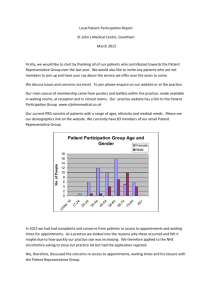
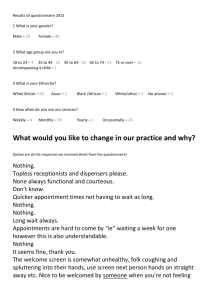
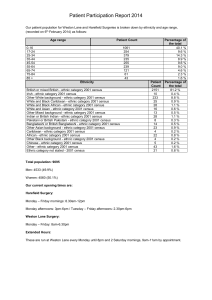
UNIVERSITY HEALTH SERVICE PATIENT PARTICIPATION GROUP ANNUAL REPORT 2011 – 2012 INTRODUCTION The University Health Service is an NHS (Personal Medical Services contract) General Practice with approximately 24,000 patients. Most of the patients are undergraduate, post graduate or partners or dependents of students of the University of Sheffield. The Practice operates an open list and is open 5 days a week – Monday to Thursday 8.45 – 6.00 pm and Friday 8.45 – 5.00pm during term time and Monday – Friday 8.45 – 5.00 during vacations. The University Health Centre is located in modern, purpose built, award winning premises. Access to the building is excellent being served by the tram, numerous bus routes, a disabled ramp and lift to the upper floor. Access to appointments is offered via: Voice Connect - 24 hour access to the automated appointment book. No Pin is required but the callers telephone number must be the one we hold at the University Health Service. On Line – 24 hour access via the University Health Service web site. You will need a PIN to access this service. Telephoning the practice during open hours. Appointments are generally for ten minutes but during afternoons, some fifteen minute appointments are available. The practice operates a scheduled release of appointments at pre defined intervals to ensure that some appointments are available to be booked in advance as well as on the same day. Choose and Book is used for all possible referrals to secondary care, for the convenience of patients. When the surgery is closed, patients can contact a doctor from the Doctors’ Collaborative by telephoning the usual practice number 0114 22 22 100. At the University Health Centre, medical services are provided by 10 (8.3wte) General Practitioners. 10 nurses (5.2wte), including 2 nurse practitioners and, a health care assistant also provide surgeries every day. They deal with a wide range of problems, including routine smears, foreign travel advice, vaccinations, general health issues, asthma, management of wounds and injuries, ear syringing, wart treatment, emergency contraception, follow-up for other contraceptive services, male/female sexual health, chlamydia screening and phlebotomy. Specialist nurses provide surgeries for eating disorders and minor ailments. Continuity of care is encouraged by asking patients to remain with the same doctor for any one condition and this is included in our practice leaflet and on our website. The practice also offers the services of a community physiotherapist and midwife. A health visitor is available. Mental health services are provided at the practice by a CBT therapist, two specialist psychotherapists and three psychological wellbeing practitioners (PWP’s). There is also a supportive reception and administration team. The Patient Survey & Patient Participation Group In April 2011 we created a Survey Monkey questionnaire using questions from the 2010 GPAQ Survey (General Practice Assessment Questionnaire) to seek the views of patients. This was emailed each week to all those patients seen in the current week who had given us an email address, until 50 had been returned for each GP. The mailings commenced in May 2011 and the last survey was collected on Friday 11th November 2011. In total 582 questionnaires were completed and returned for the 10 GP’s at the Practice. It was felt that the process provided the practice, the PPG and the PRG with valid outcomes and was comparable with the survey conducted in the previous year. In previous years when the Practice undertook the GPAQ survey, the process took approximately 6 weeks and involved a member of staff approaching patients directly in the waiting room to complete the questionnaire following their consultation. This was carried out after the Christmas recess. The Practice has a very high level of patient turnover owing to the large number of students registered with the Practice and, as a consequence, the patient representative group will change from year to year. The Union is planning to appoint a Project Support Officer to enable some continuity in the future. The Patient Representative Group: We first attempted to set up a patient representative group in October 2005 with minimal success. In August 2011, following the Government initiative to develop new methods of gaining patients’ opinions and placing the onus on practices themselves to approach patients, we contacted the Student Union Welfare Representative to discuss the feasibility of inviting student representatives to participate in a virtual, patient representative group. This was a positive meeting and was followed up in December with a further meeting when the Welfare Representative advised us that he had been successful in interesting eight patients to participate. An invitation was also posted in the waiting room and leaflets made available to patients interested in participating to ensure a representative group. An international student was also recruited directly by the practice. The Group Profile: The group currently consists of 11 members: 4 male and 7 female. Nine members are in the 17 -24 age group and two in the 25 – 34 age group. The main spoken language is English. Sharing the Survey with the PRG: We posted the results of the survey on the University Health Service website in February 2012 and set up a MUSE Space (my university of Sheffield) where the patient representative group could feed back their comments to share with other members of the group and the Practice. We emailed the PRG in mid February, following the exam period, with the patient survey comments, inviting them to comment via the MUSE group. One member of the group responded. We therefore decided to hold a meeting to discuss the survey. This was held on March 12th and one member attended who offered very constructive comments. A further meeting was held on March 19th with another member of the group attending. The principal issues raised were: waiting times for appointments a feeling of being rushed – 10 minutes not long enough the location of the patient call display – not easily visible from all positions in the waiting room We agreed an action plan. The practice was also commended for: The text reminder service for appointments The multilingual, self check in screen The offer of an appointment in Intro Week, to those patients with pre existing conditions, was thought to be particularly supportive. Action Plan: At the meetings we agreed the following actions: To explore ways to increase awareness of the staggered release of appointments for on line and 24 hour telephone bookings. To work with the Student Union to run a stall in Intro Week/or mid October for all students in addition to the International Student event. To make use of Umail, the Union, weekly newsletter. To make available to the Student Advice Centre and the Student Services Information Desk, copies of the leaflet “Which Service Is Best For You”. Also to place this on the UHS web site. To email a copy of the blank survey to all members of the group for discussion and revision for 2012/13. To discuss with the group whether Facebook would be a more effective social media for communication with the group. It was felt that a more effective position for the patient call display was not possible given the design of the waiting room. The display does beep to indicate to those waiting that another patient is being called. Publication: The action plan is published on the UHS website and the report sent to the PCT March 2012