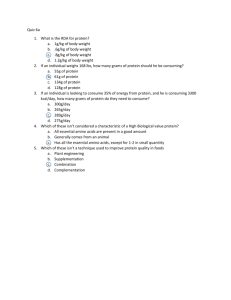
Amino acids can be used for which of the following purposes
advertisement
1) Amino acids can be used for which of the following purposes? Choose all that apply. A. Synthesis of protein B. Conversion into fats C. Oxidation into energy D. Synthesis of heme E. Synthesis of nucleic acids ###all of the above are correct 2) T/F – Dietary protein must always be hydrolyzed to its constituent amino acids before absorption. ##FALSE – This is true for most cases, but newborns are an exception. 3) Which of the following is not true regarding gastric digestion of proteins? A. Pepsin must first be converted to its active form (pepsinogen) in order to begin protein digestion B. Low pH allows for the removal of the inhibitory prosegment from pepsin C. Pepsinogen is synthesized in the gastric mucosa D. Stomach acid contains relatively high levels of HCl, providing an optimal acidic pH for gastric digestive enzymes E. Digestion of proteins in the stomach results in a mixture of large polypeptides ### A – Pepsinogen is the zymogen that must be first converted into pepsin Pepsinogen is the zymogen that is produced in the gastric mucosa, and eventually converted into the active pepsin. The inhibitory prosegment is present on pepsinogen AND pepsin, and is removed from pepsin due to the acidic (<pH 2) HCl environment. The purpose of pepsin is to break dietary amino acids into chains that are shorter than the dietary polypeptides, but still fairly long. 4) Which of the following is not true regarding chyme? Select all that apply. A. B. C. D. E. It contains the acidic remnants of partially digested protein from the stomach It results in a cloudy appearance of the lymph after its uptake into lacteals It triggers the release of the hormone secretin It is responsible for the release of the hormone cholecystokinin It is the sound a bell makes when rung vigorously. ###B is a characteristic of chyle, and is related to fat absorption. E is talking about something totally different. 5) At what pH would you expect the enzyme chymotrypsin to have optimal activity? A. B. C. D. E. 1.5 2 7 8 11 ###D - Chymotrypsin is a serine protease that is secreted into the small intestine after chyme enters the duodenum. Recall that the secretion from the pancreas is alkaline, which both prevents the digestion of the tissues of the small intestine, as well as providing the optimal pH for these proteases. Pepsin, on the other hand, is found in the stomach and has an optimal pH of 1.5. 6) Which of the following accurately describes the function of the protein trypsin? A. B. C. D. E. Denatures proteins in the diet Breaks denatured proteins down to relatively large polypeptides Breaks oligopeptides into a mixture of dipeptides and tripeptides Hydrolyzes dipeptides and tripeptides into individual amino acids Directly facilitates the absorption of amino acids in the gut ###C - The acidic environment of the stomach denatures proteins. Pepsin degrades these proteins into large polypeptides, which are then further degraded to a mixture of di- and tri-peptides by our serine proteases. Aminopeptidases and dipeptidases finish the degradation down to individual amino acids. 7) Which of the following digestive enzymes are excreted into the small intestine in active form (NOT as a zymogen)? A. B. C. D. E. Cholecystokinin Chymotrypsin Enteropeptidase Trypsin Elastase ###C - The hormones secretin and cholecystokinin (CCK) are released into the bloodstream by the movement of chyme into the SI. One of the functions of CCK is to trigger the release of enteropeptidase. Enteropeptidase goes on to activate trypsin, and trypsin goes on to activate pretty much everything else;l 8) Which of the following is not a contributor to pancreatitis? A. Cholelithiasis of the common bile duct B. Premature release of enteropeptidase C. Trypsin mutations that prevent binding of trypsin inhibitor D. Premature activation of trypsin, leading to intracellular degradation E. Pancreatic autocatalysis of trypsinogen ###B – Remember that enteropeptidase is secreted into the duodenum by the lumenal cells of the SI. By secreting this into the system far away from where trypsin is produced, you avoid premature activation of your proteases. 9) Which of the following regarding amino acid levels is false? A. B. C. D. E. Serum amino acid levels are generally lower than intracellular levels. Relative proportions of amino acids in the serum is highly fluctuant depending on diet. Glutamine and alanine are highly abundant in both plasma and inside cells. Absorption of amino acids largely occurs in the gut and kidneys Every cell takes up amino acids ###B – Serum amino acid levels have relatively little to do with how much is in the tissues or diet. Instead, the amino acid content of the blood has much more to do with metabolic processes and events. 10) Which of the following regarding amino acid transport is false? A. Amino acids are usually taken up via active transport B. Cystinuria patients are at relatively higher risk of developing renal calculi C. A cystinuria patient will excrete large amounts of the basic species arginine, citrulline, and lysine D. Pellagra would most likely occur in a patient due to a cystinuria-induced cysteine-deficiency. E. A patient with Hartnup’s disease will excrete large amounts of tryptophan. ###D – Pellagra is associated with Hartnup’s. Deficiencies in both niacin and tryptophan lead to the 3 D’s of pellagra: dermatitis, diarrhea, and dementia. 11) Which of the following sources contributes the majority of the total amino acid pool of the blood? A. Dietary protein B. Muscle protein C. Digestive enzymes D. Synthesis from glycolytic intermediates and ammonia ###B - I stole this question from a practice exam on TUSK. It’s an important point that dietary protein is not where most of our serum amino acids come from. Most of our a.a. pool comes from the constant protein turnover in our cells as they adapt to the body’s needs from moment to moment…muscle being the biggest contributor to this because of its high mass. 12) Part of your treatment for a patient with hyperammonemia is carefully monitored feeding with a solution of essential amino acids. Which of the following amino acids would be included in this formula? A. B. C. D. E. Cysteine Proline Tyrosine Alanine Threonine ###E - It’s a good idea to know your essential amino acids. I’m not super happy with the PVT TIM HALL mnemonic, and the answer choices I’ve chosen to use above should make it clear why. Still, I don’t have any better tricks for this, so be sure to take a few moments to commit them to memory. 13) The Lysosomal “autophagy” system is a relatively unimportant mechanism for the degradation of proteins. Instead, this is largely accomplished by the ubiquitin proteasome pathway (UPP)…which of the following is least likely to alter the activity of the UPP on a given protein? A. Phosphorylation of the E3 ligase B. Cleavage by an aminopeptidase C. Point mutations in a proline-rich sequence D. Cleavage by a caboxypeptidase E. HPV E6 interaction with E3 ligase ###D – I modified this question from one of the Quizzes on the TUSK sidebar. Remember that UPP recognizes proteins for destruction via: N-End, phosphorylation of substrate or E3, Destruction Boxes, PEST sequences, oxidative damage, or binding to specific facilitators/chaperones. Carboxypeptidases cleave at the C-end, as opposed to aminopeptidases that cleave at the N-end. Since the C-end isn’t really a big discerning criteria for what gets degraded or not, this is our answer. Remember that HPV E6 disrupts the UPP E3 ligase for p53, leading to abnormally increased destruction of this crucial tumor suppressor. HPV infection has been linked to increased risk for numerous health issues, incl genital, head, and neck cancers in both males and females. Tell your patients to get vaccinated! 14) Abnormalities in the UPP can lead to numerous diseases, including Alzheimer’s, Huntington’s, and Parkinson’s. Which of the following might you expect to see in a patient suffering from Parkinson’s? Select all that apply. A. Nuclear inclusions d/t CAG repeats B. Accumulation of abnormal proteins in the polyglutamine tract C. Lewy bodies from over-aggregated ubiquitin D. Accumulation of beta-amyloid plaques in the brain E. Mutations in the ubiquitin-conjugating ligase Parkin ###C/E – You don’t need to know any of these other answer choices, though some of them should look familiar. Note that etiologies of Parkinson’s disease include malfunctions in the E3 ligase and/or deubiquitinase. CHAPTER 29 - NITROGEN 15) A healthy patient who has doubled his dietary protein intake can expect increases in the excretion of urinary ___________? A. Creatinine B. Uric acid C. Urea D. Ammonia E. Glutamine ###C – Levels of urea will typically reflect protein intake. Don’t confuse this with serum amino acid levels, which typically DO NOT reflect protein intake. 16) In which of the following would you expect someone to be in positive nitrogen balance? A. A patient after severe burns B. A patient with kwashiorkor C. Starvation D. Childhood E. Infection ###D – Positive nitrogen balance occurs when body protein is accumulating, as in childhood, pregnancy, or after exercise. You would expect negative nitrogen balance to occur during starvation, infection, or trauma. 17) Free ammonium above 100 μM is toxic, so the body converts excess nitrogen into the excretory product urea. Which of the following is not true regarding this process? A. Amino groups are transferred to a common carrier via transaminases. B. All aminotransferases require the coenzyme pyridoxal phosphate to function C. The ketoacids pyruvate, oxaloacetate, and/or α-ketoglutarate are required for all transamination reactions D. Lysine and threonine cannot exchange amino groups via transamination. E. Essential amino acids can be synthesized through amination of the corresponding ketoacids. ###C – Transaminases (aka aminotransferases) require pyridoxal phosphate (PLP, aka Vitamin B6). While the three ketoacids listed in C are the major metabolites of carbohydrate metabolism, any suitable ketoacid can be used as an acceptor. Remember that the essential amino acids are essential because we lack the ability to synthesize the ketoacid precursors – making the actual amino acid is usually no problem after that. 18) Glutamate dehydrogenase is a critical enzyme that catalyzes the release of an amino group from glutamate. Which of the follow is not true of this enzyme? A. Glutamate DH is primarily found in the mitochondria B. Glutamate DH catalyzes an irreversible reaction C. Glutamate DH uses NADH as a coenzyme D. Glutamate DH uses NADPH as a coenzyme E. Deamination of glutamate is inhibited by GTP and ATP ###B – This reaction is reversible, though usually strongly favors the deamination of glutamate since [glutamate] is high and [urea] is low in most cases. Remember that this deamination often occurs because your body is breaking down proteins to use their C-skeletons for energy – high GTP and ATP means this is not necessary, so they inhibit the deamination of glutamate. 19) Glutamine synthetase catalyzes a useful reaction, forming glutamine from glutamate, using up an ATP in the process. Which of the following is not true of glutamine and glutamine synthetase? A. Glutamine synthetase is useful in detoxification by providing a non-toxic transport form for transporting ammonia B. Glutamine is the most abundant plasma amino acid C. The nitrogen in glutamine can be transferred to aspartate via asparagine synthetase to form asparagine D. Glutamine is important in the production of purines and pyrimidines E. Glutamine synthetase catalyzes a reversible reaction ###E – The glutamine synthetase reaction is irreversible. 20) Where in the body does the complete urea cycle occur? A. The bladder B. The liver C. The blood D. The mitochondria E. The joints ### B 21) Which of the following correctly describes the relationship between CPS I and/or CPS II? A. CPS I is a cytoplasmic enzyme involved in pyrimidine synthesis B. CPS II is a mitochondria enzyme involved in the urea cycle C. CPSI is a cytoplasmic enzyme involved in purine synthesis D. CPS I is a mitochondrial enzyme involved in purine synthesis E. CPS II is a cytoplasmic enzyme involved in pyrimidine synthesis ###E 22) Which of the following is false regarding the regulation of the urea cycle? A. Under normal physiological conditions, the enzymes are rarely saturated and the substrates of the urea cycle are the rate-limiting factors B. The key regulatory step of the urea cycle is catalyzed by CPS I, the first irreversible reaction of the urea cycle C. Regulation of the key regulatory step is controlled primarily by the activity of the enzyme, rather than the amount of enzyme D. N-acetylglutamate is synthesized from glutamate and acetyl-CoA only in the mitochondria E. Arginine, as an indicator of plentiful urea cycle activity, inhibits the upregulatory activity of NAG ###E – The downstream product arginine stimulates the formation of NAG in an example of positive feedback. This is characteristic of disposal pathways, whereas pathways that produce functional products are typically subject to negative feedback instead. CHAP 30 – AMINO ACID BREAKDOWN 23) Which of the following is false? A. Muscles primarily oxidize the amino acids Ile, Leu, and Val for ATP production B. The Cahill Cycle enables the body to release excess nitrogen during muscle catabolism C. The liver is the primary location for extraction of amino acids from the blood. D. The intestines make particular use of the amino acid glutamine for regeneration E. Glutaminase in the kidneys causes NH3 diffusion into the urine, which is particularly helpful against hyperammonemia and alkalosis #E – This process plays a large role in combating acidosis 24) Which of the following amino acids cannot be used to generate glucose and glycogen? A. Cysteine B. Leucine C. Isoleucine D. Tyrosine E. Phenylalanine ### B – remember that the only non-glycogenic amino acids are leucine and lysine. 25) If a patient is unable to oxidize the carbon skeletons of glycogenic amino acids, where is the problem likely to be? A. The cytosol B. The endoplasmic reticulum C. The mitochondria D. The cell membrane E. The endosomes ### C – Oxidation of these skeletons occurs in the mitochondria. Remember that the goal is to shuffle them into the TCA cycle, which occurs in the mitochondrial matrix. Moreover, the mitochondria is the major site of these types of oxidation reactions – both the TCA cycle and B-oxidation of fats occurs here. 26) Which of the following amino acids cannot enter the TCA cycle at α-ketoglutarate? A. Arginine B. Cysteine C. Proline D. Glutamate E. Glutamine ###B – The entry of the α-KB path amino acids is closely related to the urea cycle. If this problem gives you trouble, take a minute to look back at the urea cycle and how these amino acids fit in. 27) Maple Syrup Urine Disease is likely to be caused by a deficiency in: A. BCAA Dehydrogenase B. Biotin C. Methyl-B12 D. Adenosyl-B12 E. Tetrahydrobiopterin ###A – MSUD deficiency means all of our branched ketoacids can’t be turned into propionyl-CoA and accumulate, leading to cognitive deficits as well as urine that smells of maple syrup. Don’t confuse this maple syrup urine with the malodorous urine found in phenylketonuria (PKU), which is described as “musty.” 28) Which of the following causes of methylmalonyl acidemia is commonly linked to pernicious anemia? A. Deficiencies in methylmalonyl-CoA mutase B. Poor dietary intake of Vitamin B12 C. Lack of intrinsic factor D. Inability to convert B12 to the adenosyl form E. Deficiencies in biotin ###C – Intrinsic factor is what enables the absorption of Vitamin B12. While lack of B12 in the diet would also lead to similar symptoms, this is much less common. Pernicious anemia is typically found in patients over the age of 60. 29) Defects in the conversion from Phe to Tyr in the fumarate path lead to phenylketonuria (PKU). Which of the following is false regarding this reaction? A. This process requires the conversion of tetrahydrobiopterin to dihydrobiopterin B. PKU can be treated by a combination of a Phe restricted diet and Tyr supplementation C. Lack of tyrosine in PKU is responsible for symptoms of hypopigmentation D. THB is regenerated form DHB through the activity of NADPH E. PKU can be due to defects in the enzymes phenylalanine hydroxylase or DHB reductase ###D – NADH is responsible for this, not NADPH. NADPH is typically used to move along anabolic reactions – here, we are trying to break down amino acids, and NADH is the appropriate coenzyme. 30) Another defect in the fumarate path results in a disease known as alkaptonuria. Which of the following is false regarding this disease? A. Treatment typically involves a Phe-restricted diet and Tyr supplementation B. It is characterized by an accumulation of homogentisic acid C. Typical sequelae of alkaptonuria include osteoarthritis and joint damage D. It is caused by a defect in the final step of the breakdown from Phe to fumarate E. It is characterized by dark urine ###A – Phe does need to be restricted, but since this defect affects the final step of the process, Tyr supplementation will also lead to problems. 31) Tyrosine is used to generate several important products. Which of the following is false regarding Tyrosine as a precursor? A. Deficiencies in tyrosinase leads to lack of pigment in the hair, skin, and eyes. B. Production of thyroxine involves the addition of four iodide atoms to two tyrosine molecules by tyrosine peroxidase C. Grave’s Disease occurs due to an auto-antibody causing overstimulation of thyroglobulin D. Symptoms of albinism will typically be found in patients with PKU E. Synthesis of the catecholamine dopamine in the brain requires VitaminB6 and VitaminB12 ###E – This process requires Vitamin B6 (PLP) and tetrahydrobiopterin (THB, aka BH4). We used THB before in the conversion of Phe to Tyr. If you are having trouble remembering where each cofactor is used, try taking some time to write out a table for them. 32) Folate is used in numerous processes in the body. Which of the following folate NOT directly involved in? A. Synthesis of glycine B. Regeneration of methionine C. Synthesis of guanidinoacetic acid D. Synthesis of purines E. Synthesis of pyrimidines ###C – Guanidinoacetic acid is an intermediate in the production of creatine. All of the other reactions utilize folate as a cofactor. 33) Which of the following is false regarding the metabolism of creatine? A. Arginine and glycine are joined together and methylated to form creatine B. Phosphocreatine provides a way for muscles to store the high-energy phosphate bonds of ATP for later use C. Creatinine is formed spontaneously from phosphocreatine D. Urine creatine is typically reflective of muscle mass, since the muscles generate a baseline level of creatine E. Creatine appears to be useful as a supplement for resistance training ###D – The species found in the urine should be creatinine, not creatine. Be sure not to confuse these two! 34) Which of the following is false regarding cysteine metabolism? A. Vitamin B6 is a necessary cofactor in the production of cystathione B. The hydrolysis of cystathione is an important step in the conversion of methionine to succinyl-CoA C. Supplementation of cysteine in patients with methionine deficiencies will likely lead to acute exacerbation of symptoms D. Cysteine is converted into taurine, commonly found in the muscles E. Cystathione is formed from the joining of serine to homocysteine ###C – Remember that there is only one way to make cysteine, and that’s through methionine/homocysteine/cystathione. This makes cysteine supplementation a very important part of treatment of methionine deficiencies 35) Homocystinuria is a disease that occurs when elevated serum homocysteine and urinary homocystine present with arterial disease, among other symptoms. Which of the following would not be therapeutically appropriate? A. Cysteine supplementation B. Vitamin B6 supplementation C. Choline/betaine supplementation D. Folate-restricted diet E. Methionine-restricted diet ###D – If defects in cystathione synthetase are leading to buildup of homocysteine, we need to supplement the downstream product cysteine. Vitamin B6 will help a partially functional synthetase convert excess Hcy into cystathione, and choline/betaine and folate are active in two different pathways converting excess Hcy to methionine. Met-restricted diets will help prevent the addition of excess methionine into the already blocked-up Hcy cycle. Restricting folate from the diet would not be appropriate. LEC 32 – PURINE SYNTHESIS 36) In what tissues would de novo purine synthesis be most prevalent? A. The eyes B. The intestines C. The brain D. The liver E. The kidneys ###D – Purine synthesis is especially prevalent in the liver and placenta 37) Which of the following is the committed step of purine synthesis? A. The conversion of glucose-6-phosphate to 6-phosphoglucono-δ-lactone B. The conversion of G6P to ribose-5P C. The conversion of R5P to PRPP D. The conversion of PRPP to 5-phosphoribosyl-1-amine E. The conversion of 5-phosphoribosyl-1-amine to IMP ###D – The committed step here is the first irreversible reaction in the process, which is true of many pathways. The conversion of G6P to R5P to PRPP is common to multiple pathways, and all reversible. The formation of 5-phosphoribosylamine is not only irreversible, but its product is used exclusively in the production of purines. 38) IMP is the first true purine in our de novo purine synthesis. Which of the following is NOT used in the production of IMP from 5-phosphoribosylamine? A. PLP B. Glycine C. ATP D. Folate E. Glutamine ###A – The production of IMP requires Gly, Gln, Asp, CO2, ATP, and folate. I don’t know how important it is to memorize all these elements, but do remember that folate contributes TWO carbons to the final purine ring (this requires two folate molecules, each donating one carbon). 39) IMP is the branching point in the synthesis of either adenosine nucleotides or guanosine nucleotides. Which of the following is not true of this synthesis? A. Formation of xanthylate is upregulated by the activity of ATP B. The kinases used to phosphorylate diphosphate nucleotides to triphosphates are basespecific, but not sugar-specific. C. Elevated GMP levels downregulate the formation of guanosine nucleotides. D. The activation of the antiretroviral AZT requires the activity of thymidine-specific kinases E. 6-mercaptopurine is a hypoxanthine analog effective in preventing the de novo synthesis of purines in leukemia ###B – This is true of the kinases that turn NMPNDP, but the NDP NTP enzyme can work with any base. 40) No need to use energy to make purines de novo if we can just recycle old ones for no energy cost. Which of the following is untrue of the purine salvage pathway? A. The purine salvage pathway operates by combining PRPP with already-formed purine rings B. The enzyme APRT is used in the salvage pathway to produce IMP C. The salvage pathway is particularly important in the activity of purine-analog medications D. The phosphoribosyltransferase enzymes active in the salvage pathway are more effective at low concentrations of PRPP than the de novo amidotransferases E. The end products of the salvage pathway are important in downregulating the de novo pathway. ###B – HGPRT forms GMP and IMP, APRT makes AMP. Another important note to make about choice (a) is that this tactic of adding PRPP to a finished nitrogenous base ring is also found in pyrimidine de novo synthesis. De novo purine synthesis works by taking a PRPP and building the purine on top of it. 41) The catabolism of purines eventually ends with the production of uric acid. Which of the following is NOT a step in the conversion of AMP to uric acid? A. Removing phosphates from AMP to form the nucleoside adenosine B. Removal of the hypoxanthine base from inosine to form ribose-1P C. The formation of xanthine by xanthine oxidase D. The formation of uric acid by xanthine oxidase E. The conversion of adenine to hypoxanthine ###E - AMP is dephosphorylated to form the nucleoside adenosine. The nucleoside adenosine is converted to the nucleoside inosine. They hypoxanthine base of inosine is removed, resulting in R-1P and the hypoxanthine base. The base adenine is never found on its own in this pathway. 42) Disruption of which of the following steps results in SCID? A. AMPadenosine B. AdenosineInosine C. Inosine hypoxanthine D. Inosine R-1P E. Hypoxanthine Xanthine ###B – Deficiencies in adenosine deaminase leads to a lack of B and T lymphocytes, etiology unknown. 43) Gout is a painful disease that occurs as urate crystals are deposited in the joints. Which of the following is false regarding the etiology and treatment of gout? A. Partial defects in HGPRT leads to increased PRPP and decreased inhibition of the de novo synthetic pathway. B. Defects in the regulation of PRPP synthetase leads to increased PRPP C. Gout can be treated by upregulating xanthine oxidase, thus alleviating the accumulation of purines by generating more excretable uric acid D. Total defects in HGPRT result in decreased amounts of purine nucleotides, thus leading to gout E. Allopurinol is commonly used for the treatment of gout ###C – Allopurinol inhibits xanthine oxidase, lowering the amount of uric acid that can crystallize into urate. The intermediates xanthine and hypoxanthine are actually more soluble than uric acid, and are easily excreted. Answer (d) leads to Lesch-Nyhan, which is characterized by symptoms of self-mutilation, mental illness, and gout. 44) Which of the following accurately explains the effectiveness and safety of sulfonamide drugs as antimicrobials? A. Sulfa drugs are particularly effective in impairing the formation of bacterial cell walls B. The 70S ribosomal subunit targeted by these drugs is found only in bacteria. C. These drugs block the activity of bacterial topoisomerase, but have low affinity to eukaryotic topoisomerase D. Administration of these drugs leads to poor purine and pyrimidine synthesis in bacteria, but not humans E. Sulfa drugs act as detergents, increasing bacterial membrane permeability. ###D – Bacteria synthesize folate endogenously, while humans obtain it through diet. Thus, the pathway for folate biosynthesis is a vital process for bacteria, but totally unnecessary in humans. This is an important characteristic for antibiotics – all of the above mechanisms are found in different classes of antimicrobial. Remember that folate is a required step in both purine and pyrimidine synthesis. With sulfa drugs, bacteria are deprived of their folate while the patient’s cells continue to absorb it from dietary sources. Allergies to sulfa drugs are common however, so be sure to check what medications your patients are allergic to! LEC 33 – PYRIMIDINE SYNTHESIS 45) The synthesis of pyrimidines differs from the synthesis of purines in several notable ways. Which of the following is false regarding the synthesis of pyrimidines? A. Unlike purine nucleotides, cytosine nucleotides are generated as triphosphates in the de novo pathway B. Orotate is attached directly to PRPP to form our first nucleotide in the de novo pathway C. Folate is a vital cofactor in the production of cytosine and uracil nucleotides D. The enzyme OPRT is used in both the de novo and salvage pathways E. Carbamoyl phosphate used in pyrimidine synthesis can originate from either the cytosol or the mitochondria ###C – Folate is important in the formation of thymidine nucleotides. Thymidine nucleotides are really only formed in the deoxy-form, when you need it for DNA synthesis. The production of uracil and cytosine nucleotides are unaffected. For (e), the carbamoyl phosphate in the mitochondria is supposed to be used in the urea cycle…but it can occasionally leak out into the cytosol and get tied up in pyrimidine synthesis. 46) Which of the following is the primary regulated step of de novo pyrimidine synthesis? A. Formation of carbamoyl phosphate by CPS II B. Formation of N-carbamoyl aspartate by aspartate transcarbamoylase C. Formation of dihydroorotate by dihydroorotase D. Formation of orotate by dihydroorotate dehydrogenase E. Formation of OMP by OPRT ###A – Carbamoyl phosphate is also produced by CPS I in the mitochondria for urea production. Note the importance of regulation at this step in the urea cycle. 47) Pyrimidine salvage is somewhat more complicated that purine salvage…which of the following is not true regarding salvage? A. OPRT is active in salvage by directly attaching pyrimidine rings to PRPP B. Salvage may be disrupted by interfering with phosphorylase-catalyzed joining of R-1P to a pyrimidine base C. Salvage may be disrupted by interfering with the kinase-catalyzed conversion of pyrimidine nucleoside to nucleotide D. Orotic aciduria can be caused by either a deficiency in OPRT or OMP decarboxylase E. UTP is an effective inhibitor of OMP decarboxylase, inhibiting de novo synthesis but leaving salvage fully operational ###E – UTP inhibits CPS II, which will impact both salvage and de novo pathways. UMP inhibits OMP decarboxylase, but since this enzyme is on the same polypeptide as OPRT, OMP decarboxylase inhibition means to OPRT inhibition as well. 48) Pyrimidine catabolism differs from purine catabolism in several notable ways. Which of the following is false regarding pyrimidine synthesis? A. Cytidine and uridine nucleosides must be converted to the base uracil to undergo catabolism B. The catabolism of bases uracil and thymine are catalyzed by the same enzymes C. Unlike in the catabolism of purine rings, pyrimidine rings are opened during catabolism D. The catabolic end product of uracil is used to monitor cell turnover following radiation therapy E. Pyrimidine catabolism yields soluble products, rather than the relatively insoluble products of purine catabolism ###D – β-aminoisobutyrate is the end product of thymine catabolism, and is indeed used to monitor radiation therapy. 49) All four ribonucleotides can be reduced to form their deoxy-counterparts. Which of the following is not true of this reaction? A. Hydroxyurea inhibits the enzyme ribonucleotide reductase, and is used as an anticancer drug B. The electrons for this reaction are donated by the sulfhydryl groups of a protein called thioredoxin C. The conversion from ribose to deoxyribose requires the nucleotides to be diphosphates D. The electron donor of this reduction reaction is regenerated by a reductase E. NADH is a required cofactor for the regeneration of the electron donor ###E – NADPH is used here. 50) Deoxy-thymidine nucleotides are generated from uracil species using folate and thymidylate synthetase. Which of the following is the substrate in this reaction? A. UMP B. UTP C. dUMP D. dUTP E. Uracil ###C 51) Methotrexate and 5-fluorodeoxyuridine are used as anticancer drugs. Which of the following regarding their anticancer activity is false? A. Both drugs interfere with the production of dTMP. B. Methotrexate interferes with the regeneration of THF C. fdUMP interferes with the synthesis of thymine nucleotides by acting as a competitive inhibitor for thymidylate synthetase D. Methotrexate is also used in the treatment of psoriasis and other proliferative disorders E. Methotrexate binds its target with such high affinity that this binding is effectively irreversible. ###C – fdUMP binds its target covalently 52) 53) 54) 55) 56) 57) 58) 59)