Handbook - University of Alabama at Birmingham
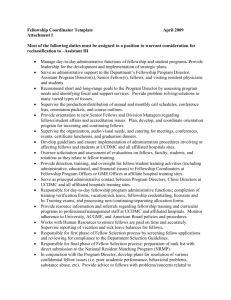
advertisement

Female Pelvic Medicine and Reconstructive Surgery Fellowship Handbook The Fellowship Handbook has been developed as an explanatory tool for the fellows and fellowship applicants. It describes all requirements of this fellowship, many of which are set by the ACGME, UAB GME or the American Boards of Obstetrics and Gynecology and Urology. Each fellow should review this in its entirety at the beginning the fellowship and applicable parts of it throughout the duration of the fellowship. Table of Contents I. II. III. IV. V. VI. VII. VIII. IX. X. XI. XII. XIII. XIV. XV. XVI. XVII. XVIII. XIX. XX. XXI. Pages General Description of Fellowship General Goals, Objectives and Strengths Organization Description of Fellowship Fellowship Staff Fellow Rotations Weekly Schedules Levels of Supervision for Fellows in FPMRS Escalation of Care Bedside Procedures Transitions of Care Competency Based Learning Requirements Section1: Competency Objectives Section2: Learning Objectives (ABOG) Section 3: Milestones Research Requirements Academic and Service Portfolio Healthstream Requirements Policies and Procedures for Duty Hours and Work Environment Policy for Moonlighting Vacation, Sick and Maternity Case List Fellow Competency Evaluations and Assessments for Feedback and Advancement (general description) Responsibilities of the Fellowship Faculty Responsibilities of the Fellow in Female Pelvic Medicine and Reconstructive Surgery 1 2 3 4 7 8 9 12 15 16 17 19 44 47 48 49 53 55 58 59 61 61 I. General Description of Fellowship The Female Pelvic Medicine and Reconstructive Surgery (FPMRS) Fellowship at the University of Alabama at Birmingham is accredited by the ACGME and is compliant with ACGME Program Requirements. It is a three year fellowship for gynecologists and two year fellowship for urologists (unless the urologist desires to do a three year fellowship). To qualify for this fellowship, the applicant should have completed or plan to complete a residency program in Obstetrics and Gynecology or Urology in the US or Canada which is in good standing with the American Board of these specialties. Each fellowship includes the equivalent of 12 months of research, which may be basic science or clinically oriented, interspersed with 24 or 12 months of clinical rotations primarily in Urogynecology, and Urology, as well as, one to two months of Geriatrics. A Colorectal Surgery rotation is available as an elective. The Fellowship faculty includes five Urogynecologists, two Urologists, two Geriatric Specialists, two Colorectal Surgeons, and a Radiologist. Fellows are trained in the evaluation and treatment of women with all pelvic floor disorders. Both surgical and non-surgical approaches to treatment are emphasized. Fellows are also prepared for academic careers via full participation in research projects, grant development, presentations at national meetings, and journal publications. A Thesis Project is required. Fellows are required to complete courses or equivalent training in quantitative techniques of biostatistics and other areas related to research. Completion of master's level graduate degrees concurrent with Fellowship Training is offered. 2 II. General Goals, Objectives and Strengths A. Educational objectives: 1) To broaden the Medical knowledge in Female Pelvic Medicine in a multidisciplinary fashion by educating fellows in the basic science, anatomy, physiology and benign pathology of the pelvic floor including the lower urinary tract, pelvic support structures, and the distal GI tract. 2) To provide advanced training of fellows in the clinical care (both surgical and non-surgical) of patients with disorders of the pelvic floor. This will involve problem-based learning and improvement based on investigative evidence. 3) To instruct and mentor fellows in research techniques: the planning and performing of meaningful research in this subspecialty field. 4) The above objectives will be met through improvement in interpersonal communication skills by which collaborations will be established. To accomplish this, professionalism, systems based team work, and adherence to ethical principles will be necessary. B. Goals: 1) The primary goal of the fellowship at the University of Alabama at Birmingham (UAB) is to train OB/GYN and Urology physicians to have a broad knowledge base and broad expertise in female pelvic medicine and reconstructive pelvic surgery. This should also increase research efforts in this area which has been relatively neglected. The combination of increased knowledge, improved clinical care, and sound research should thus improve the healthcare of an increasing population of women with these conditions. 2) A secondary goal of the program is to improve the education of residents, students, nurses and other healthcare providers in obstetrics and gynecology, urology, and geriatric medicine at our institution. C. Perceived strengths: 1) An unselfish collaboration of multiple specialties including gynecology, urology, geriatric medicine, behavioral psychology and radiology (as evidenced by the existing Genitourinary Disorders Center established in 1997 and Genitorectal Disorders Center established in 2002 through which multidisciplinary clinical care and research are performed). 2) Large and diverse clinical case volume. 3) Excellent research opportunities. 4) Excellent facilities for patient care, teaching and research all located within a single, large academic medical center. The majority of the fellow’s time is spent at UAB Hospital and clinics which includes The University Hospital, The Women and Infants Center, UAB Highlands, and The Kirklin Clinic and their research facilities. All are a part of a large referral institution where both clinical and academic functions are performed. 5) Diverse faculty with expertise in teaching basic science, diagnostic techniques, conservative treatments, surgery and in mentoring research. 6) We have shown that the organization and collaboration between various faculty and fellows has worked well as evident by the productivity of our present fellows and graduating fellows and by their meeting the requirements of the Boards. 3 III. Organization Description of Fellowship General Organization: Fellows are involved in both In-patient and out-patient teaching during each of their rotations. At this time, all of the teaching is performed at University Hospital, the Women’s and Infants Hospital (WIC), UAB Highlands and The Kirklin Clinic (TKC) all of which are part of the University of Alabama at Birmingham Hospitals and Clinics (UAHC). In-patient teaching is organized within each clinical service (Urogynecology, Urology, and Geriatrics) and Colorectal Surgery if desired. Teaching includes: (1) Rounds attended by the fellows, faculty members, residents, and students, (2) Didactic presentations or interactive conferences held in addition to patient rounds, and (3) Interactive sessions prior to, during, and/or after surgical procedures. Each surgical procedure is attended by a faculty member and the fellow progressively assumes more and more responsibility in the performance of surgical procedures. Outpatient teaching is conducted at the WIC and Kirklin Clinic. While rotating on the individual services, fellows will attend clinic with FPMRS faculty members in urogynecology, urology, and colorectal surgery and geriatrics one to four half days weekly and become proficient in evaluation, treatment choices, patient consultation, and the performance of various outpatient evaluations and treatments (outpatient or inpatient as is appropriate). These include urodynamics (simple, complex and video), cystoscopy, Botox and neuromodulation therapy, urethral bulking injections, pessary choice and utilization, excision of small lesions, various nerve blocks, and behavior and biofeedback therapies. In addition, the importance of accurate record documentation, billing and correspondence with referring physicians, family members, etc. is emphasized and critiqued. The fellow’s direct responsibilities in the clinic progressively increase during the first year during which he/she works in the attending physicians’ clinics (see Section XIX). Beginning in the second year of fellowship, the urogynecology fellow will see new and referral patients with incontinence, prolapse, and/or anorectal disorders, as well as some general gynecology or urology patients, in his/her own Friday PM clinic which will alternate with the other senior (2nd or 3rd year) urogynecology fellow every 6 months. The fellow will perform appropriate evaluations including urodynamics, cystoscopy, anorectal evaluation or other appropriate procedures; employ outpatient treatment measures; schedule surgery and counsel patients and family members concerning the procedures. Fellows will follow their own “continuity” patients throughout their care process including preoperative and postoperative assessments during each of these time periods. These clinics are held at the WIC three Fridays each month and at Kirklin Clinic one Friday where urodynamics and other outpatient procedures are performed. A faculty member is assigned to each of these clinics and all patient care will be overseen. (Direct Supervision immediately available). Urology Fellow Continuity clinics will be held in the urology space at Kirklin Clinic and will begin very early in the fellowship under the direction of Drs. Wilson and Lloyd. These will be held weekly. Supervision in ambulatory unit and operating room (also see Section V): Fellows are supervised by faculty members at all times. Faculty members are in attendance in the operating room during the critical portion of all procedures and, throughout the procedures during the initial phase of the fellow’s training. The fellow’s responsibilities increase based on individual assessments of expertise and with experience; he/she may assist residents, with the faculty member serving as a second assistant. Direct supervision or direct supervision immediate availability will be available during all regular work days and direct supervision available on weekends, nights, and holidays. In the outpatient unit, the fellow also sees faculty patients with different faculty members, learning evaluation techniques, outpatient treatment procedures and observing various methods of history taking, counseling, etc. Fellows will immediately communicate any complication or unusual circumstance arising in patient care, in surgery, clinic, or other patient care areas to the supervising physician. This would naturally include admissions to ICU or end of life decisions. 4 Specific Learning Objectives are expected to be met throughout the fellowship as outlined in section IX. These have been developed by the Boards and this Faculty. The fellows are instructed to prepare informal didactic lectures or group discussions on these topics which are presented during their rotations. Fellow clinical performance and knowledge is evaluated by faculty at the end of each 1, 2 or 3 month rotation and by patients, staff, students and residents throughout the fellowship. Conferences: Conferences include General Conferences with attendance required by all fellows and Rotation Conferences with attendance required when the fellow is on the specific rotation. General Conferences: Fellows Conference (1st Wednesday of each month at 5:00 PM) 9 of the 12 conferences would be Milestone Conferences in which case directed discussions related to the following Milestone learning topics selected by our subspecialty’s education committee will be directed by Dr. Ellington, Dr. Wilson, Dr. Varner or other Faculty members. Fellows will have a schedule of these conferences at the beginning of each academic year, one month before the process starts (this year in early September), in order to know which Milestone topics to study. The general topics are: General Pelvic Floor Evaluation and anatomy and physiology of the female pelvic organs UI and Overactive Bladder physiology, pathophysiology and treatment Anal Incontinence & Defecatory problems: physiology, dysfunction and management POP: demographics evaluation and management Urogental Fistula & Urethral Diverticulae: pathophysiology and Treatment Painful Bladder Syndrome: definitions, possible pathophysiology and Treatment UTIs: pathophysiology and management Neurourology (will be divided into 2 conferences) Other interactive conferences on these topics may be scheduled at other times by various faculty members. During the Milestone Conferences, fellows will be asked direct questions or may be asked to discuss various aspects of the Milestone. Junior level fellows will be given more basic questions but if doing exceptionally well; will have their chance to show a higher level of knowledge. Fellows of different levels of training will be expected to exhibit different levels of knowledge and patient care. Examples of where fellows should be at each level are demonstrated in the FPMRS Milestone list which is in the Website. Competencies of Medical Knowledge, Patient Care and Communication Skills of each fellow will be assessed by each faculty member present. These assessments will be compiled as part of the overall milestone assessment on MedHub and immediate feedback regarding performance will be given to the individual fellows by faculty. Other Wednesday Conferences: In addition to the 9 milestone conferences, two other Wednesday Conferences will be scheduled including one or two on research design and statistical considerations and/or special “state of the art” lectures by our faculty or visiting faculty. One conference at the end of the academic year will be reserved for Fellows Thesis presentations. Rotation Conferences: Urogynecology Rotations: Monday AM Surgical Conference, (6:30 AM) The fellows, residents and students on Urogynecology, meet with Dr. Varner to discuss selected surgical procedures including discussions of indications, alternatives, and choice, as well as, technique, complications, and avoidance thereof. Reading on the procedures prior to each session is encouraged. Tuesday Resident-Student Conference (7:00 AM): On the every Tuesday except the last the fellows will alternate with each other and division faculty in leading a 3045min lecture or interactive discussion on a wide array of FPMRS specific topics, as well as general gynecologic subjects. These lectures are attended by both the rotating Urogyn and GYN residents and medical student teams. 5 The intent of the lecture series is to provide teaching/learning experiences for the fellows while covering CORE Curriculum Objectives as outlined by CREOG for the residents. Presentations and Interactive Conferences presented by fellows will be evaluated by faculty and residents in the audience. The last Tuesday of each month and will be attended by fellows, faculty and interested others in 10th Fl WIC Conf. Rm. One faculty member (perhaps a Gen. Gyn or one of us) would concurrently give the Resident and Student conference that same week on 5th Floor. The other Tuesday AM conferences would continue as presently designed. Six of these Tuesday Fellowship conferences would cover selected “Landmark” papers from the PFDN and UITN or other selected papers that will make a major impact to our specialty. There would be two (occasionally one) papers discussed at each of these conferences with a fellow presenter and open discussion. 3 or 4 of these conferences would be interactive case study conferences related to urodynamic or genitorectal evaluations, neuromodulation or other selected cases. 2 or 3 conferences (Mini Protocol Conferences) would be designed to introduce research ideas to the diverse group (this was requested by the members of the Program Evaluation Committee). Mini research protocols would be developed by individual fellows or faculty members (or more than one person) and submitted to the group at least two weeks prior to these conferences. Each fellow or faculty member would rank the submitted mini protocols and the one , two, or more proposals ranked highest would be discussed and, if it was felt by the group to merit further consideration, an “ interested” working group could be designated who would develop a subsequent plan for potential implementation. This could allow for one or more collaborative fellowship projects each year in addition to what is done now and should be educational to all involved. Some of these projects would be small “problem based learning and improvement projects”, but some more substantial projects could receive funding. A selected statistician, Allie Howell or Vel Willis and Dr Richter would be expected to participate in these conferences to help guide the process when a project is decided to be worthwhile and feasible. Friday 12:30 PM: Ob/GYN Department Morbidity and Mortality Conference and Grand Rounds conferences are each held twice monthly. They are, for the most part interactive and include Urogynecology topics ¼ of the time. Fellows’ attendance is mandatory unless the fellow is unable to leave an ongoing surgical case. Fellows are also expected to participate in Friday PM pig lab surgical sessions, with residents and perform and teach general techniques and will develop simulation of urogyn procedures when time and animal availability permits. Urology Conferences: Tuesday: 6:00 AM – Urology AM Rounds as applicable 7:00 AM – Urology/Urogynecology Weekly Lecture (M&M conference once a month, journal club once a month, and didactic presentations by urology residents and faculty members twice a month). Geriatric Conferences: The Geriatric Clinical Conference on Tuesdays at noon Center for Aging Scientific Seminar Series Fridays at noon, variable topics related to geriatrics are presented. Continence Journal Club meets at 9:30 a.m. on Tuesdays. The Journal Club is a teleconference with all members of the Southeast Center of Excellence in Geriatric Medicine which focuses on published articles on incontinence. 6 IV. Fellowship Staff Fellows: The number of fellows may vary between three and four at any one time. Core Faculty Members*: The faculty members who have “contact” with one or more fellows at least eight hours weekly. At this time, core faculty will include the Urogynecology Faculty and Urology Faculty. Other Faculty Members: Geriatric Continence Faculty**, Colorectal Faculty***, Radiology Faculty****, and Non-physician Faculty such as two nurse practitioners functioning in these same subspecialties. Presently, colorectal rotations will be elective; however, they may become regular rotations in the near future. Faculty Email Address and Contact numbers Dr. Holly E. Richter* hrichter@uabmc.edu Dr. Alicia Ballard* aballard@uabmc.edu Dr. Robert E. Varner Jr.* evarner@uabmc.edu Dr. Robert Holley* rholley@uabmc.edu Dr. David Ellington* dellington@uabmc.edu Dr. L K Lloyd* klloyd@uabmc.edu Dr. Tracey S Wilson* traceywilson@uabmc.edu Dr. Patricia S Goode** pgoode@uabmc.edu Dr. Alayne D Markland** amarkland@uabmc.edu Dr. Jamie A Cannon*** jacannon@uabmc.edu Dr. Melanie S Morris*** msmorris@uabmc.edu Dr. Mark E Lockhart**** mlockhart@uabmc.edu Jeannine McCormick, CRNP jmccormick@uabmc.edu (205) 934-3180 (205) 996-2182 (205) 934-3180 (205) 934-3180 (205) 975-3587 (205) 975-0088 (205) 996-8765 (205) 934-3259 (205) 558-7064 (205) 996-4958 (205) 996-4132 (205) 934-7130 (205) 801-8935 Research Nurse Managers: Allie Howell ahowell@uabmc.edu, Velria Willis vwillis@uabmc.edu. Administrative Faculty: Fellowship Director Co-Director Urology Director of Research Dr. Robert E. Varner Jr. Dr. Tracey Wilson Dr. Holly E. Richter Fellowship Competency Committee: Drs. Varner, Wilson, Lloyd, and Richter Fellowship Coordinator: Julie Burge jburge@uabmc.edu (205) 934-2569. 7 V. Fellow Rotations Block Diagram by Month Academic Year 2014- 2015 st One 1 yr. Urogyn Fellow (UGF1), Two 2rd year Urogyn Fellows (UGF2a, UGF2b) UGF1 UGF2a UGF2b Jul UGa UGb R Aug UGb R UGa Sep U UG R Oct UG R U Nov G/R U UG Dec U UG R Jan R R UG Feb G/R U UG Legend: Rotations UG (a) rotation: Drs. Varner/Ellington Service UG (b) rotation: Drs. Richter/Holley/ Ballard UG rotation: Primarily surgery with all UG faculty. Mar UG U R Apr UGb UGa U May U R UG Jun R UG U UG – Urogynecology G/R – Geriatrics/Research R – Research U – Urology Two year Urology fellows will have 9 to 10 Urogyn rotations during their fellowships. Urogynecology fellows will have 9 urology rotations during their fellowship. Two year Urology Fellows: will do 1 month of Geriatrics/Research and one 2 fellow uro/gyn slot which is equivalent to one research slot their first year. If a Urology fellow chooses to do three years, his or her rotations will be the same as Urogynecology fellows. Elective months in Colorectal Surgery, which include ½ time on colorectal clinical service and ½ research time, can be substituted for a research month in years 2 or 3. This will still allow an equivalent of more than 12 months of research. Geriatric/Research rotations are 2/3 research. Urogynecology rotations, UG (a&b), include at least 2 or 3 half day research slots. Fellows are also allowed to use 2 weeks of a research month to go to a site in Africa where they care for patients with significant injuries from child birth, during which time research data is collected. 8 VI. Weekly Schedules Urogynecology Weekly Schedules (UG) ONE FELLOW ON Urogyn ROTATION Monday: 06:15 AM – Floor Rounds as applicable 06:30 AM – Preoperative Conference with Dr. Varner and Rotating Urogyn Residents 7AM – 5PM - OR with Dr. Varner 4PM – 5PM – Post-operative Rounding as applicable Tuesday: 06:15 AM – Floor Rounds as applicable 7 AM – Tuesday AM Lecture Series – Rotating Assignments 8AM – 5PM – Dr. Ballard OR 4PM – 5PM – Post-operative Rounding as applicable 4PM – 5PM – Dr. Richter Pre-operative meeting Wednesday: 06:15 AM – Floor Rounds as applicable 6:30 AM – 5PM Dr. Richter OR 4PM – 5PM – Post-operative Rounding as applicable 5PM-6PM: Urogynecology Conference (1st Wednesday of the Month) Thursday: 06:15 AM – Floor Rounds as applicable 7 AM – 5PM – Robot Surgery with Dr. Ballard the 1st and 3rd of the month and GRDC with Dr. Richter on the 2nd and 4th of the month, (research/office afterwards) 4PM – 5PM – Post-operative Rounding as applicable Friday: 06:15 AM – Floor Rounds as applicable 7 AM – 12:30PM – OR Coverage (Dr. Ellington or Dr. Holley) 12:30PM – 1:30PM – Department Resident Conference/M&M Conference 1:30PM – 5PM - Office/Research Time/OR Coverage as applicable Fellows own clinic when on clinic service ________________________________________________________________________ (UGa) Dr. Ellington and Dr. Varner Service (TWO FELLOWS ON Urogyn ROTATIONS) Monday: 06:15 AM – Floor Rounds as applicable 06:30 AM – Preoperative Conference with Dr. Varner and Rotating Urogyn Residents 7AM – 5PM - OR with Dr. Varner 4PM – 5PM – Post-operative Rounding as applicable Tuesday: 06:15 AM – Floor Rounds as applicable 7 AM – Tuesday AM Lecture Series – Rotating Assignments 8AM – 5PM – Dr. Varner clinic (1st year fellow only) 8AM –4PM – 2nd and 3rd year fellow research/office 4PM – 5PM – Post-operative Rounding as applicable 9 Wednesday: 06:15 AM – Floor Rounds as applicable 7AM - 5PM - Office/Research Time 4PM – 5PM – Post-operative Rounding as applicable 5PM-6PM: Urogynecology Conference (1st Wednesday of the Month) Thursday: 06:15 AM – Floor Rounds as applicable 7 AM – 12AM – Dr. Varner Clinic - Urodynamics, In-Office Procedures, Preop surgical planning 4PM – 5PM – Post-operative Rounding as applicable Friday: 06:15 AM – Floor Rounds as applicable 7 AM – 12:00PM – OR coverage for Dr. Ellington until complete- research/office 12:30PM – 1:30PM – Department Resident Conference/M&M Conference 1:30PM – 5PM - Office/Research Time/Animal Lab/OR Coverage as applicable or Fellows Clinic if on clinic service ______________________________________________________________________________________________ (UGb) – Dr. Holley, Dr. Richter, Dr. Ballard Service -TWO FELLOWS ON Urogyn ROTATIONS Monday: 06:15 AM – Floor Rounds as applicable 7AM – 4Pm - OR with Dr. Holley at Highlands 4PM – 5PM – Post-operative Rounding as applicable Tuesday: 06:15 AM – Floor Rounds as applicable 7 AM – Tuesday AM Lecture Series – Rotating Assignments 8AM – 5PM – OR coverage with Dr. Ballard 4PM – 5PM – Post-operative Rounding as applicable 4PM – 5PM – Dr. Richter Pre-operative meeting Wednesday: 06:15 AM – Floor Rounds as applicable 6:30 AM – 5PM Dr. Richter OR 4PM – 5PM – Post-operative Rounding as applicable 5PM-6PM: Urogynecology Conference (1st Wednesday of the Month) Thursday: 06:15 AM – Floor Rounds as applicable 7 AM – 1PM – Richter GRDC Coverage on 2nd and 4th of the month/OR coverage with Dr. Ballard on 1st and 3rd of the month/Research Time/OR Coverage as applicable 4PM – 5PM – Post-operative Rounding as applicable Friday: 06:15 AM – Floor Rounds as applicable 7 AM – 12:30PM – OR Coverage (Dr. Holley)/GRDC Coverage (Dr. Ballard)/Office/Research Time/ 12:30PM – 1:30PM – Department Resident Conference/M&M Conference 1:30PM – 5PM - Office/Research Time/ Pig Surgical lab/ or OR Coverage as applicable or Fellows clinic if on clinic service _______________________________________________________________________________________________ 10 UROLOGY Rotation Weekly Schedules The Urology rotation consists of both inpatient and outpatient surgical procedures performed at University Hospital and UAB Highlands as well as outpatient clinics at both The Kirklin Clinic and the Spain Rehabilitation Facility. The following schedule provides and outline of the weekly Urology Rotation: Monday: 7AM – 5PM: Dr. Lloyd OR Coverage – University Hospital Tuesday: 6 AM – Urology AM Rounds as applicable 7 AM – Urology/Urogynecology Weekly Lecture (M&M conference once a month, journal club once a month, and didactic presentations by urology residents and faculty members twice a month). 8AM – 5PM: Dr. Wilson TKC Outpatient Clinic Wednesday: 7AM – Dr. Lloyd OR Coverage – UAB Highlands 1PM-5PM: Spain Rehabilitation Urology Clinic 5PM-6PM: Urogynecology Conference (1st Wednesday of the Month) Thursday: 7 AM – UAB Highlands AM Rounds as applicable 7:30 AM - Dr. Wilson OR Coverage – UAB Highlands Friday: 7 AM – UAB Highlands AM Rounds as applicable 8 AM – 5 PM: Dr. Lloyd TKC Outpatient Clinic ____________________________________________________ 11 VII. Supervision for Fellows in FPMRS Fellows, faculty members and patients are aware of the specific attending physician responsible for each patient and will be available through the UAB paging system and, if he/she is not available the fellow will immediately contact the on call faculty member. Residents/fellows and faculty members should inform patients of their respective roles in each patient’s care Faculty attending and call schedules are structured to provide residents/fellows with continuous supervision and consultation. Residents/fellows and other health care personnel are provided beeper numbers and have all phone numbers for communicating with supervising faculty. Levels of Supervision To ensure oversight of resident/fellow supervision and graded authority and responsibility, the program has defined the levels of supervision that is in accordance with the RRC and use the following classification of supervision: a) Direct Supervision (Level1) – the supervising physician is physically present with the resident/fellow while providing patient care b) Indirect Supervision with direct supervision immediately available (Level 2) – the supervising physician is physically within the hospital or juxtaposed site of patient care (North Pavilion, West Pavilion, Spain Wallace, Women and Infants Center, VAMC) and is immediately available to provide Direct Supervision c) Indirect Supervision with direct supervision available (Level 3) – the supervising physician is not physically present within the hospital or other site of patient care but is immediately available by means of telephone and/or electronic modalities, and is available to provide Direct Supervision d) Oversight (Level 4) – The supervising physician is available to provide review of procedures/encounters with feedback provided after care is delivered Fellows are supervised by teaching staff in such a way that the fellows assume progressively increasing responsibility according to their level of education, ability and experience. The program demonstrates that the appropriate level of supervision is in place for all fellows who care for patients. The level of responsibility granted to fellows is determined by the program director and/or supervising teaching faculty and is based on documented evaluations of the fellow's clinical experience, judgment, knowledge, technical skill and the needs of the patient. In general a) Fellows serve in a supervisory role of residents/junior fellows in recognition of their progress toward independence, based on the needs of each patient and the skills of the individual resident/fellow or fellow. b) Fellows must communicate with appropriate supervising faculty members any time there is a patient care emergency, a situation when there is a conflict between any parties delivering patient care or when a subspecialty surgical procedure is to be performed. c) Fellows must be aware of their limitations and may not attempt to provide clinical services or perform procedures for which they are not trained. d) Faculty supervision assignments is of sufficient duration to assess the knowledge and skills of each fellow and delegate to him/her the appropriate level of patient care authority and responsibility. e) The program director is responsible for ensuring that all teaching faculty and residents/fellows are educated to recognize the signs of fatigue and for implementing policies and procedures to prevent and counteract the potential negative effects. Faculty members and residents/fellows are educated to recognize the signs of fatigue and sleep deprivation; alertness management and fatigue mitigation processes; and to adopt fatigue mitigation processes to manage the potential negative effects of fatigue on patient care and learning such as naps or back-up call schedules through direct discussion and formal educational programs (GME lecture on fatigue and management) f) In the event that a fellow may be unable to perform his/her patient care duties, his/her faculty supervisor will be notified in order to assume or arrange for assumption of duties by another fellow and appropriate arrangements will be made to care for the affected fellow. 12 Female Pelvic Medicine and Reconstructive Surgery Urogynecology or Urology Service Level of Supervision Guidelines Faculty Clinics including procedure clinics Surgical Cases Gynecology call and general gynecology surgical cases while on call *Urogynecology Fellow PGY 5* Level 1 PGY 6* PGY6** Level 1 and 2 PGY7* PGY7** Level 1 and 2 Level 1 Level 1 advancing to Level 3 when deemed capable Level 1 Level 3 Level 1 and 2 Level 3 ** Urology Fellow Fellow Level 1: At the beginning of the Fellowship, a fellow(s) should communicate every aspect of patient evaluation or management plan to the attending physician(s) prior to instituting management. Faculty will “directly supervise or perform all surgical procedures with that fellow. The attending faculty will also review the fellows dictated consultation record or notes. For inpatient care the chief resident on Urogynecology or Urology will serve as the manager of that service with the Fellow serving as his/her advisor. The fellow will round on all complicated patients or patients with complications or morbidities with the residents and serve as an advisor and teacher to those residents, but will not serve as their director or “foreman” of the team. The fellow(s) should demonstrate adherence to the six clinical competencies and be an example to the residents. The fellow(s) will function as directed by the attending physicians in the operating room and clinic and will be in direct communication with the attending about all patient care. The fellow will instruct residents in pathophysiology, patient management issues and procedures during rounds and will give formal didactic/interactive conferences to residents and students which are attended by faculty and evaluated by all attendees. Fellow Level 2: In the 2nd year of fellowship for a Urogynecology fellow, he/she will begin his/her own weekly continuity clinics, and “attend” low risk gynecology surgical cases with Direct supervision available. Urogynecology Continuity Clinics will rotate between two or three fellows each 6 to 8 month period, however if a fellow is not on the continuity clinic schedule he/she may make arrangement to see a postop pt. or another private patient with a problem. During the continuity clinic, the fellow will first be under direct faculty supervision (level 1) presenting each case to the faculty member in the same clinic area. When the fellow is felt capable the faculty member will function as a direct supervisor, immediate availability (level2) in the clinic and for inpatients as well. However, the faculty is required to see and be directly responsible for all Medicare patients and will continue to perform daily rounds with the fellow and residents on his/her patients. Urology fellows will function likewise and will largely see general urology patients in their clinic. Urogynecology fellows’ night and weekend call includes general gynecology. Urology fellows’ call includes all urology patients. All fellows will have completed their residency training and will be qualified to manage general gynecological problems (both medical and surgical). However, there will be a faculty member backup for night and weekend call. All calls concerning urogynecology patients will be checked out with the attending either at the time of the call or, if the decision is obvious to the fellow, the next morning or work day. The attending physician is notified of all admissions and is available to come in for any surgical procedures perceived to be difficult or unusual if he/she feels unsure as to whether the fellow might need his/her assistance. Residents are also present during patient care including surgical cases. The fellow’s responsibility progresses as faculty sees fit. All subspecialty surgical procedures on patients of faculty members are performed with Direct Supervision (level 1). Procedures on fellow patients require at least level 2 supervision. 13 Fellow Level 3: At the later stages of fellowship generally early in the last year of fellowship the fellow(s) functions more independently on his/her own patients, but with direct supervision available (level 3), or on occasion (level 4with Oversight)The fellow(s), when the Competency Committee deems he or she capable, however continues to function with faculty supervision on faculty patients, and is still expected to discuss all of his/her surgical cases and out of the ordinary clinical or non-surgical hospitalized patients with the attending. The fellow will occasionally take “attending” responsibility of the inpatient services for periods of time, even on individual faculty member’s patients. At this time, the fellow is allowed to perform or attend residents on surgical procedures performed on his or her continuity patients. Demonstrated competency on focused assessment cases and on the other evaluative assessments is necessary prior to this. Resident and faculty perception that a fellow is able to function well in these situations is important to establish that the fellow can function independently after completion of the fellowship. 14 VIII. Escalation of Care Escalation of Care: Any urgent patient situation should be discussed immediately with the supervising attending. This includes: • In case of patient death • Any time there is unexpected deterioration in patient’s medical condition • Patient is in need of invasive operative procedures • Instances where patient’s code status is in question and faculty intervention is needed • A patient is transferred to or from a more acute care setting (floor to ICU and vice versa) • A patient’s condition changes requiring MET/CHAT team activation • Any other clinical concern whereby the intern or the resident feels uncertain of the appropriate clinical plan Timeliness of Attending Notification: Notification of the attending should not delay the provision of appropriate and urgent care to the patient. The fellow will notify the attending as soon as possible after an incident has occurred. If despite the best efforts, the resident cannot reach the assigned attending, then they should notify the program director, medical director of the service or the chair of the department for guidance. 15 IX. Bedside Procedures Purpose: The purpose of this policy is to provide guidance for fellows on when to notify the attending or higher supervisor trainee when performing bedside invasive procedures. Scope: This policy applies to all bedside procedures performed by fellows on patients seen at University Hospital. Surgical procedures performed by fellows on patients in the operating rooms are not covered by this policy as there are already policies covering these situations. Performance of Procedure: 1. All fellows performing a bedside procedure will discuss the clinical appropriateness of the procedure that might entail risk to the patient with the attending. 2. The attending physician is responsible for determining the appropriate level of supervision required for performing a bedside procedure, the appropriate indication for the procedures, discussion of risk-benefit with residents and patients (as necessary), assessing the risk of the procedure, determining the qualification of the fellow performing the procedure and providing adequate support if felt indicated. 3. It is expected that a fellow shall inform the faculty member when he/she does not feel capable of performing a bedside procedure. 4. The fellow performing a procedure should make sure that there is adequate backup (such as attending, interventional services, surgical services) before performing the procedure. 5. The fellow should attempt the procedure no more than two times before stopping and re-evaluating the clinical situation and asking for a attending, interventional service, or surgical service to take over the performance of the procedure. 6. The procedure should be aborted and alternate plans discussed with the attending when the risk of the procedure including discomfort to the patient outweighs the benefit of repeated attempts beyond three. 7. In case of emergency, greater than three attempts can be made but should be justified with clear documentation of the need to do so in the procedure note. 8. If a life or death patient situation is encountered immediate CPR should be initiated and the MET team should be called STAT. E. TEAMWORK Residents/fellows care for patients in an environment that maximizes effective communication. This include the opportunity to work as a member of effective inter-professional teams that are appropriate to the delivery of care in the specialty 16 X. Transitions of Care Purpose: A responsibility of the Institution that sponsors Graduate Medical Education is to ensure and monitor effective, structured hand-over processes to facilitate both continuity of care and patient safety (Common Program Requirement VI.B.2). The ACGME has charged the institution and the programs with designing clinical assignments to minimize the number of transitions in patient care (CPR VI.B.1), ensuring that residents/fellows are competent in communicating with team members in the hand-over process (CPR VI.B.3), and ensuring the availability of schedules that inform all members of the health care team of attending physicians and residents/fellows currently responsible for each patient’s care (CPR VI.B.4). Scope: This policy applies to all graduate medical education training programs sponsored by the University of Alabama Hospital Definitions: 1. Transitions of care constitute the transfer of information, authority and responsibility during transitions in care across the continuum for the purpose of ensuring the continuity and safety of the patient’s care. 2. Hand-off communication is a real time, active process of passing patient-specific information from one caregiver to another, generally conducted face-to-face, or from one team of caregivers to another for the purpose of ensuring the continuity and safety of the patient’s care. Hand-offs should occur at a fixed time and place each day and use a standard verbal or written template. The circumstances for transitions of care may include scheduled and unscheduled changes of assignments, at the conclusion and the commencement of assigned duty periods or call, when the patient is transferred to another site or another team of providers (e.g. transfer within in-patient settings and out-patient settings), and when it is in the best interest of the patient to transfer the care to another qualified or rested provider (e.g. duty hours or fatigue). Patient Hand off policies which are outlined by the Obstetrics and Gynecology and Urology residency programs will apply to all inpatient Urogyncology and Urology services which fellows rotate. The residents on the Urogynecology Service are responsible for first call on urogynecology or female urology inpatients during the day Monday-Friday. Handoffs occur in a quiet conference room at 5PM each week day evening (unless another time is arranged). These PM and all weekend and holiday handoffs are performed face to face and include the transfer of a printed “Multi-patient Rounds/Sign-Out Report” available for each in hospital patient through Cerner. This template includes all required patient data plus written explanatory notes on current condition, active issues, pending results and any new management plan. This constitutes greater than the “minimal elements for a handoff template”. In addition, the fellow on the urogynecology service or urology service is responsible for corresponding with the “on call” resident about any patient that is considered to have any excess risk for complications. This will be performed after the 5PM handoff between the residents, usually by telephone. Weekday AM handoffs may be made by telephone between the on call gynecology resident and a urogynecology service resident who is familiar with service patients. If there has been an admission, such handoff is face to face and the new EMR is reviewed together. All weekend and holiday transfers are face to face and include the forms on each patient. The house staff members on call are responsible for notifying the Urogynecology or Urology faculty member or fellow on call if any problems should develop involving any patient or the specific service. The disposition of the problem will be decided on, including the need (or no need) for that physician to be present. This correspondence should be made immediately by telephone (direct line or through the paging system). The Impact EMR system, uses the (I-PASS) Impact Physician Handoff on all inpatients which is easily accessible by the residents, fellows and physicians. 17 Since the Urogynecology and Urology inpatient services include individual patients for several different attendings. In addition to the above resident to resident and service fellow to resident handoffs, individual attending physicians are expected to “handoff” patients who have problems or are at risk for problems to the on call faculty or fellow and to discuss with the appropriate on call resident. This will be done by telephone or in person, therefore insuring that direct contact is made and discussion of the patients name, age, condition, care plan, pertinent evaluations which have been performed and concerns that the attending MD has. The attending physicians also have EMR access at home. This policy facilitates appropriate care by the on call attending and resident team should a problem develop in such patients. The individual faculty members or fellows on service will also be responsible for communicating with the on call division member (faculty or fellow) regarding special needs patients (inpatient and outpatient). General Policies: 1. Hand-off communication entails direct communication. 2. Off-going provider will have at hand any required supporting documentation or tools used to convey information and immediate access to the patient’s record. 3. All communication and transfers of information will be provided in a manner consistent with protecting patient confidentiality and privacy. 4. Providers will afford each other the opportunity to ask or answer questions and read or repeat back information as needed. 5. The patient will be informed of any transfer of care or responsibility, when possible. 6. The effectiveness of the program’s hand-off process will be monitored through direct observation and multiperspective surveys of resident/fellow performance. The program will review hand-off effectiveness at least annually during the annual program evaluation meeting. Minimal Elements of a Template: Each residency training program that provides in-patient care is responsible for creating a patient checklist template. At a minimum, key elements of this template should include, but are not limited to: 1. Patient information (name, age, room number, medical id number, important elements of medical history, allergies, resuscitation status, family contacts) 2. Current condition and care plan (pertinent diagnoses, diet, activity, planned operations, significant events during previous shift, current medications) 3. Active issues (pending laboratory tests, x-rays, discharge or communication with consultant, changes in medication, overnight care issues, “to-do’ list) 4. Contingency plans (if/then statements) 5. Synthesis of information (“read-back” by receiver to verify) 6. Opportunity to ask questions and review historical information 7. Name and contact number of responsible resident/fellow and attending physician 8. Name and contact number of resident/fellow/attending physician for back up 18 XI. Competency Based Learning Requirements Section 1: Lists specific competency objectives that will be ongoing throughout the fellowship and reviewed with the fellow each six month period. The fellow and Fellowship Director will set specific competency goals at each semiannual evaluation based on the feedback from the 360 competency evaluations and rotation evaluations. Section 2: Review and study of all specialty specific topics should be begun during the first year with reading all available current literature in textbooks and review papers as, well as, learning in conferences, web based learning programs, journal clubs, surgical labs, and while participating in patient care clinics and surgery. Learning of these topics will continue with thorough reviews of Level I and II literature and appropriate other papers throughout the duration of the fellowship. This section designates which topics should be completed during each 6 month period. At the end of each rotation in Urogynecology (UG), Urology (U), and Geriatrics Research (GR), faculty members will submit an evaluation of how well the fellow has accomplished the specific objectives designated for that rotation. These evaluations and portfolios will be reviewed with the fellowship director at each semiannual evaluation to ensure fellow’s adherence to these assignments. The Focused Assessments of each designated surgical and clinical procedures, the primary research Thesis Project and the Comprehensive Oral Examination are also included. Each of these activities or learning objectives will include the related competency. Other research projects will be interspersed with no specific time table required however weekly oversight by Dr. Richter will insure that appropriate progress is made. Section 3: Milestones. See FPMRS Milestone document on website. These (23) milestones have been set by the ACGME and Boards as the primary requirements by which fellows are determined to be capable of practicing solo in this subspecialty (Level 4) and, in some cases, determined to have achieved “exemplary expertise” (Level 5). All of the evaluations of fellows, which include assessment of all competences, will be objectively tabulated by MedHub and reviewed by the Competency Committee in the spring of each fellowship year to determine his/her, progress in achieving these Milestones. These should be reviewed by the fellow multiple times during his/her fellowship training so that he/she can direct his/herself toward maximal achievement. There will be Milestone Conferences (interactive between faculty and fellows) on all Medical Knowledge and Patient care related milestones repeated each year of the fellowship. 19 Female Pelvic Medicine Milestone Topics Patient Care PC-1 General Pelvic Floor Evaluation PC-2 PC-3 PC-4 PC-5 PC-6 PC-7 Urinary Incontinence and Overactive Bladder Treatment Anal Incontinence and Defecatory Dysfunction Treatment Pelvic Organ Prolapse Treatment Urogenital Fistulas and Urethral Diverticula Treatment Painful Bladder Syndrome Treatment Urinary Tract Infection (UTI) Medical Knowledge MK-1 Pelvic Floor Anatomy and Physiology MK-2 Urinary Incontinence and Overactive Bladder Treatment MK-3 Anal Incontinence and Defecatory Dysfunction Treatment MK-4 Pelvic Organ Prolapse Treatment MK-5 Urogenital Fistulas and Urethral Diverticula Treatment MK-6 Painful Bladder Syndrome Treatment MK-A7 Urinary Tract Infection MK-A8 Neuro-Urology Active Systems-based Practice SBP-1 Computer Systems SBP-2 Health Care Economics SBP-3 Works and coordinates patient care effectively in various health care delivery settings and systems Practice-based Learning and Improvement PBLI-1 Scholarly PBLI-2 Implements Quality Improvement Project Professionalism PROF-1 Professional Ethics and Accountability Interpersonal Communication Skills (ICS) ICS-1 Health Care Teamwork ICS-2 Effective Communication 20 Section I Competency Based Requirements Abbr: PC: Patient Care, MK: Medical Knowledge, PBL: Practice-based Learning, ICS: Interpersonal & Communication Skills, P: Professionalism, SBP: Systems-Based Practice Gyn Uro PC MK PBL ICS P SBP Level Level Fellow must be able to provide care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Fellows are expected to: Patient Care Demonstrate caring and respectful behaviors when interacting with patients and their families. 1,2,3 1,2 x Gather essential information about patients by performing a complete and accurate medical history and physical examination. 1,2,3 1,2 x x Make informed decisions about diagnostic and therapeutic interventions based on patient information and preferences, up-to-date scientific evidence, and clinical judgment. 1,2,3 1,2 x x Develop, negotiate, and implement effective patient management plans. 1,2,3 1,2 x Counsel and educate patients and their families. 1,2,3 1,2 x Use information technology to support patient care decisions and patient education. 1,2,3 1,2 x Competently perform all medical and invasive procedures considered essential for the practice of Female Pelvic Medicine and Reconstructive Surgery 1,2,3 1,2 x x Recognize problems encountered in patient care delivery and develop means of investigating and correcting these problems. 1,2,3 1,2 X X Work with health care professionals, including those from other disciplines, to provide patientfocused care. 1,2,3 1,2 x Use competency assessments for goal setting each semiannual period. 1,2,3 1,2 x 21 x x x x x x x x x x x x X x x x X X X x x x x x x GYN Level Medical Knowledge Uro Level PC MK PBL ICS P SBP Fellow must demonstrate knowledge about established and evolving biomedical, clinical, and cognate (e.g., epidemiological and social-behavioral) sciences and apply this knowledge to patient care. Fellows are expected to: Demonstrate an investigatory and analytic thinking approach to clinical situations. 1,2,3 1,2 Demonstrate a sound understanding of the basic science background of Female Pelvic Medicine Reconstructive Surgery and apply this knowledge to clinical problem solving, clinical decision making, and critical thinking. 1,2,3 1,2 Obtain a thorough understanding of all of the learning objectives listed in section II adhering to the time table provided. 1,2,3 1,2 x x x x x x x x x x x x GYN Uro PC MK PBL ICS P SBP Level Level Fellows must be able to demonstrate interpersonal and communication skills that assist in effective information exchange and be able to team with patients, patients’ families, and professional associates. Fellows are expected to: Interpersonal and Communication Skills Sustain therapeutic and ethically sound relationships with patients, patients’ families, and colleagues. 1,2,3 1,2 Provide effective and professional consultation to other physicians and health care professionals. 1,2,3 1,2 Elicit and provide information using effective listening, non-verbal, explanatory, questioning, and writing skills. 1,2,3 1,2 Demonstrate effective communication with patients in language that is appropriate to their age and educational, cultural, and socioeconomic background. 1,2,3 1,2 Maintain comprehensive, timely, and legible medical records. 1,2,3 1,2 Demonstrate effective communication with others as a member or leader of a health care team or other professional group. 1,2,3 1,2 Complete CERT Creating Effective Resident Teachers Program and give effective educational presentation to residents and medical students at UAB, presentations of research at national subspecialty meetings. 1,2,3 1,2 Use competency evaluations and presentation evaluations for goal setting each semiannual period. 22 x x x x x x x x x x x x x x x x x x x x x x x x GYN Uro PC MK PBL ICS P SBP Level Level Fellow must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse population. Fellows are expected to: Professionalism Demonstrate respect, compassion, integrity, and responsiveness to the needs of patients and society that supersedes self-interest. 1,2,3 1,2 x x Demonstrate accountability to patients, society, and the profession. 1,2,3 1,2 x x Demonstrate uncompromised honesty. 1,2,3 1,2 x x Develop and maintain habits of punctuality and efficiency. 1,2,3 1,2 x Maintain a good work ethic (i.e., positive attitude, high level of initiative). 1,2,3 1,2 x Demonstrate a commitment to excellence and ongoing professional development. 1,2,3 1,2 Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care. 1,2,3 1,2 Describe basic ethical concepts such as: autonomy, beneficence, justice, and nonmalfeasance. 1,2,3 1,2 Describe the process of informed healthcare decision making, including the elements that must exist and the specific components of an informed-consent discussion. 1,2,3 1,2 x Discuss important issues regarding stress management, substance abuse, and sleep deprivation. 1,2,3 1,2 x 1,2,3 1,2 x 1,2,3 1,2 x x x 1,2,3 1,2 x x x x 1,2,3 1,2 x x x x 1,2,3 1,2 x x x Describe current standards for the protection of health-related patient information. 1,2,3 1,2 x x x List potential sources of loss of privacy in the health care system. (P, SBP) 1,2,3 1,2 x x List preventive stress-reduction activities and describe their value. Identify the warning signs of excessive stress or substance abuse within one’s self and in others. Intervene promptly when evidence of excessive stress or substance abuse is exhibited by oneself, family members, or professional colleagues. Demonstrate an understanding of the signs of sleep deprivation and intervene promptly when they are exhibited by oneself or professional colleagues. Maintain confidentiality of patient information. 23 x x x x x x x x x x x x Professionalism GYN Level Uro Level Demonstrate sensitivity and responsiveness to the culture, age, sexual preferences, behaviors, socioeconomic status, beliefs, and disabilities of patients and professional colleagues. 1,2,3 Describe the procedure for, and the significance of, maintaining medical licensure, board certification, credentialing, hospital staff privileges, and liability insurance. PC MK PBL ICS P SBP 1,2 x x 2,3 2 x x x GYN Level Uro Level ICS P SBP x x Use competency assessments for goal setting each semiannual period. Practice-Based Learning and Improvement PC MK PBL Fellow must be able to use scientific evidence and methods to investigate, evaluate, and improve patient care practices. Identify areas for personal and practice improvement and implement strategies to enhance knowledge, skills, attitudes, and processes of care, as well as making a commitment to life-long learning. x x x x x 1,2 x x x 2/3 2 x Demonstrate receptiveness to instruction and feedback. 1,2,3 1,2 Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness. 1,2,3 1,2 Use information technology to manage information, access online medical information, and support their education. 1,2,3 Facilitate the learning of students and other health care professionals. Participate actively in one or more planned project to improve the practice of FPMRS at UAB. Analyze and evaluate personal practice experience and implement strategies to continually improve the quality of patient care provided using a systematic methodology. Locate, appraise, and assimilate evidence from scientific studies related to their patients’ health problems. Obtain and use information about their population of patients and the larger population from which their patients are drawn. Use competency assessments for goal setting each semiannual period. 24 1,2,3 1,2 2/3 2 1,2,3 x x x x x x x x 1,2 x x 1,2,3 1,2 x x x 1,2,3 1,2 x x x x x x x x x GYN Level Systems-Based Practice Uro Level PC MK PBL ICS P SBP Fellow must demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value. Fellows are expected to: Describe how their patient care and other professional practices affect other health care professionals, the health care organization, and the larger society, and how these elements of the system affect their practices. Describe the processes for obtaining licensure, receiving hospital privileges and credentialing. 2/3 2 x x 1,2,3 1,2 x x List common systems of health care delivery, including various practice models. 2/3 2 x x Describe common methods of health care financing. 2/3 2 x x Discuss common business issues essential to running a medical practice. 2/3 2 1,2,3 1,2 Practice cost-effective health care and resource allocation that does not compromise quality of care. 1,2,3 1,2 x x x Advocate for quality patient care and assist patients in dealing with system complexities. 1,2,3 1,2 x x x Recognize that social, economic and political factors are powerful determinants of health and incorporate these factors into how they approach patient care. 1,2,3 1,2 x x x Demonstrate knowledge of disparities in health and health care in a variety of populations. 1,2,3 1,2 x x x Recognize the role of the women’s health provider to advocate for patients, particularly poor and vulnerable women, and to help develop methods of care that are effective, efficient, and accessible to all women. 1,2,3 1,2 x x x 2/3 2 x x x 1,2,3 1,2 x x x 2/3 2 x x x 1,2,3 1,2 x x x Describe how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources. Apply current procedural and diagnostic codes to reimbursement requests. Be aware of ACOG and AUG and community resources and advocacy on behalf of underserved and vulnerable populations such as poor women and teenagers. Communicate effectively about women’s health concerns to family and community groups. Recognize the role of the physician in legislation as it relates to women’s health policy. Communicate well with physicians and other providers in specialized other than your own to optimize the overall care of patients. 25 x x x x x x x x x x x x Systems-Based Practice GYN Level Uro Level PC MK PBL ICS P SBP Acknowledge that patient safety is always the first concern of the physician. 1,2,3 1,2 x x x x x x Demonstrate the ability to discuss errors in management with peers and patients to improve patient safety. 1,2,3 1,2 x x x x Develop and maintain a willingness to learn from errors and use errors to improve the system or process of care. 1,2,3 1,2 x x x x Participate in hospital/departmental QI activities and Patient Safety initiatives 1,2,3 1,2 x x x x Recognize the value of input from all members of the health care team and methods by which to facilitate communication among team members. 1,2,3 1,2 x x x x x Demonstrate understanding of institutional disclosure processes and participate in disclosure and discussions of adverse events with patients. 2/3 2 x x x x Partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance. 1,2,3 1,2 x x x x Describe the process of quality assessment and improvement including the role of clinical indicators, criteria sets, and utilization review. 2,3 2 x x x x Participate in organized peer review activities and use outcomes of such reviews to improve personal and system-wide practice patterns. 1,2,3 1,2 x x x x x Demonstrate an ability to cooperate with other medical personnel to correct system problems and improve patient care. 1,2,3 1,2 x x x x x 1,2,3 2 x x x x List the major types and providers of insurance. 2/3 2 Describe the most common reasons for professional liability claims. 2/3 2 Describe a systematic plan for minimizing the risk of professional liability claims in clinical practice. 2/3 2 Describe basic medical-legal concepts regarding a professional liability claim and list the steps in processing a claim. 2/3 2 Risk management and professional liability Use competency assessments for goal setting each semiannual period. 26 x x x x x x x x x x x x x x Section II FPMRS Specialty Specific Objectives Urogynecology Fellow or Three year Urology Fellow Acquired knowledge assignments for year 1 with completion expected during the first 6 months Pelvic Floor Anatomy (UG) Demonstrate knowledge of pelvic anatomy, including genital, urinary, colorectal, and musculoskeletal elements. Describe the vascular and nerve supply to each of the pelvic organs and structures, including the external genitalia, uterus, kidney, urethra, bladder, and recto-sigmoid. Explain the normal anatomic supports of the vagina, rectum, bladder, urethra, and uterus, including the bony pelvis, pelvic floor nerves and musculature, and connective tissue. Describe the inter-relationships and function of the pelvic organs and support mechanisms. MK Describe the anatomy, borders, and content of the pelvic and retroperitoneal spaces. MK Describe the anatomy of the anterior abdominal wall. Describe the vascular and nerve supply to the urethral and anal sphincter mechanisms. Describe and interpret normal and abnormal reproductive and urinary tract anatomy. MK MK MK Pelvic Floor Physiology (UG) Describe the normal function of the lower urinary tract during storage and micturition and the mechanisms responsible for urinary continence. Describe the physiology of colorectal function. MK Describe normal utero-vaginal physiology and function. Overactive Bladder (U) (UG) Cite the prevailing international definitions of urinary frequency urgency nocturia and overactive bladder syndrome. Discuss the indications characteristic findings and limitations of the following methods that may be used to diagnose overactive bladder syndrome: Clinical symptoms, Urinary diary, Urine, urethral cervical culture, Cystometry, Cystourethroscopy. General Pelvic Floor Evaluation (UG) Elicit a comprehensive medical history including a directed history that identifies all pelvic floor disorders, their type and severity. Urinary Incontinence (U) (UG) Perform a directed pelvic floor history including appropriate use of prevailing international terminology related to the signs and symptoms of urinary incontinence and lower urinary tract function and evaluation of: Urinary symptom severity and bother, including use of urinary diaries pad tests, and condition-specific bother, and quality of life questionnaires. Past medical obstetrical and surgical histories. Structural anatomic and congenital malformations. Current medications and their effects on urinary symptoms. Other organ systems including the nervous system and their effects on lower urinary tract function. Prior treatments and patient’s response. Surgical Treatment of Urinary Incontinence (U) (UG) Assist in and perform surgical procedures for stress incontinence which are felt to be applicable today (mid-urethral sling ( retropubic and transobutrator), Burch procedure, and autologous fascial slings. Understand the basic techniques of the commonly performed procedures in the past. ( Kelly and Pubo urethral ligament plications, MMK, Stamey, Raz, Pereyra and modifications thereof) MK MK, PBLI 27 MK MK MK MK MK PC MK, PC PC Describe indications, contraindications, intra and post operative complications, and their management , and avoidance, as well as, success rates of the following incontinence procedures: Periurethral bulk injections, Retropubic urethropexy (Marshall-Marchetti-Krantz, Burch, and paravaginal defect repair),Sling procedures, Fascial (fascia lata, rectus fascia),and Synthetic, Retropubic, and Transobturator Midurethral Sling procedures Identify evaluate and know management of complications associated with continence surgery. MK, PC Discuss role of urodynamic testing when planning continence surgery including. MK Discuss alternatives advantages disadvantages and evidence for prophylactic continence procedures at the time of vaginal and abdominal prolapse surgery in stress continent women. Behavioral Treatment (GR) Describe each of following behavioral treatments used to treat urinary incontinence. Timed voiding, Bladder training, Biofeedback, Pelvic floor muscle training, Electrical stimulation, other evidenced based treatments. Counsel patients on each of the behavioral interventions listed above specifically: List indications and contraindications, Cite published effectiveness rates, Explain frequency and types of side effects, Discuss long-term continuation and compliance rates, Evaluate the level of evidence for success and complication rates, List costs of treatment regimens. Functional Treatment (GR) Describe the following functional factors related to urinary incontinence: Mobility issues, Fecal impaction, Dementia, Hyperglycemia, Infection, Nocturnal polyuria, Medications, Sedatives, Hypnotics, Diuretics, Antidepressants. MK, PBLI, ICS Discuss the role and risks of each of the following functional interventions in the management of urinary incontinence: Fluid management, including evening restrictions, Change of pharmacologic agents or timing of their use (diuretics), Avoid nocturnal diuresis with decompression, CPAP, Optimize control of allergies, bronchitis, and chronic cough, Modification the environment (e.g., use of a bedside commode),Optimize bowel function and minimize constipation and fecal impaction, Modification of clothing to compensate for decreased dexterity, Intermittent self-catheterization, Absorbent products, Pessaries or tampons, Other evidenced based treatments, Counsel patients regarding hazards and limitations of chronic indwelling catheters. Fecal Incontinence Evaluation (UG) Elicit a comprehensive pelvic floor history including the following: Symptoms associated with fecal incontinence such as diarrhea, fecal urgency constipation or defecatory problems. Prevailing international terminology for anal incontinence. Determine fecal incontinence duration and severity, precipitating factors, and lifestyle modifications. Evaluate past medical, obstetrical, and surgical histories. Structural, anatomic and congenital malformations. Evaluate current medications and their effect on colorectal function. Evaluate other organ systems including neurologic, lower urinary tract and pelvic support, and their possible effects of the colorectal system. Determine psychosocial and psychosexual effects of fecal incontinence. Determine all prior therapies and responses. Perform a focused physical examination including: Neuromuscular examination with assessment of pelvic floor muscle and anal sphincter strength, pelvic floor reflexes, and perineal and anal sensory function. Identification of anal fistula, fissures, or scarring, perineal descent, rectal prolapse, hemorrhoids, tumor, and anal sphincter disruptions. MK, PC, ICS 28 MK, PC MK MK, PC, PBLI, ICS MK PC PC Interpret diagnostic tests to characterize anal incontinence and defecatory disorders and demonstrate knowledge of the following for each test: Standard terminology, normal values, and test reliability, Variations in instrumentation and technique, Indications, limitations, and cost-effectiveness, Results which require further testing. MK, PC Pelvic Organ Prolapse (UG) Elicit a focused prolapse symptom history. Discuss other pelvic floor symptoms and disorders and explain their relationship to pelvic organ prolapse. Explain the most common symptoms associated with prolapse and explain the relationship between symptoms and anatomy. Discuss various definitions of prolapse and normal support. Discuss lower urinary tract symptoms associated with pelvic organ prolapse and the role and methods for reduction stress testing. Discuss bowel symptoms associated with prolapse, including difficult defecation, splinting, or feeling of incomplete evacuation. Discuss relationship of prolapse with sexual activity and function. Perform a focused pelvic floor physical examination, assessing: Neurologic status (pelvic floor and lower limb reflexes and sensation). Pelvic floor muscle and anal sphincter strength. Pelvic organ support defects (identifying and quantifying all pelvic support defects using Pelvic Organ Prolapse Quantification (POP-Q) system. Urethral hypermobility. Sign of stress incontinence (reduction stress test) Describe factors that may affect severity of observed prolapse and alter POP-Q measures during examination (strain, supine vs. standing, etc.) Describe techniques to identify enteroceles and perineal descent. Non-surgical Treatment (UG) Discuss non-surgical and surgical treatment options for symptomatic anterior, apical, and posterior prolapse. Discuss role of pelvic floor physical therapy in management of prolapse. List factors which impact successful pessary fitting for prolapse, including: stage, genital hiatus, uterus, etc. Fit and manage prolapse pessaries. Discuss the advantages and disadvantages of the following pessary types: Ring with and without support Donut, Gelhorn, Gehrung, Lever, Cube Discuss the role of estrogen replacement therapy (systemic vs. local) in women using pessary for prolapse. Explain how recommendations differ based on presence or absence of uterus. Vesicovaginal, Urethrovaginal, and Ureterovaginal Fistulas (U) (UG) Describe risk factors for genitourinary fistulas (urethrovaginal, vesicovaginal, ureterovaginal, colovesical) and urethral diverticula. PC, ICS PC, MK MK MK MK MK MK PC MK MK MK MK MK, PC PC MK, PC MK, PC MK, PC MK Complete background study, hypothesis, feasibility, and plan for Thesis Project should be completed by the end of 1st 6 months. The thesis may be changed if completion of an alternative acceptable project is feasible by early in the last 6 months of the fellowship. Projects should be discussed with Dr. Richter and deemed acceptable, mentor(s) should be chosen and protocol draft and IRB application should be completed. Other research studies are expected to be performed during the duration of the fellowship all requiring the above planning. 29 Urogynecology Fellow or three year Urology Fellow: Acquired knowledge assignments for year 1 with completion expected during the second 6 months Epidemiology and Impact of disease (U) (UG) Urinary Incontinence Fecal Incontinence Defecatory dysfunction and Pelvic Organ Prolapse. Epidemiology and Demographics of fistulas from childbirth injury. Relationship of incontinence and prolapse to birth, aging, and neurologic disease. Impact of all pelvic floor disorders on Quality of Life. Know the disease specific and global health questionnaires use to evaluate them. Urinary Tract Infection (U) (UG) Obtain a pertinent patient history and diagnose urinary tract infection., (PC, ICS), Distinguish pathophysiology, including host factors, for lower and upper urinary tract infections. MK Describe diagnostic methods and diagnostic criteria for the various types of urinary tract infections. Describe techniques accuracy sensitivity specificity and interpretation of the following urine tests for primary and recurrent urinary tract infection. Urine dipstick analysis, Urine analysis, Urine culture. Describe the indications for the following tests for urinary tract infection. Cystourethroscopy, Upper tract imaging. MK MK Describe evidence for urinary tract infection treatment options including the following; Single dose therapy, Short-term (3-day) therapy, Longer treatment (7-10 days), Prophylactic treatment (daily versus coital), Non-microbial agents, probiotics, urine acidifiers. Administer and assess efficacy of appropriate therapy for acute, chronic, and complicated urinary tract infections. Overactive Bladder (U) (UG) Cite indications techniques response rates and side effects of the following: Biofeedback, Bladder Training, Neuromodulation, Pharmacologic agents including, Anticholinergics, Antispasmodics, Sedatives, Antidepressants, and Other evidenced based treatments. MK General Pelvic Floor Evaluation (UG) Perform a focused pelvic floor examination including assessment of uterovaginal support pelvic muscle strength neurologic status and uterine and ovarian size. Describe the techniques needed to diagnose different pelvic floor disorders including urinary incontinence and subtypes of lower urinary tract disorders, pelvic organ prolapsed and fecal incontinence using prevailing international terminology. Evaluate for co-existing environmental factors or diseases which may impact patient selection or response to treatment. Focused assessment of POP Q evaluation (UG) (Lisa Pair CRNP FPMRS faculty), List and Understand all causes of urinary incontinence due to both lower urinary tract dysfunction per se’ and that due to functional causes. (U) (UG) (GR) Urinary Incontinence (U) (UG) Perform a focused pelvic floor physical examination assessing: Neurologic status (pelvic floor and lower limb reflexes and sensation), Pelvic floor muscle and anal sphincter strength, Pelvic floor support defects – anterior apical and posterior, Urethral hyper-mobility, Structural anatomic and congenital malformations, Sign of stress incontinence (stress test). Complete Focused Assessment of Basic Urodynamics Evaluation (UG) PC Surgical Treatment of Urinary Incontinence (U) (UG) Describe the indications intra and postoperative complications and success of the following continence procedures: Kelly plication Needle suspension procedures (Pereyra Raz Stamey Gittes, Muzsnai), MK, PC 30 PC, ICS MK PC PC MK, PBLI MK, PC PC MK, PC, ICS MK, SBC, PC PC PC, P, MK Discuss differences in continence procedure success rates in women with and without urethral hypermobility. MK Discuss impact of concomitant prolapse surgery on continence procedure success rates. MK Pharmacological Treatment (U) (UG) (GR) Describe lower urinary tract receptors and mediators (detrusor bladder neck urethra) and potential sites for pharmacologic manipulation to treat various types of urinary incontinence. List the following for each class of drug used to treat urinary incontinence listed in #3 below. Indications and contraindications, Safe and effective dose, Published rates of effectiveness, Side effects and their prevalence, Rates of long-term continuation and compliance, Quality of studies establishing success and complication rates, Costs, Drugs Used to Treat Urinary Incontinence, Antimuscarinic agents, α-adrenergic agonists and antagonists, β-adrenergic agonists, Selective norepinephrine and serotonin uptake inhibitors, Tricyclic antidepressants, Neurotoxins (botulinum capsaicin resiniferatoxin), Fecal Incontinence Evaluation (UG) (GR) Diagnostic Tests for Fecal Incontinence and Defecatory Disorders Endoscopy including anoscopy, proctoscopy, and colonoscopy, Anal manometry, Anorectal sensory assessment, Measurement of rectal compliance, Defecography/ evacuation proctography/dynamic fluoroscopy, Neurophysiologic studies (e.g., electromyography, sacral reflexes, terminal motor latencies), Anal ultrasound, Levator and anal sphincter MRI, Fistulogram, Motility studies. Evaluate co-existing factors or diseases which may direct treatment selection and response. Complete Focused Assessment of Genitorectal Evaluation (UG) (Evaluator Dr. Richter or Ballard) Surgical Treatment (UG) Discuss the alternatives, risks, benefits, complications, success rates and levels of evidence for each of the following apical prolapse procedures. Sacrocolpopexy (open, laparoscopic, robotic), Vaginal mesh procedures (absorbable, non-absorbable, biologics), Uterosacral suspension, Sacrospinous ligament suspension, McCall’s culdeplasty, Illiococcygeous suspension, Colpocleisis, Manchester operation, Other evidenced based procedures. Discuss the alternatives, risks, benefits, complications, success rates, and levels of evidence for each of the following anterior prolapse procedures. Anterior colporrhaphy, Anterior vaginal repair with graft, Paravaginal repair, Other evidenced based procedures. Discuss the alternatives, risks, benefits, complications, success rates, and Levels of evidence for each of the following posterior prolapse procedures. Posterior colporrhaphy, Defect-specific posterior repair, Trans-anal repair, Posterior repair with graft, Perineorrhaphy, Other evidenced based procedures. Complete Pig Lab simulated Laparoscopic Sacrocolpopexy (UG) Complete Robotic SCP training Module (UG) Rectovaginal Fistula (UG) Describe risk factors for rectovaginal fistulas, including vaginal childbirth, operative vaginal delivery, episiotomy, pelvic radiation, inflammatory bowel disease, neoplasm. Describe appropriate techniques, imaging studies, and procedures to diagnose rectovaginal fistula, Fistulogram, Ultrasound. MK Complete Focused Assessment on Diagnostic Cystoscopy (U) PC, MK, SBP, ICS MK, SBP, PBLI, ICS Should have completed: Options for Understanding Research Design and Statistics, (UAB courses or Excellence in Research). Completion of this during year two is acceptable if a specific program can only be accomplished then. Complete Focused Assessment of Retropubic and Transobturator slings 31 MK, PC, PBLI PC,MK PC,MK PC PC,MK,PBLI,SBP MK, PC, PBLI MK, PC, PBLI MK, PC, PBLI PC, SBP, MK PC, SBP, MK MK MK, PC Urogynecology Fellow or Three Year Urology Fellow: Acquired knowledge assignments for year 2 with completion expected during the first 6 months General Pelvic Floor Evaluation (UG) Correlate findings on focused pelvic floor examination with the results of diagnostic testing to formulate a treatment plan. Urinary Incontinence (U) (UG) Perform and/or interpret the diagnostic tests listed below to characterize lower urinary tract disorders: Simple single urodynamics, Multi-channel urodynamics including video-urodynamics, Urethral pressure profilometry, Leak point pressures, Uroflowmetry (simple instrumented pressure flow studies), Urethral and anal sphincter electromyography, Neurophysiologic studies (e.g. electromyography sacral reflexes and terminal motor latency), Endoscopy (cystoscopy urethroscopy), Imaging studies (e.g. fluoroscopy ultrasound MRI), Pelvic floor muscle testing, Bladder cytology, Urinary microscopy and culture, PC Discuss each of the following as related to the diagnostic tests listed in #3 above. Standard terminology normal values and test reliability, Variations in instrumentation and technique, Technical specifications of the equipment or instrumentation, Indications limitations and costeffectiveness, Results which require further testing. MK Complete Focused Assessment on Retropubic and Transobturator Sling (U) (UG) Urogenital Fistulas (U) (UG) Vesicovaginal, Urethrovaginal, and Ureterovaginal Fistulas Describe alternative, risks, benefits, complications, success rates, and levels of evidence and techniques for the following procedures: Prolonged bladder drainage, TransVaginal repair of Vescico Vaginal Fistulas, Abdominal (open and minimally invasive), transvesical, and vaginal, Vesicovaginal fistula repairs, Vascular grafts (e.g., martius, omental), Ureteroneocystostomy, Psoas hitch, Boari flap, Transureteroureterostomy. PC, SBP, MK MK, PC, PBLI Describe how timing of repair influences outcomes. Describe postoperative care after genitourinary fistula and urethral diverticula repair: Postoperative bladder drainage, Antibiotics. Rectovaginal Fistula (UG) Describe operative technique to repair rectovaginal fistula and impact of location and etiology on technique. Discuss postoperative management of rectovaginal fistula repair. Congenital Anomalies (U) (UG) Describe the normal embryology of Mullerian and ovarian development Describe the pathogenesis of abnormal Mullerian development, including imperforate hymen, transverse vaginal septum, vaginal agenesis with and without a uterus. Evaluate and diagnose congenital anomalies of the urogenital tract. (MK) Discuss the relationship between genital anomalies and renal/lower urinary tract anomalies. Describe features of a patient’s history suggestive of a developmental anomaly of the urogenital tract. Interpret the following tests to diagnose a urogenital anomaly, its etiology, and potential clinical implications: Ultrasound, Endocrinologic assay (hormones), Karyotype assessment, CT or MRI, Endoscopic assessment (hysteroscopy, laparoscopy, cystoscopy, retrograde, pyelogram). Understand appropriate non-surgical and surgical techniques to treat urogenital anomalies, including imperforate hymen, vaginal agenesis with and without uterus, transverse vaginal septum, Mullerian anomalies. Discuss appropriate timing and indications for gonadectomy. Counsel patients and their families about the impact of urogenital anomalies on reproduction and timing of reconstruction. MK PC MK, PC 32 MK, PC, SBL MK, PC MK MK MK MK MK, PC PC MK ICS Sensory Disorders (U) Discuss the proposed theories and the levels of evidence regarding the pathophysiology of painful bladder syndrome. Diagnose painful bladder syndrome using prevailing international definitions and urinary diaries. MK, PBLI Explain the role of diet on the development or exacerbation of painful bladder symptoms. MK Perform and interpret cystourethroscopy, cytology, and bladder biopsy findings under anesthesia for painful bladder syndrome PC Describe the technique, indications, limitations, side effects and level of evidence for each of the following treatments: Hydrodistention of the bladder under anesthesia, Bladder instillation, Physical and behavioral therapy, Systemic therapy including, Immunosuppressive agents, such as corticosteroids, Antihistamines, Anti-inflammatory agents, Sodium pentosan polysulfate, Comprehensive pain management, Endoscopic surgical procedures, Surgical procedures, Bladder augmentation procedures, Urinary diversions, Other evidenced based therapies MK, PC, PBLI Neuro Urology (U) Describe the pathophysiology of neurologic conditions which affect the bladder and lower urinary tract. (MK) Elicit a complete neuro-urologic history elucidating relevant neurologic conditions and any gross motor and sensory deficits. MK Perform an accurate neurologic examination, including assessment of lower limb reflexes, sensory and motor function, perineal sensation and reflexes, and pelvic floor and anal sphincter muscle strength. Appropriately evaluate bladder storage and voiding function using urodynamic testing and prevailing international terminology. PC Describe the pathophysiology of the risks associated with neurogenic lower urinary tract dysfunction. Assess the risks of bladder dysfunction to upper urinary tract function. Formulate a management plan to protect the upper urinary tract from neurogenic bladder dysfunction. MK PC PC Discuss the pathophysiology and management of autonomic dysreflexia. Recognize and manage lower urinary symptoms related to neurologic disorders. MK PC Complete Focused Assessment on Retropubic and Transobutrator Mid-urethral slings. PC, MK,SBP,ICS 33 PC PC PC Urogynecology Fellow or Three Year Urology Fellow: Acquired knowledge assignments for year 2 with completion expected during the second 6 months Know the Embryological development of the genitor-urinary and colorectal structures and correlate anomalies of these structures to embryological defects. (U) (UG) Surgical Treatment of Urinary Incontinence (U) (UG) Cite published success and complication rates for each continence procedure, quality of studies and level of evidence. Discuss differences in success rates of primary and secondary continence procedures. MK, PC Complete Focused Evaluations (UG) High Uterosacral Intraperitaneal Suspension Michigan Sacrospinous Suspension Laparoscopic sarcolpopexy Ureteral Stint placement and Retrograde Pyelogram Vaginal reconstruction repair of total prolapsed (Procidentia a total vault prolapsed) PC,MK, PBLI,P,ICS Urogenital Fistulas (U) (UG) Vesicovaginal, Urethrovaginal, and Ureterovaginal Fistulas Treat genito-urinary fistulas and urethral diverticula. Understand the benefits and short comings and interpret the results of selected tests to diagnose genitourinary fistulas and diverticula. Tampon test, Cystourethroscopy, CT Urogram, MRI, Ultrasound, Retrograde pyelograms. PC 34 PBLI MK MK, PC Urogynecology Fellow: Acquired knowledge assignments for year 3 with completion expected during the first 6 months Thesis Project (see page 17) Write publishable scientific thesis. Must be in a form fulfill publication criteria for one of the following Journals: Obstetrical and Gynecology Journal of Urology American Journal of Obstetrics and Gynecology New England Journal of Medicine Study aims, Hypothesis, Study Plan Study population and generalizability of findings Inclusion and exclusion criteria Appropriate study design to answer specific aims Experimental, randomized, analytical, prospective/retrospective, observational Types of bias (selection, information, confounding) Appropriateness of control group Statistical (study) power Outcome measures Analysis of results (statistical tests and interpretations). Conclusions justified by findings and relevant to hypothesis. Participate in a problem based or system based learning quality improvement activity whereby a problem is identified and investigated, a potential solution or several solutions are proposed, then put into place with follow up investigation. The following GMS Health Stream Web Based or Formal Lecture Based programs with a passing grade on Post-test Evaluations should be completed. (U) (UG) (R) Quality/ Patient Safety Professionalism with staff and patients (AIDET) Information System – Rules of Behavior Safety and Clinical Competency 2011 Corporate Compliance Confidentiality Conflict and Disclosures Stress and Substance Abuse Sleep Deprivation (Prevention, Recognition and Responsibility Diversity Training (Cultural, Race, Ethnic) Attend Obstetrics and Gynecology Ethics Grand Rounds held quarterly Complete Modified Focus Assessments (UG) Vaginal repair of Vesicovaginal Fistula Vaginal Repair of Recto Vaginal Fistula (UG) Abdominal repair of Vesicovaginal Fistula (U) (UG) 35 MK, PBLI, SBP, ICS PBC, P, SBP, MK, ICS P, MK, SBP, ICS PC, MK, ICS PC, MK, ICS PC, MK, ICS Urologist (2 year program): Acquired knowledge assignments for year 1 with completion expected during the first 6 months Pelvic Floor Anatomy (UG) Demonstrate knowledge of pelvic anatomy, including genital, urinary, colorectal, and musculoskeletal elements. Describe the vascular and nerve supply to each of the pelvic organs and structures, including the external genitalia, uterus, kidney, urethra, bladder, and recto-sigmoid. Explain the normal anatomic supports of the vagina, rectum, bladder, urethra, and uterus, including the bony pelvis, pelvic floor nerves and musculature, and connective tissue. Describe the inter-relationships and function of the pelvic organs and support mechanisms. Describe the anatomy, borders, and content of the pelvic and retroperitoneal spaces. MK Describe the anatomy of the anterior abdominal wall. Describe the vascular and nerve supply to the urethral and anal sphincter mechanisms. Describe and interpret normal and abnormal reproductive and urinary tract anatomy. Pelvic Floor Physical (UG) Describe the normal function of the lower urinary tract during storage and micturition and the mechanisms responsible for urinary continence. MK MK MK MK Describe the physiology of colorectal function. Describe normal utero-vaginal physiology and function. Overactive Bladder(U) (UG) Cite the prevailing international definitions of urinary frequency urgency nocturia and overactive bladder syndrome. MK MK MK, PBLI Discuss the indications characteristic findings and limitations of the following methods that may be used to diagnose overactive bladder syndrome: Clinical symptoms, Urinary diary, Urine, urethral cervical culture, Cystometry, Cystourethroscopy, General Pelvic Floor Evaluation (UG) Elicit a comprehensive medical history including a directed history that identifies all pelvic floor disorders, their type and severity. Urinary Incontinence (U) (UG) Perform a directed pelvic floor history including appropriate use of prevailing international terminology related to the signs and symptoms of urinary incontinence and lower urinary tract function and evaluation of: Urinary symptom severity and bother, including use of urinary diaries pad tests and condition-specific bother and quality of life questionnaires Past medical obstetrical and surgical histories Structural anatomic and congenital malformations, Current medications and their effects on urinary symptoms, Other organ systems including the nervous system and their effects on lower urinary tract function, Prior treatments and patient’s response, Surgical Treatment of Urinary Incontinence (U) (UG) Assist in and perform surgical procedures for stress incontinence which are felt to be applicable today (mid-urethral sling retropubic and transobutrator burch procedure and understand the basic techniques of the commonly performed procedures in the past (MMK Stamey Raz Pereyra and modifications). Describe the indications intra and postoperative complications and success of the following continence procedures: Periurethral bulk injections, Retropubic urethropexy (Marshall-Marchetti-Krantz, Burch, and paravaginal defect repair), Sling procedures, Fascial (fascia lata, rectus fascia), Synthetic, Retropubic, Transobutrator, Identify evaluate and know management of complications associated with continence surgery. Discuss role of urodynamic testing when planning continence surgery. MK 36 MK MK MK MK PC MK, PC PC MK, PC MK, PC MK Discuss alternatives advantages disadvantages and evidence for prophylactic continence procedures at the time of vaginal and abdominal prolapse surgery in stress continent women. Complete Focused Assessment on Diagnostic Cystoscopy (U) Behavioral Treatment (GR) Describe each of following behavioral treatments used to treat urinary incontinence. Timed voiding, Bladder training, Biofeedback, Pelvic floor muscle training, Electrical stimulation, Other evidenced based treatments. MK, PBLI, ICS Counsel patients on each of the behavioral interventions listed above specifically: (MK, PC, PBLI, ICS) List indications and contraindications, Cite published effectiveness rates, Explain frequency and types of side effects, Discuss long-term continuation and compliance rates, Evaluate the level of evidence for success and complication rates, List costs of treatment regimens. Functional Treatment (GR) Describe the following functional factors related to urinary incontinence: Mobility issues, Fecal impaction, Dementia, Hyperglycemia, Infection, Nocturnal polyuria, Medications, Sedatives, Hypnotics, Diuretics, Antidepressants. MK, PC, PBLI, ICS Discuss the role and risks of each of the following functional interventions in the management of urinary incontinence. Fluid management, including evening restrictions, Change of pharmacologic agents or timing of their use (diuretics), Avoid nocturnal diuresis with decompression, CPAP, Optimize control of allergies, bronchitis, and chronic cough, Modification the environment (e.g., use of a bedside commode), Optimize bowel function and minimize constipation and fecal impaction, Modification of clothing to compensate for decreased dexterity, Intermittent self-catheterization, Absorbent products, Pessaries or tampons, Other evidenced based treatments. Counsel patients regarding hazards and limitations of chronic indwelling catheters. MK Fecal Incontinence Evaluation (UG) (GR) Elicit a comprehensive pelvic floor history including the following: Symptoms associated with fecal incontinence such as diarrhea, fecal urgency constipation or defecatory problems, Prevailing international terminology for anal incontinence, Determine fecal incontinence duration and severity, precipitating factors, and lifestyle modifications, Evaluate past medical, obstetrical, and surgical histories, Structural, anatomic and congenital malformations, Evaluate current medications and their effect on colorectal function, Evaluate other organ systems including neurologic, lower urinary tract and pelvic support, and their possible effects of the colorectal system, Determine psychosocial and psychosexual effects of fecal incontinence. Determine all prior therapies and responses, Perform a focused physical examination including: Neuromuscular examination with assessment of pelvic floor muscle and anal sphincter strength, pelvic floor reflexes, and perineal and anal sensory function, PC Identification of anal fistula, fissures, or scarring, perineal descent, rectal prolapse, hemorrhoids, tumor, and anal sphincter disruptions, Interpret diagnostic tests listed in #4 below to characterize anal incontinence and defecatory disorders and demonstrate knowledge of the following for each test: Standard terminology, normal values, and test reliability, Variations in instrumentation and technique, Indications, limitations, and costeffectiveness, Results which require further testing, MK, PC Pelvic Organ Prolapse (UG) Elicit a focused prolapse symptom history. Discuss other pelvic floor symptoms and disorders and explain their relationship to pelvic organ prolapse. Explain the most common symptoms associated with prolapse and explain the relationship between symptoms and anatomy. Discuss various definitions of prolapse and normal support. Discuss lower urinary tract symptoms associated with pelvic organ prolapse and the role and methods for reduction stress testing. Discuss bowel symptoms associated with prolapse, including difficult defecation, splinting, or feeling of incomplete evacuation. Discuss relationship of prolapse with sexual activity and function. PC, ICS 37 PC, MK, SBP, ICS MK MK MK, PC, ICS PC PC, MK MK MK MK MK MK Perform a focused pelvic floor physical examination, assessing: Neurologic status (pelvic floor and lower limb reflexes and sensation), Pelvic floor muscle and anal sphincter strength, Pelvic organ support defects (identifying and quantifying all pelvic support defects using Pelvic Organ Prolapse Quantification (POP-Q) system, Urethral hypermobility, Sign of stress incontinence (reduction stress test) Describe factors that may affect severity of observed prolapse and alter POP-Q measures during examination (strain, supine vs. standing, etc.). PC Describe techniques to identify enteroceles and perineal descent. Non-surgical Treatment (UG) Discuss non-surgical and surgical treatment options for symptomatic anterior, apical, and posterior prolapse. Discuss role of pelvic floor physical therapy in management of prolapse. List factors which impact successful pessary fitting for prolapse, including: stage, genital hiatus, uterus, etc. Fit and manage prolapse pessaries. Discuss the advantages and disadvantages of the following pessary types: Ring with and without support, Donut, Gelhorn, Gehrung, Lever, Cube. Discuss the role of estrogen replacement therapy (systemic vs. local) in women using pessary for prolapse. Explain how recommendations differ based on presence or absence of uterus. Urogenital Fistulas (U) (UG) Vesicovaginal, Urethrovaginal, and Ureterovaginal Fistulas Describe risk factors for genitourinary fistulas (urethrovaginal, vesicovaginal, ureterovaginal, colovesical) and urethral diverticula. MK MK Sensory Disorders (U) Discuss the proposed theories and the levels of evidence regarding the pathophysiology of painful bladder syndrome. Diagnose painful bladder syndrome using prevailing international definitions and urinary diaries. Explain the role of diet on the development or exacerbation of painful bladder symptoms. Perform and interpret cystourethroscopy, cytology, and bladder biopsy findings under anesthesia for painful bladder syndrome. Describe the technique, indications, limitations, side effects and level of evidence for each of the following treatments. Hydrodistention of the bladder under anesthesia, Bladder instillation, Physical and behavioral therapy, Systemic therapy including, Immunosuppressive agents, such as corticosteroids, Antihistamines, Anti-inflammatory agents, Sodium pentosan polysulfate, Comprehensive pain management, Endoscopic surgical procedures, Surgical procedures, Bladder augmentation procedures, Urinary diversions, Other evidenced based therapies Neuro Urology (U) Describe the pathophysiology of neurologic conditions which affect the bladder and lower urinary tract. Elicit a complete neuro-urologic history elucidating relevant neurologic conditions and any gross motor and sensory deficits. Perform an accurate neurologic examination, including assessment of lower limb reflexes, sensory and motor function, perineal sensation and reflexes, and pelvic floor and anal sphincter muscle strength. Appropriately evaluate bladder storage and voiding function using urodynamic testing and prevailing international terminology. (PC) MK, PBLI MK MK MK, PC PC MK, PC MK, PC MK, PC MK PC MK PC MK, PC, PBLI MK PC PC Describe the pathophysiology of the risks associated with neurogenic lower urinary tract dysfunction. (MK) MK Assess the risks of bladder dysfunction to upper urinary tract function. (PC) PC Formulate a management plan to protect the upper urinary tract from neurogenic bladder dysfunction. (PC) PC Discuss the pathophysiology and management of autonomic dysreflexia. (MK) MK Recognize and manage lower urinary symptoms related to neurologic disorders. (PC) PC Complete background study, hypothesis, feasibility, and plan for Thesis Project should be completed by the end of 1st 6 months. The thesis may be changed if completion of an alternative acceptable project is feasible by early in the last 6 months of the fellowship. Projects should be discussed with Dr. Richter and deemed acceptable, mentor(s) should be chosen and protocol draft and IRB application should be completed. Other research studies are expected to be performed during the duration of the fellowship all requiring the above planning. 38 Urologist: Acquired knowledge assignments for year 1 with completion expected during the second 6 months Epidemiology and Impact of disease (U) (UG) Urinary Incontinence Fecal Incontinence Defecatory dysfunction and Pelvic Organ Prolapse, Epidemiology and Demographics of fistulas from childbirth injury, Relationship of incontinence and prolapse to birth, aging, and neurologic disease, Impact of all pelvic floor disorders on Quality of Life, Know the disease specific and global health questionnaires use to evaluate them, MK Know the Embryological development of the genitor-urinary and colorectal structures and correlate anomalies of these structures to embryological defects (U) (UG) Urinary Tract Infection(U) (UG) Obtain a pertinent patient history and diagnose urinary tract infection. Distinguish pathophysiology, including host factors, for lower and upper urinary tract infections. MK, PC Describe diagnostic methods and diagnostic criteria for the various types of urinary tract infections. Describe techniques accuracy sensitivity specificity and interpretation of the following urine tests for primary and recurrent urinary tract infection: Urine dipstick analysis, Urine analysis, Urine culture. Describe the indications for the following tests for urinary tract infection: Cystourethroscopy, Upper tract imaging. Describe evidence for urinary tract infection treatment options including the following: Single dose therapy, Short-term (3-day) therapy, Longer treatment (7-10 days), Prophylactic treatment (daily versus coital), Non-microbial agents, probiotics, urine acidifiers. Administer and assess efficacy of appropriate therapy for acute, chronic, and complicated urinary tract infections. Overactive Bladder (U) (UG) Cite indications techniques response rates and side effects of the following: Biofeedback, Bladder Training, Neuromodulation, Pharmacologic agents including, Anticholinergics, Antispasmodics, Sedatives, Antidepressants, and Other evidenced based treatments. General Pelvic Floor Evaluation (UG) Elicit a comprehensive medical history including a directed history that identifies all pelvic floor disorders, their type and severity. Perform a focused pelvic floor examination including assessment of uterovaginal support pelvic muscle strength neurologic status and uterine and ovarian size. Correlate findings on focused pelvic floor examination with the results of diagnostic testing to formulate a treatment plan. Describe the techniques needed to diagnose different pelvic floor disorders including urinary incontinence and subtypes lower urinary tract disorders, pelvic organ prolapsed and fecal incontinence using prevailing international terminology. Evaluate for co-existing environmental factors or diseases which may impact patient selection or response to treatment. Focused assessment of POP Q evaluation (Lisa Pair CRNP FPMRS faculty) (UG) List and Understand all causes of urinary incontinence due to both lower urinary tract dysfunction per SE’ and that due to functional causes. (UG) (GR) Urinary Incontinence (U) (UG) Perform a focused pelvic floor physical examination assessing: Neurologic status (pelvic floor and lower limb reflexes and sensation), Pelvic floor muscle and anal sphincter strength, Pelvic floor support defects – anterior apical and posterior, Urethral hyper-mobility, Structural anatomic and congenital malformations, Sign of stress incontinence (stress test), Complete Focused Assessment of Basic Urodynamics Evaluation. (Lisa Pair CRNP FPMRS faculty) (UG) Surgical Treatment of Urinary Incontinence (U) (UG) Describe the indications intra and postoperative complications and success of the following continence procedures. MK MK 39 PC, ICS MK PC MK PC MK, PBLI PC PC PC MK, PC PC MK, SBC, PC PC PC, P, MK MK, PC Discuss differences in continence procedure success rates in women with and without urethral hypermobility, (Kelly placation Needle suspension procedures (Pereyra Raz Stamey Gittes, Muzsnai). MK Discuss impact of concomitant prolapse surgery on continence procedure success rates. Complete Focused Assessment on Retropubic and Transobutrator Mid-urethral slings. (U) (UG) Pharmacological Treatment (U) (UG) (GR) Describe lower urinary tract receptors and mediators (detrusor bladder neck urethra) and potential sites for pharmacologic manipulation to treat various types of urinary incontinence. List the following for each class of drug used to treat urinary incontinence listed in #3 below: Indications and contraindications, Safe and effective dose, Published rates of effectiveness, Side effects and their prevalence, Rates of long-term continuation and compliance, Quality of studies establishing success and complication rates, Costs, Drugs Used to Treat Urinary Incontinence, Antimuscarinic agents, α-adrenergic agonists and antagonists, β-adrenergic agonists, Selective norepinephrine and serotonin uptake inhibitors, Tricyclic antidepressants, Neurotoxins (botulinum capsaicin resiniferatoxin). Fecal Incontinence Evaluation (UG) Evaluate co-existing factors or diseases which may direct treatment selection and response. Complete Focused Assessment of Genitorectal Evaluation (Evaluator Dr. Richter or Ballard) (UG) Surgical Treatment (UG) Discuss the alternatives, risks, benefits, complications, success rates and levels of evidence for each of the following apical prolapse procedures: Sacrocolpopexy (open, laparoscopic, robotic) Vaginal mesh procedures (absorbable, non-absorbable, biologics) Uterosacral suspension, Sacrospinous ligament suspension, McCall’s culdeplasty, Illiococcygeous suspension, Colpocleisis, Manchester operation, Other evidenced based procedures Discuss the alternatives, risks, benefits, complications, success rates, and levels of evidence for each of the following anterior prolapse procedures: Anterior colporrhaphy, Anterior vaginal repair with graft, Paravaginal repair, Other evidenced based procedures Discuss the alternatives, risks, benefits, complications, success rates, and levels of evidence for each of the following posterior prolapse procedures: Posterior colporrhaphy, Defect-specific posterior repair, Trans-anal repair, Posterior repair with graft, Perineorrhaphy, Other evidenced based procedures Complete Pig Lab simulated Laparoscopic Sacrocolpopexy (UG) Ureteral Stint placement (U) Retrograde Pyelogram Rectovaginal Fistula (U) Describe risk factors for rectovaginal fistulas, including vaginal childbirth, operative vaginal delivery, episiotomy, pelvic radiation, inflammatory bowel disease, neoplasm. Describe appropriate techniques, imaging studies, and procedures to diagnose rectovaginal fistula, Fistulogram, Ultrasound Should have completed required (Progress in Research Design and Statistics) MK PC, MK, SBP, ICS MK 40 MK, PC, PBLI PC PC,MK,PBLI,P MK, PC, PBLI MK, PC, PBLI MK, PC, PBLI PC, SBP, MK MK MK MK, PC Urologist: Acquired knowledge assignments for year 2 with completion expected during the first 6 months General Pelvic Floor Evaluation (UG) Correlate findings on focused pelvic floor examination with the results of diagnostic testing to formulate a treatment plan. Urinary Incontinence (U) (UG) Perform and/or interpret the diagnostic tests listed below to characterize lower urinary tract disorders: Simple single urodynamics, Multichannel urodynamics including video-urodynamics, Urethral pressure profilometry, Leak point pressures, Uroflowmetry (simple instrumented pressure flow studies), Urethral and anal sphincter electromyography, Neurophysiologic studies (e.g. electromyography sacral reflexes and terminal motor latency), Endoscopy (cystoscopy urethroscopy), Imaging studies (e.g. fluoroscopy ultrasound MRI), Pelvic floor muscle testing, Bladder cytology, Urinary microscopy and culture, Discuss each of the following as related to the diagnostic tests listed in #3 above: Standard terminology normal values and test reliability, Variations in instrumentation and technique, Technical specifications of the equipment or instrumentation, Indications limitations and costeffectiveness, Results which require further testing, Surgical Treatment of Urinary Incontinence (U) (UG) Cite published success and complication rates for each continence procedure, quality of studies and level of evidence. Discuss differences in success rates of primary and secondary continence procedures. Complete Robotic SCP training Module (UG) Complete Focused Evaluations (UG) High Uterosacral Intraperitaneal Suspension Michigan Sacrospinous Suspension Vaginal reconstruction repair of total prolapsed (Procidentia a total vault prolapsed) Urogenital Fistulas Vesicovaginal, Urethrovaginal, and Ureterovaginal Fistulas (U) (UG) Treat genito-urinary fistulas and urethral diverticula. Understand the benefits and short comings and interpret the results of selected tests to diagnose genitourinary fistulas and diverticula: Tampon test, Cystourethroscopy, CT Urogram, MRI, Ultrasound, Retrograde pyelograms. PC Describe alternative, risks, benefits, complications, success rates, and levels of evidence and techniques for the following procedures: Prolonged bladder drainage, TransVaginal repair of Vescico Vaginal Fistulas, Abdominal (open and minimally invasive), transvesical, and vaginal vesicovaginal fistula repairs, Vascular grafts (e.g., martius, omental), Ureteroneocystostomy, Psoas hitch, Boari flap, Transureteroureterostomy MK, PC, PBLI Describe how timing of repair influences outcomes. Describe postoperative care after genitourinary fistula and urethral diverticula repair: Postoperative bladder drainage, Antibiotics Congenital Anomalies (U) (UG) Describe the normal embryology of Mullerian and ovarian development. Describe the pathogenesis of abnormal Mullerian development, including imperforate hymen, transverse vaginal septum, and vaginal agenesis with and without a uterus. Evaluate and diagnose congenital anomalies of the urogenital tract. Discuss the relationship between genital anomalies and renal/lower urinary tract anomalies. Describe features of a patient’s history suggestive of a developmental anomaly of the urogenital tract. Interpret the following tests to diagnose a urogenital anomaly, its etiology, and potential clinical implications: Ultrasound, Endocrinologic assay (hormones), Karyotype assessment, CT or MRI, Endoscopic assessment (hysteroscopy, laparoscopy, cystoscopy, retrogradepyelogram). Understand appropriate non-surgical and surgical techniques to treat urogenital anomalies, including imperforate hymen, vaginal agenesis with and without uterus, transverse vaginal septum, Mullerian anomalies. MK PC MK 41 MK, PC, SBL MK PBLI MK PC, SBC, MK PC,MK, SBP, PBLI,P ICS PC MK, PC MK MK MK MK MK, PC PC Discuss appropriate timing and indications for gonadectomy. MK Understand the counseling of patients and their families about the impact of urogenital anomalies on reproduction and timing of reconstruction. ICS Thesis Project (see page 17) Write publishable scientific thesis. Must be in a form fulfill publication criteria for one of the following Journals: Obstetrical and Gynecology, Journal of Urology, American Journal of Obstetrics and Gynecology, New England Journal of Medicine. MK, PBLI, SBP, ICS Study aims: Study population and generalizability of findings, Inclusion and exclusion criteria, Appropriate study design to answer specific aims Experimental, randomized, analytical, prospective/retrospective, observational, Types of bias (selection, information, confounding) Appropriateness of control group, Statistical (study) power, Outcome measures, Analysis of results is appropriate (statistical tests and interpretations), Conclusions justified by findings and relevant to hypothesis. Participate in a problem based or system based learning quality improvement activity whereby a problem is identified and investigated, a potential solution or several solutions are proposed, then put into place with follow up investigation (U) (UG) (R) Perform the following GMS Health Stream Web Based or Formal Lecture Based programs with a passing grade on Post-test Evaluations. (U) (UG) (R) Quality/ Patient Safety, Professionalism with staff and patients (AIDET), Information System – Rules of Behavior, Safety and Clinical, Competency 20111, Corporate Compliance, Confidentiality, Conflict and Disclosures, Stress and Substance Abuse, Sleep Deprivation (Prevention, Recognition and Responsibility Diversity Training (Cultural, Race, Ethnic), Attend Obstetrics and Gynecology Ethics Grand Rounds held quarterly. MK,ICS,PBLI,SBP,P 42 PBC, P, SBP, MK, ICS MK, SBP, ICS, P Urologist: Acquired knowledge assignments for year 2 with completion expected during the second 6 months Complete Focused Evaluations Laparoscopic sacrocolpopexy Rectovaginal Fistula Describe operative technique to repair rectovaginal fistula and impact of location and etiology on technique. Discuss postoperative management of rectovaginal fistula repair. Complete Modified Focus Assessments Vaginal repair of Vesico Vaginal Fistula Vaginal Repair of Rectovaginal Fistula Abdominal repair of Vesicovaginal Fistula Thesis Project should be complete during this 6 month period 43 PC,MK,PBLI,ICS,P MK, PC MK, PC PC, MK, ICS PC, MK, ICS PC, MK, ICS Milestones Topics Patient Care: General Pelvic Floor Evaluation UI and Overactive Bladder Treatment Anal Incontinence & Defecatory Dysfunction Treatment POP Treatment Urogental Fistula & Urethral Diverticula Treatment Painful Bladder Syndrome Treatment UTI Medical Knowledge: Pelvic Floor Anatomy & Physiology UI and Overactive Bladder Treatment Anal Incontinence & Defecatory Dysfunction Treatment POP Treatment Urogental Fistula & Urethral Diverticula Treatment Painful Bladder Syndrome Treatment UTI Neuro Urology System Based Practice: Computer Systems Health Care Economics Works & Coordinates Patient Care Effectively in Various Health Care Delivery setting & system 44 XII. Research Requirements Oral Examination: Thesis A thesis is required by the Division of Female Pelvic Medicine and Reconstructive Surgery. The thesis will be reviewed by the committee for acceptability, presented to the faculty and fellows in FPMRS and Thesis Committee at UAB, and defended. Approval by the Committee and FPMRS Division Faculty is a requirement for entrance to the Oral Board Examination and Board approval is necessary for certification. The thesis need not have been published or accepted for publication at the time of submission for the Oral Board Examination. Acceptance of a thesis for publication by a refereed journal does not guarantee acceptance of the thesis for the oral examination (Appendix C). Appendix C: Thesis The following information is provided to allow the candidate to see the subspecialty thesis requirements that are in effect for the oral examinations in MFM, REI and Gyn Oncology and for FPMRS. Candidates are responsible for preparing a thesis that meets the requirements for the year they are applying to take the oral examination. Preparation 1. Format: The format of the thesis must comply with the instructions for authors for one of the following journals: (1) American Journal of Obstetrics and Gynecology; (2) The New England Journal of Medicine; (3) Obstetrics and Gynecology, (4) Journal of Urology, (5) Urology, (6) Neurology and Urodynamics and (7) Female Pelvic Medicine and Reconstructive Surgery. The chosen format must be clearly identified on the cover page of the manuscript. The manuscript may not exceed 30 pages in length, and the pages must be numbered. The thesis must be type-written in 12 point type, single-spaced, and double-sided on standard 8 1/2 x 11 paper. Reprints of published manuscripts are not acceptable. The applicant must be the sole or principal investigator and should be the only author listed on the manuscript. Do not list co-authors, institutions, or acknowledgments. No more than one thesis may be submitted. 2. Subject Matter: The subject matter should clearly relate to the area of Female Pelvic Medicine and Reconstructive Surgery. 3. Research: The thesis may report a clinical, translational, or basic science based research project performed during the fellowship period. A review of work performed by others is not acceptable. 4. IRB Approval: All research involving humans and animals must be reviewed and approved by the human or animal institutional review boards (IRBs) of the sponsoring institution. If the research is considered to be exempt from IRB approval, a statement from the IRB to that effect must be included with the thesis. 5. Thesis Content: The thesis must be a scholarly effort that most often should include the following sections: a. Abstract: A concise statement of the work performed limited to 300 words; b. Introduction: A short summary of the pertinent background and reasons for the project, as well as, when appropriate, a testable hypothesis and a rationale for the hypothesis; c. Methodology: If the thesis is based on bench research, a short description of the techniques used, including the quality control of the methods, must be included. If the thesis is based on clinical research, a description of the study and control groups and their appropriateness, as well as a power analysis is required; d. Statistical Approach: A description of the analyses performed must be included, and support of the chosen statistical techniques will be part of the defense of thesis during the oral examination. e. Discussion: Pertinent discussion and significance of the study, including an appropriate review of the literature and justification of the conclusion(s) reached must be included; f. Conclusions: A short summary of results based on the findings of the study must be included; and g. References: Appropriate references must be included. The pages listing the references should be counted in the 30 page limit. 6. Unacceptable Papers: The following are not acceptable for a Fellow’s thesis: a. book chapters, b. clinical case reports, c. descriptive series, d. systemic reviews and meta-analyses 45 e. cost-efficiency or cost-effective analyses f. results of patient surveys 7. Thesis Defense: As above during the last 6 months of Fellowship and during the oral examination, the candidate may be asked one or all of the following questions. Additional questions may be asked which are not listed in this outline. a. Hypothesis 1) What were the study objectives? 2) What was the population studied? 3) What was the population to which the investigators intended to apply their findings? b. Design of the investigation 1) Was the study an experiment, case control study, randomized clinical trial, planned observations, or a retrospective analysis of records? 2) Were there possible sources of sample selection bias? 3) How comparable was the control group? 4) What was the statistical power of the study? 5) Was the design of the study appropriate for the hypothesis to be tested? c. Observations 1) Were there clear definitions of the terms used (i.e., diagnostic criteria, inclusion criteria, measurements made and outcome variables)? 2) Were the observations reliable and reproducible? 3) What were the sensitivity, specificity and predictive values of the methods? d. Presentation of findings 1) Were the findings presented clearly, objectively, and in sufficient detail? 2) Were the findings internally consistent (i.e., did the numbers add up properly and could the different tables be reconciled, etc). Fellows will generally perform and or participate in several other studies during their fellowship. They may choose to serve as a mentor to residents or medical students, but this would be a special circumstance where the fellow is specifically over-seeing a project where the mentee has an interest in the field. All proposed projects will be expected to pass through the phases of protocol development: 1. Concept outline: A brief summary of the project overall goals should be organized as: Title, Hypotheses, Target population, Study design, Primary outcome, Second outcome(s), Clinical significance, Feasibility, Proposed statistical approach. This concept will be presented to the Fellowship Research Group for comments, advice. 2. Proposal: This is an extended (usually less than 6 pages) explanation of the protocol. This should include the following sections: Title, Potential collaborators as co-investigators, Brief introduction, Hypothesis, Aims, Significance, Approach (to include - Study design, methods, procedure, and materials), Statistical approach (to include - sample size/power analysis, evaluation of outcomes), Feasibility, Timeline, and Plan for personnel/funding. 46 Statistical resources: If department statistical effort is to be sought, it will need to be presented to the department Center for Research in Women’s Health (CRWH) over-sight committee and prioritized. If you plan to seek statistical support through the Center for Clinical and Translational Sciences (CCTS), the fellow will meet with a biostatistician during a twice monthly biostatistics clinic for statistical over-sight. This biostatistician will be a designated investigator of your study/trial. The IRB approval process will be over-seen directly by the fellow with input and over-sight by one of the Urogynecology division’s nurse managers (Ms Alice Howell or Velria Willis). Fellows will be responsible for completion of all initial review, renewals, amendments, etc for each project. A faculty mentor will give guidance for these studies as well. It is ideally expected that all projects be completed and written by the end of your fellowship. A research instruction and policy manual has been developed by Dr. Richter and research staff, Allie Howell and Velria Willis and includes basic references to research design and statistics as well as UAB IRB and conflict of interest policies. This manual will be reviewed in detail at the fellowship orientation that is held during the first week of fellowship. 47 XIII. Academic and Service Portfolio (Items in italics will be monitored and summaries provided by the Coordinator) 1. CV 2. Credentialing 3. Contracts 4. HealthStream 5. Learning Bibliography 6. Manuscripts 7. Research Proposals/Projects 8. Research Report from Dr. Richter 9. Article Reviews 10. Surgical Case List in ACGME format 11. PA OB/GYN Lecture, Conferences or lecture presentations, fellows’ conference, resident and student conference and lecture, grand rounds, presentation’s at local or national meetings. 12. Scholar Activities/ Article Reviews 13. Duty Hours 14. Evaluations a. Rotation Evaluations by Faculty b. Clinical Focused Assessments c. Surgical Focused Assessments d. Presentation Evaluations e. Global Competency Evaluations: student, patient, health care professionals, nurse, as well as, semiannually by Faculty, and residents f. Milestone Assessments g. Semiannual Assessment by Fellowship Director and Competency Committee h. Oral Exam August 3rd for UROGYN March 2nd for Urology 15. Fellows Self Evaluations, Assessments and goal setting 48 XIV. Healthstream Requirements: Hospital requires all Physician trainees to participate in scheduled lectures and/or webinar type programs on the following topics and others which are added each year. Fellows’ participation in this program is required. IMPACT Annual Corporate Compliance UAB Medicine Hazard Communication Confidentiality Form UABHS GME Lecture#1: (various topics) GME Lecture#2: (various topics) GME Lecture#3: (various topics) GME Lecture #4: (various topics) GME TB TEST NOTICE Hand Hygiene Pledge Patient Safety Clinical Competency Rapid Regs – Clinical I (UAB Medicine): Compliance, Ethics, Sexual Har, Workplace Har, Pt Rights, Informed Consent, Adv. Directives, Grievances, Dev Appro Care, Pop Specific Care, Cult. Competence, Restraints, Patient Abuse/Assault/Neglect Rapid Regs - Clinical II (UAB Medicine): Gen/Fire/Elec/Back/Rad./MRI Safety, Ergo, Lift/Transp, Slips/Trips/Falls, LatexAllergy, HazComm, WorkplaceViol.,EmergPrep, Infec.Control:HAI, HandHyg, Bloodborne, StdPrec, PPE Rules of Behavior-Information Systems (UABHS) UAB Residents as Teachers Program: Teaching Procedures to Medical Students UAB Residents as Teachers: Teaching Medical Students in the Operating Room 49 XV. Policies and Procedures for Duty Hours and Work Environment Duty hours are defined as all clinical and academic activities related to the fellowship program; i.e., patient care (both inpatient and outpatient), administrative duties related to patient care, the provision for transfer of patient care, time spent in-house during call activities, and scheduled academic activities such as conferences. Duty hours do not include reading and preparation time spent away from the duty site. Purpose: In compliance with the ACGME Institutional and Common Program Requirements, it is the goal of the Hospital as the Sponsoring Institution to provide residents/fellows with a sound academic and clinical education. This requires the Sponsoring Institution to provide “formal written policies and procedures governing resident/fellow duty hours. (IR.II.D.4.i). Scope: UAB has developed the following Duty Hour Policies applicable to every resident/fellow in all GME training programs: Definitions (from ACGME Glossary): 1. At-Home Call: Same as pager call or call taken from outside the assigned site. Time in the hospital, exclusive of travel time, counts against the 80 hour per week limit but does not restart the clock for time off between scheduled in-house duty periods. At-Home Call may not be scheduled on the resident/fellow’s one free day per week (averaged over four weeks). 2. Continuous time on duty: The period that a resident/fellow or fellow is in the hospital (or other clinical care setting) continuously, counting the resident/fellow’s (or fellow’s) regular scheduled day, time on call, and the hours a resident/fellow (or fellow) remains on duty after the end of the on-call period to transfer the care of patients and for didactic activities. 3. Duty-Hours: Duty hours are defined as all clinical and academic activities related to the program; i.e., patient care (both inpatient and outpatient), administrative duties relative to patient care, the provision for transfer of patient care, time spent in-house during call activities, and scheduled activities, such as conferences. Duty hours do not include reading and preparation time spent away from the duty site. 4. External moonlighting: Voluntary, compensated, medically-related work performed outside the institution where the resident/fellow is in training or at any of its related participating sites. 5. Fatigue management: Recognition by either a resident/fellow or supervisor of a level of resident/fellow fatigue that may adversely affect patient safety and enactment of a solution to mitigate the fatigue. 6. In-House Call: Duty hours beyond the normal workday when residents/fellows are required to be immediately available in the assigned institution. 7. Internal Moonlighting: Voluntary, compensated, medically-related work (not related with training requirements) performed within the institution in which the resident/fellow is in training or at any of its related participating sites. 8. Night Float: Rotation or educational experience designed to either eliminate in-house call or to assist other residents/fellows during the night. Residents/fellows assigned to night float are assigned on-site duty during evening/night shifts and are responsible for admitting or cross-covering patients until morning and do not have daytime assignments. Rotation must have an educational focus. 50 9. One Day Off: One (1) continuous 24-hour period free from all administrative, clinical and educational activities. 10. Scheduled duty periods: Assigned duty within the institution encompassing hours, which may be within the normal workday, beyond the normal workday, or a combination of both. 11. Strategic napping: Short sleep periods, taken as a component of fatigue management, which can mitigate the adverse effects of sleep loss. Policy: Each program must ensure that the learning objectives of the program are not compromised by excessive reliance on residents/fellows to fulfill service obligations. Didactic and clinical education must have priority in the allotment of residents/fellows' time and energies. Duty hour assignments must recognize that faculty and residents/fellows collectively have responsibility for the safety and welfare of patients. The ACGME common program requirements require the following: Fellow Duty Hours: 1. Maximum Hours of Work per Week: Duty hours must be limited to 80 hours per week, averaged over a fourweek period, inclusive of all in-house call activities and all moonlighting. a) Mandatory Time Free of Duty: fellows are provided with one day in seven free from all educational and clinical responsibilities, averaged over a four-week period. At-home call cannot be assigned on these free days. One day is defined as one continuous 24-hour period free from all clinical, educational, and administrative duties. b) Maximum Duty Period Length: (2) Duty periods of fellows may be scheduled to a maximum of 24 hours of continuous duty in the hospital. Fellows are encouraged to use alertness management strategies in the context of patient care responsibilities. Strategic napping, especially after 16 hours of continuous duty and between the hours of 10:00 p.m. and 8:00 a.m. is strongly suggested (3) It is essential for patient safety and fellow education that effective transitions in care occur. Fellow may be allowed to remain on-site in order to accomplish these tasks; however, this period of time must be no longer than an additional four hours (4) Fellows will not be assigned additional clinical responsibilities after 24 hours of continuous inhouse duty 2. Minimum Time Off Between Scheduled Duty Periods: Adequate time for rest and personal activities must be provided. (a) Intermediate-level residents/fellows should have 10 hours free of duty, and must have eight hours between scheduled duty periods. They must have at least 14 hours free of duty after 24 hours of inhouse duty. (b) The program must provide back-up support systems when patient care responsibilities are unusually difficult or prolonged, or if unexpected circumstances create fellow fatigue sufficient to jeopardize patient care. 3. Maximum Frequency of In-House Night Float: Fellows must not be scheduled for more than six consecutive nights of night float. 4. Maximum Frequency of In-House On-Call Frequency: In-house call is defined as those duty hours beyond the normal work day when the fellows are required to be immediately available in the assigned institution. The following policies apply to fellows in all programs: a) Fellows are scheduled for in-house call no more frequently than every third night, averaged over a four-week period. 51 5. At-Home Call: At-home call (pager call) is defined as call taken from outside the assigned institution. a) Time spent in the hospital by residents/fellows on at-home call must count towards the 80-hour maximum weekly hour limit. The frequency of at-home call is not subject to the every third night limitation, but must satisfy the requirement for on-day-in-seven free of duty, when averaged over four weeks. However, at home call must not be so frequent as to preclude rest or reasonable personal time for each resident/fellow. b) Fellows taking at-home call must be provided with one day in seven completely free from all educational and clinical responsibilities, averaged over a four-week period. c) Fellows are permitted to return to the hospital while on at-home call to care for new or established patients. Each episode of this type of care, while it must be included in the 80-hour weekly maximum, will not initiate a new “off-duty” period. d) The program director and the faculty will monitor the demands of at-home call in their programs and make scheduling adjustments as necessary to mitigate excessive service demands and/or fatigue. 6. Exceptions to Maximum 24 Hours of Continuous Duty in the Hospital: a) In unusual circumstances, fellows, on their own initiative, may remain beyond their scheduled period of duty to continue to provide care to a single patient. Justifications for such extensions of duty are limited to reasons of required continuity for a severely ill or unstable patient, academic importance of the events transpiring, or humanistic attention to the needs of a patient or family. Under those circumstances, the fellow must: i. appropriately hand over the care of all other patients to the team responsible for their continuing care; and, ii. document the reasons for remaining to care for the patient in question and submit that documentation in every circumstance to the program director. b) The program director will review each submission of additional service, and track both individual fellow and program-wide episodes of additional duty. 7. Exceptions to Minimum Time Off Between Scheduled Duty Periods: a) Fellows in the final year of education [as defined by the Review Committee] must be prepared to enter the unsupervised practice of medicine and care for patients over irregular or extended periods. b) This preparation must occur within the context of the 80- hour, maximum duty period length, and one day-off-in seven standards. While it is desirable that residents/fellows in their final years of education have eight hours free of duty between scheduled duty periods, there may be circumstances [as defined by the Review Committee] when these residents/fellows must stay on duty to care for their The Program Director will review the duty hours of all fellows by sampling throughout the year during representative months 1. Residents/fellows may report violations of the 80-hour rule through procedures established by calling the Designated Institutional Official, UAB Hospital; Director, Graduate Medical Education Department; the Corporate Compliance Hotline at 934-4446, or the Residents/fellows’ Hotline at 934-5025. Such calls will be investigated and reported to the DIO and Dean's Council for Graduate Medical Education. 2. The Dean's Council for Graduate Medical Education will evaluate each program's compliance and request that the Program Director describe, develop and implement a plan for corrective action for any rotations exceeding the 80 hour rule, or otherwise identified as problematic. Fellows are required to keep and maintain work hour logs on daily basis through the MedHub system. These are reviewed each week and monitored for any potential work hour concerns, including but not limited to clinical work approaching or in danger of exceeding more than 24 continuous hours of work or less than 8 contiguous hours off between clinical duty periods. If there is an obvious violation or if the coordinator has any question or concern, the Program Director will be contacted. Fellows should review, in detail, Section VI.C. of the ACGME Common Requirements that clearly outlines duty hour restrictions on a regular basis. Fellows are encouraged to directly address any concerns regarding potential work hour violations with both the Fellowship Director. The 52 Division Call schedule takes into account clinical and on-call hours and is reviewed with the Fellowship Director on a monthly basis to prevent work hour scheduling that is incongruent with duty hour guidelines. All violations that are detected through the above system of checks and balances are addressed individually and analyzed for cause and resolution within the fellowship. Violations are reviewed semiannually with each fellow and the Fellowship Director. Annual ACGME fellowship program review questionnaires are also reviewed as it relates to duty hours. Work Environment The work environment for the fellowship is designed so that all fellows have individual workspace within a singular office within the Division academic office. Private call rooms with bedding, lavatory, and shower facilities are provided and available to all fellows through coded-access 24 hours per day. If at any time, fellow is fatigued to the point where he/she (or those working with him or her) feels that it would be unsafe for the fellow to drive home, a taxi can be arranged free of charge through the GME office. All fellows are required to view the Dean’s Counsel P.P. lecture on fatigue recognition and management. All ACGME requirements (section VI.C.3.) and UAB GME requirements are applicable for this Fellowship and any breech of these should be reported. 53 XVI. Moonlighting Policy FPMRS Moonlighting Request Form To: Ed Varner, MD Fellowship Director Fellow Name: _____________________________ Date: ______________________ I wish to request to moonlight beginning _________________. The estimated average number of hours per month that I will be moonlighting is ___________, I plan to moonlight at the following location(s). 1. ______________________________________________________________________ 2. ______________________________________________________________________ I attest by initialing that I am in and will continue in full compliance with all program requirements listed below. 1. Moonlighting must not interfere with the ability of the fellow to achieve the goals and objectives of the educational program. _____ (initial) 2. Fellows participating in moonlighting activities must be fully licensed to practice medicine in the State of Alabama. _____ (initial) 3. Fellows must use their individual DEA numbers for moonlighting activities. The UAB institutional number cannot be used for moonlighting activities. _____ (initial) 4. Professional liability insurance coverage for moonlighting activities is not provided by UAB. It is the responsibility of the institution hiring the fellow to moonlight to determine whether appropriate licensure is in place, whether adequate liability coverage is provided, and whether the fellow has the appropriate training and skills to carry out assigned duties. _____ (initial) 5. Moonlight hours will be recorded each week in the fellow’s MedHub duty hours log, and counted with other work hours toward the 80 hour maximum weekly work hour limit. They will be monitored by the Program Director and Coordinator. _____ (initial) I acknowledge that moonlighting likely will not enhance my training, and that it is a privilege not a right. My moonlighting activities should in no way interfere with my fellowship training. If I do not comply with any of the above rules, in any way falsify hours or other compliance information, or if moonlighting is felt to adversely affect my performance as a fellow, I understand that the fellowship Competency Committee may choose to revoke my moonlighting privileges. _____ (initial) I also understand that the hours spent moonlighting are considered part of my fellowship duty hours and are logged and monitored as such in the MedHub system, and therefore must be in compliance with all UAB GME Policies and Procedures. _____ (initial) I am aware that the UAB malpractice insurance, DEA registration and my Alabama License do not cover me while moonlighting. _____ (initial) ___________________________________ Fellow’s Signature & Date ___________________________________ PD Signature & Date 54 The above request form may be obtained from the program coordinator. 1. Applications to moonlight will be reviewed and approved by the DIO. 2. Audits of moonlighting duty hours logged will be performed by the GME office and trainee’s Program Director. The moonlighting policy needs to be reviewed every year at the time of the Annual Program Evaluation. A copy of the moonlighting policy will be available to the GME office as an attachment to the Annual Program Evaluation document. 3. Applications are valid for a twelve month period or the end of the academic period whichever comes first; at such time a re-application may be submitted for consideration. 55 XVII. Vacations, Sick, and Maternity Leave In conjunction with the Graduate Medical Education Policy on Paid Leave Benefits (www.umm.edu/gme/doc/GMS-NPaid_Leave_Benefits.doc), the fellowship program has established the following vacation/leave policies. All leave requests must be submitted through the MedHub system. Once the request for vacation/time off is submitted it will be reviewed and approved in MebHub. If there is a conflict or concern regarding the request, it will be discussed with the fellow individually. Vacation and time off should be planned 6 months in advance. ALL requests should be submitted by the end of July and the beginning of January. Fellows should work out coverage for his or her clinical responsibilities before such a request is made. Request should also be submitted whenever the fellow will be unavailable for clinical duties, including (but not limited to) vacation, interviews, medical appointments, scientific presentations, etc. Vacation FPMRS Fellows are allowed 15 calendar days of vacation each year per the contract with the medical center. When call schedules are being developed, attempts will be made to include the weekends before and after the vacation week. This is not guaranteed. Certain times of the year are more challenging for education, patient care, and scheduling. Therefore, vacation/special requests should not be requested during July and preferably not during the core rotations (Urogyn and Urology) during the first 3 months of fellowship. In general, vacations should be scheduled for one week at a time. Two-week vacations may possibly be permitted if the weeks ‘straddle’ two rotations. Vacations cannot be scheduled for two weeks during one rotation unless it is a research rotation and in the case request should be made approximately 1 year in advance. A holiday work schedule will be developed for the Christmas (12/24, 25 ) and New Year (12 31, 1/1) holidays, Thanksgiving Day , July 4th,MLK Day and Labor Day at a meeting in July- chaired by the Senior Fellow. Vacations are explicitly discouraged during the first week of any rotation. Conflicting dates will be awarded based on date of request and seniority. Vacations taken without an approved request will be taken without pay and may result in disciplinary action and may be considered as absence from duty days (see last paragraph). Unused vacation time Vacation time exists to be used and not “banked”, but rarely all allotted vacation time cannot be used during a given year. In that event, the resident may submit a written vacation carry over request for approval by the program director. Vacation carry over may not exceed half of the annual allotment, and must be used up by March 1 There is no reimbursement for unused vacation time. Job interviews Up to five week days off. Efforts should be made to schedule job interviews on days that minimize disruption of clinical responsibilities and patient care. Potential employers understand the importance of clinical responsibilities and patient care; it is perfectly acceptable to negotiate an interview date. You are expected to coordinate with the other fellows. More than five days away from the fellowship for interviews and other career development must be taken from the allotted vacation time or taken without pay. The appropriate vacation request form must be completed. 56 Sick/medical leave If a fellow is sick and cannot come to work, Fellow must call the senior fellow or, if the illness develops during the 8 to 5 hours on week days the program coordinator, Julie Burge at 934-2569. These calls should be made as early as possible. Extended medical leave will be handled on a case-by-case basis in accordance with medical center policies. The Fellowship Coordinator will help you process the necessary paperwork. Emergency leave In the event of an absence resulting from sudden illness or death in the immediate family, the fellow will complete the Leave Request form on the day s/he returns to work. Notification policies as listed in Sick/medical leave section (see above) also apply. Bereavement Leave In the event of the death of a spouse, first degree relative, or member of the resident’s household, time off is granted without loss of pay for three working days. Additional time off without pay may be requested. Family Medical Leave Act (FMLA) FMLA is available for specified family and medical reasons. This includes but is not limited to maternity leave, paternity leave, and extended medical leave. The program will grant unpaid family leave (childbirth, adoption, serious health condition of a spouse, parent or child) in compliance with all state and federal laws. Paid leave after childbirth shall be four weeks, using 3 weeks of your annual sick leave and one week of your annual vacation. A fellow can take up to 6 weeks of leave with pay using all sick and vacation time, assuming that no leave has been taken during that current academic year and with prior approval from the Fellowship Director. For specifics on this policy, refer to the FMLA Fact Sheet found on the hospital intranet at http://intra.umm.edu/ummc/employee/benefits/documents/FMLAFactSheet.doc The Fellowship Coordinator will help you process the necessary paperwork. Military Obligation Leave will be granted for military or reserve obligations. Military obligations must be scheduled well in advance of the dates of the obligations. Jury Duty Paid leave will be granted for jury duty. However, jury duty is considered an absence from the educational program in the eyes of the ABOG and may have to be made up. The program director will therefore be happy to furnish a letter requesting that the fellow be excused from jury duty; however this request is not always granted by the court. Conferences Whenever possible, the department will support a resident attending a conference to present first-author research. These requests must be submitted at least three months prior to the planned conference. Time away beyond that necessary for presentation of the research may not be able to be granted (i.e., attendance for the full length of the meeting may not be possible, however effort will be made to provide it and can generally be worked out). Each urogyn fellow receives $416.66 a month, (prior to taxes), ($5000 Total) in his/her pay check for reimbursement. For further approval of travel reimbursements, an accounting of your personal expenditures should be submitted following each trip. Once this has been met, the division may reimburse monies above and beyond the $5,000 only with Dr. Richter's approval. It is taxed income and will be accounted for in approving future expenditures. Your personal expenditures are business related expenditures such as books, journals, meals, travel to meetings, etc. 57 Overall Absence from the Program: Please note that ABOG’s requirements of Fellowship Programs include the following: The Residency Review Committee in Obstetrics and Gynecology (RRC) under the direction of the Accreditation Council for Graduate Medical Education (ACGME) requires that absences of more than eight weeks in any of the first three years of training, more than six weeks in the senior resident year, or absences totaling more than 20 weeks require an extension of the training period by the amount of time in excess of the above listed limits. The additional training must be completed by September 1 to receive permission to take the written examination of The American Board of Obstetrics and Gynecology (ABOG) in June of the following year. Absences include vacations, sick leave, jury duty, and maternity or paternity leave. Attendance at scientific meetings or postgraduate courses approved by the Program Director is not considered an absence in this context. 58 XVIII. Case List Each fellow will be added to the ACGME case log site specific to our program at the beginning of the fellowship. Fellows are responsible for logging all of their cases into the system. This will be monitored on a regular basis by the Program Coordinator and Director and, formally, at the time of each semiannual competency meeting with the Program Director (and Competency Committee if deemed unacceptable). Case Logs for Boards 1. A Case Log form must also be completed as part of the Board Exam application process. The form must be completed and submitted on line. 2. The deadline for submission of all application materials, including the case log will be set by the boards and may be found under the FPMRS subsection of ABOG.org or ABU.org. 59 XIX. Fellow Evaluations for Feedback and Advancement Semi Annual Fellow Evaluation: Each fellow will meet formally with the fellowship director and if indicated other members of the competency committee semi-annually in early January and May of each year. That meeting will include the following listed below. A review of all competency evaluations of the fellow by faculty, residents, nurses, other medical staff, medical students, and patients. A review of Rotation Evaluations and Focused Assessments Review of Milestone Conference Evaluations A review of the fellow’s academic portfolio which include a record of his/her self-learning, UAB presentations, National Presentations, duty hours, case logs, and his/her Curriculum Vitae.(Section VIII) A review of the fellow’s progress in research which will include the thesis project as well as other projects. Adherence to time tables established will be expected. Other professional achievements will be reviewed as well. Self-Assessment review will include a review of the fellow’s present and previous self-assessments, goals and how well the goals have been met. One to three new goals will be determined for the upcoming six months. The fellow will then be given his/her overall assessment by the program director and if there are any inadequacies, these will be reviewed by the competency committee, with consultation from others if need be, to determine if further action will be required. Evaluative Tools (See MedHub) Rotation Evaluations: upon completion of Urogynecology, Urology, Geriatric, Research, or Colorectal rotations the faculty for that rotation will complete the specific rotation evaluation form, which will be submitted electronically to the fellowship coordinator. The individual faculty members may also give the fellow his/her perception of the fellow’s progress. If upon review of the evaluation by the coordinator there is a reason for immediate review by the fellowship director and competency committee that will be instituted with immediate action taken with the fellow when felt indicated. It is expected that educational and competency goals will be met as outlined and on each evaluation sheet. The faculty assessment of the fellows’ knowledge during each rotation should be obtained by informal questioning of the fellow or by observation of a fellow who is performing teaching activities. The faculty member and fellow will adjust the evaluations based on the time lines given for each learning assignment. Additionally the faculty may prefer to perform an informal oral examination of the fellow. These rotation evaluations are also reviewed with the fellow by the Fellowship Director at the semiannual evaluations. Focused Assessments of Specific Clinical Activities include clinical evaluations, (POP-Q, Urodynamics, and Anal/Rectal Studies), as well as, evaluations of specific surgical procedures listed. These will be performed by designated faculty members (or nurse practitioner for POPQ and urodynamic evaluations). It will be the responsibility of the fellow to notify the program coordinator when these assessments need to be sent through the MedHub system. The evaluation for Robotic Surgery will be submitted a similar manner. Milestone Conference Evaluations: Interactive conferences based on the Medical Knowledge and Patient Care Milestones will be directed by faculty members for the fellows together. Various questions will be given to each fellow at the three levels to better assess performance on these competences. There Communication skills will also be assessed. There will be a conference on each of the topics each year and evaluations of each fellow will be performed and discussed with her/him. 60 Presentation Assessments: These will be completed by faculty, residents and other fellows following observed presentations (conferences, national meetings, or other) and handed to the fellowship director or faxed to the fellowship Coordinator, Julie Burge as soon as possible following the presentation. These will be used to further assess all of the clinical competencies and for instruction of fellows on teaching techniques. Fellowship Global Competency Evaluations: Faculty and residents will submit these electronically every six months. Other health care workers, divisional nursing staff, medical students, and patients will submit their evaluations periodically as directed by the clinic or operating room nurses. All will be reviewed at least semiannually and Competency Goals will be created with the Program Director. Formal Oral Exam: This will be given toward the end third year to Urogynecology fellows and the end of the second year to urology fellows. The exam will be developed and administrated by the Competency Committee. If a fellow’s performance is unsatisfactory, he/she will be personally counseled with the need for specified learning activities prior to completion of his/her fellowship. 61 XX. Responsibilities of the Fellowship Faculty To know educational and clinical (competency based) goals and objectives of the fellowship related to your individual expertise. To instruct of the fellow in clinical and surgical patient care, related to these objectives and evaluate their progress during all activities. To perform Rotation evaluations after each rotation for the fellow on that rotation. To participate in selected Milestone Conferences as well as other conferences in order to instruct and evaluate fellows and for self review of sujects To perform a Global Competency Evaluation semi-annually on each fellow who rotated on your service. To provide both positive and negative feedback to the fellows as necessary. To perform focused assessments on specified surgical procedures performed by the fellow To perform assessments of oral presentations or teachings sessions performed or conducted by the fellow Periodically, on a rotational basis, participate in the development of and administration of an oral exam to one or two fellows To perform or participate in “Scholarly Activity” to advance yourself as an academician and teacher XIX. Responsibilities of the Fellow in Female Pelvic Medicine and Reconstructive Surgery are: To adhere to all policies and meet all requirements outlined in the above sections and, in doing so, well demonstrate the six clinical competencies which include the following: 1. Medical Knowledge – By demonstrating thorough evidence based understanding of the FPMRS Specialty topics. 2. Professionalism – To demonstrate professionalism in patient care, in relationships with other health care workers, and in recordkeeping and fulfillment of all the requirements of the fellowship. 3. Patient Care – To demonstrate application of medical knowledge in the evaluation and management of patients in this subspecialty. This will include the development of all the other competencies. 4. Interpersonal and Communication Skills – There should be demonstrated during interactions not only with patients but with all others who the fellow is associated. 5. Problem-Based Learning and Improvement – The fellow will demonstrate the ability to recognize shortcomings of various aspects of his/her practice, learn how to define a problem, develop an evaluation of how the problem may be solved and progress in to resolution of the problems by various means including designed comparison studies. 6. System-Based Practice – Fellow will be expected to coordinate all aspects of patient care and, in doing so; will communicate with others in the system as a whole to facilitate the optimal management of an individual patient and of his/her practice as a whole. 62