Week 12_Lecture_Notes_Urinary System - TAFE-Cert-3
advertisement
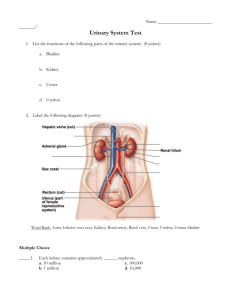
HLTAP301A ANATOMY & PHYSIOLOGY LECTURE 12 - THE URINARY SYSTEM Metabolism of nutrients by body cells produces waste products such as carbon dioxide and nitrogenous wastes (such as creatinine, urea and ammonia). These metabolic wastes must be eliminated from the body, while retaining essential substances to maintain homeostasis. While several organ systems are involved in the excretory process, the urinary system bears the primary responsibility for removing nitrogenous wastes from the blood. The kidneys filter blood and return most of the water and many solutes to the bloodstream. The remaining water and solutes constitute urine. Urine is excreted from each kidney through it’s ureter and stored in the urinary bladder until it is expelled through the urethra. In addition to the pure excretory function of the kidneys, they also maintain the electrolyte, acid-base and other fluid balances in the blood. Malfunction of the kidneys leads to an imbalance in homeostasis, which unless corrected, will result in death. The structure of the urinary system includes two kidneys, two ureters, one urinary bladder and one urethra. Let’s look at these structures in more detail: The Kidneys The paired kidneys are kidney-bean shaped organs located just above the waist between the peritoneum and the posterior wall of the abdomen. The kidneys are located between the levels of the last thoracic and third lumbar vertebrae, and the right kidney is slightly lower than the left, because of the location of the liver. An adult kidney is about 12cm long, 6cm wide and 3 cm thick, about the size of a large bar of soap. Each kidney is enclosed by a fibrous, transparent renal capsule and in a living person, a capsule of fatty tissue surrounds each kidney, protecting them from external damage. In the event of a rapid weight loss, the kidneys may drop to a lower position which can cause the ureters to become kinked, which in turn causes urine to back up and exert pressure on the tissue of the kidneys, a condition known as hydronephrosis, which can severely damage the kidney. The Nephron A nephron is both the structural and functional unit of the kidney and may sometimes be referred to as the kidney tubules. Nephrons do three things – they filter blood, return useful substances to the blood and remove substances from the blood that are not needed by the body. Nephrons maintain the homeostasis of the blood and urine is produced. There are about one million of these microscopic structures and each nephron consists of two main parts – a glomerulus (a knot of capillaries that perform the filtration process) and a renal tubule. The closed end of the renal tubule is a cup-shaped structure that completely surrounds the glomerulus. This part of the renal tubule is known as Bowman’s capsule. 8/2/16 1 of 4 LECTURE 12 HLTAP301A ANATOMY & PHYSIOLOGY As the renal tubule extends from the Bowman’s capsule, it twists into three distinct regions – the proximal convoluted tubule (PCT), the Loop of Henle and the distal convoluted tubule (DCT). The collecting ducts in the nephron runs from the DCT downwards into the renal pyramids, delivering urine, which will eventually move into the ureters. The Ureters, the Bladder and the Urethra The ureters are passageways that carry urine from the kidneys to the bladder and are approximaely 25-30 cm long. The urinary bladder is a hollow, muscular organ situated in the pelvic cavity posterior to the pubic symphasis and is the storage area for urine. In males, it is directly anterior to the rectum, in females it is anterior to the vagina and inferior to the uterus. It is held in place by folds of the peritoneum. The bladder changes shape depending on the amount of urine contained within. When the bladder is empty, it is collapsed; when it is slightly distended it becomes spherical and when it is fuller, it becomes pear-shaped. Although urine is formed continuously by the kidneys, it is usually stored in the bladder until its release is convenient. The bladder capacity averages 700-800ml. It is smaller in females because the uterus occupies the space just superior to the bladder. The urethra is a small tube leading from the internal urethral orifice in the floor of the urinary bladder to the exterior of the body and it carries urine by peristalsis from the bladder to the outside of the body. In both males and females the urethra is the terminal portion of the urinary system. In females the urethra is located between the clitoris and the vaginal opening. In males, the urethra passes through the prostate gland, through the urogenital diaphragm and finally through the penis. The internal urethral sphincter (involuntary) keeps the urethra closed when urine is not being passed. The external urethral sphincter is controlled voluntarily. The length and function of the urethra differs in the two sexes. In females, it is about 3-4cm long and its only function is to conduct urine to the body exterior. In males it is about 20cm long and not only carries urine out of the body but also provides the passageway through which sperm is ejected from the body. Thus, in males, the urethra is part of both the urinary and reproductive systems. Urine Formation For urine to be formed in the nephron three processes must take place – filtration, reabsorption and secretion. Filtration is performed by the capillary beds of the glomerulus – they have extremely high blood pressure which forces fluid and solutes (smaller than proteins) out of the blood into the glomerular capsule. The filtrate that is formed is basically blood plasma without blood proteins. 8/2/16 2 of 4 LECTURE 12 HLTAP301A ANATOMY & PHYSIOLOGY When systemic blood pressure is normal, filtration will continue to occur. If arterial blood pressure drops too low, the glomerular blood pressure drops and substances can no longer be forced out of the blood, thereby stopping filtrate formation. Tubular Reabsorption takes place in the renal tubules, commencing as soon as the filtrate enters the proximal convoluted tubule. The filtrate contains many useful substances that the body can still use – these include water, glucose, amino acids and ions. These need to be reclaimed from the filtrate and returned to the blood. The capillary beds are low pressure, porous vessels that are specially adapted for absorption. Some of the substances, such as water, reenter the capillaries passively via osmosis. Others require active transport processes, and the body is very selective about what is allowed to pass through. For example, glucose and amino acids are usually always completely removed from the filtrate, but nitrogenous wastes such as urea are hardly reabsorbed at all. Most absorption takes place in the proximal convoluted tubule, however the Loop of Henle, the distal convoluted tubule and collection ducts can reabsorb substances as well. Secretion is reabsorption in reverse. For example, substances that the body doesn’t need, (such as urea, uric acid and creatinine) are excreted from the peritubular capillaries and into the renal tubules and become part of the filtrate, which then becomes urine. Ions such as hydrogen and potassium also move into the filtrate, and this plays an important role in maintaining blood pH. Solutes normally found in urine are sodium, potassium, urea, uric acid, creatinine, ammonia, bicarbonate ions and various other ions depending on blood composition. Substances not normally found in urine are glucose, blood proteins, red blood cells, haemoglobin, white blood cells and bile. Homeostatic Imbalances Uremia is a condition resulting from advanced stages of kidney failure in which urea and other nitrogen-containing wastes are found in the blood. Uremia can be caused by NSAIDs (nonsteroid anti-inflammatory drugs), especially in older patients treated primarily with ibuprofen for arthritis. Some of the early signs of uremia are lethargy, mental depression, loss of appetite, and edema; later symptoms include diarrhea, anemia, convulsions and even coma. Incontinence occurs when we are unable to voluntarily control of external sphincter. It is common in children under 2 and in women during pregnancy. It can also be caused by emotional problems and degradation of the pelvic floor muscles. Urinary retention is the opposite of incontinence – where the bladder is unable to expel its contained urine. It can occur after a general anesthetic because it takes a little time for the smooth muscles to regain their activity. It can also be caused by an enlarged prostate gland. 8/2/16 3 of 4 LECTURE 12 HLTAP301A ANATOMY & PHYSIOLOGY Maintaining Water Balance The human body is mostly liquid and our total body water is a function of age, body mass, and body fat. Due to their low body fat and bone mass, infants are about 73% water, whereas the body water content of men is about 60%. Because women have relatively more body fat and less skeletal muscle than men their water content is about 50%. Body water declines throughout life, ultimately comprising about 45% of total body mass in old age. The kidneys maintain chemical balance throughout the body by producing and eliminating urine – they regulate the volume, electrolyte concentration and acid-base balance of body fluids. The skin and lungs also play a role in fluid and electrolyte balance through the process of perspiration and respiration. In addition the blood contains buffers which regulate bicarbonate ions. Fluid imbalance occurs when regulatory mechanisms can’t compensate for an abnormal intake and output at any level from the cell to the organism as a whole. Fluid and electrolyte imbalances include oedema, isotonic, hypertonic or hypotonic alterations, and electrolyte imbalances. Disorders of fluid volume or osmolarity (concentration of electrolytes in the fluid) result. Increased fluid volume in the interstitial spaces is called oedema. Oedema may be classified as localised or systemic. Obstruction of the veins or lymphatic system or increased vascular permeability usually causes localised oedema in the affected area (eg. Swelling around an injury). Systemic or generalised oedema may be due to cardiac failure or renal disease. For the body to remain properly hydrated, water intake must equal water output. Most water enters the body through ingested liquids and food, but is also produced by cellular metabolism. Water output is due to evaporative loss from lungs and skin (insensible water loss), sweating, defecation, and urination. The thirst mechanism is triggered by a decrease in plasma osmolarity, which results in a dry mouth and excites the hypothalamic thirst center. Thirst is quenched as the mucosa of the mouth is moistened, and continues with distention of the stomach and intestines, resulting in inhibition of the hypothalamic thirst center. The amount of water reabsorbed in the renal collecting ducts is proportional to Anti Diuretic Hormone (ADH) release. When ADH levels are low, most water in the collecting ducts is not reabsorbed, resulting in large quantities of dilute urine. When ADH levels are high, filtered water is reabsorbed, resulting in a lower volume of concentrated urine. ADH secretion is promoted or inhibited by the hypothalamus in response to changes in solute concentration of extracellular fluid, large changes in blood volume or pressure, or vascular baroreceptors. 8/2/16 4 of 4 LECTURE 12