Cecil ch 29 [4-20
advertisement

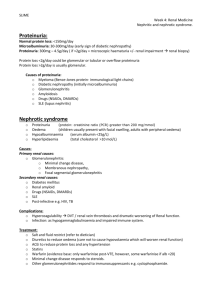
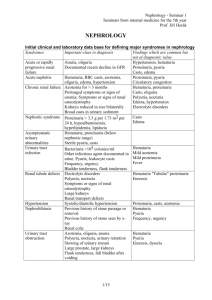
Cecil’s Chapter 29: Glomerular Diseases Each kidney has nearly 1 million glomerular capillary tufts deriving from the afferent arterioles, and are held together by the mesangial matrix - They then drain into the efferent arteriole Fenestrated endothelial cells, the GBM, and foot processes from epithelail podocytes, all form a selective filtration barrier between the capillary blood and urinary space Each glomerular tuft has an associated renal tubule that drains into the urinary system Nearly ¼ of the blood of each heartbeat is filtered by the kidney A tremendous amount of protein is filtered each day, but hardly any appears in the urine - This is because the negatively charged GBM and slit-pore membranes restrict movement of large or negatively charged proteins, so it’s a size and charge barrier Symptoms of glomerular disease – hematuria, proteinuria, pyuria, hypertension, fluid retention, edema, and decreased GFR Acute nephritic syndrome is characterized by hypertension, hematuria, edema, RBC casts or dysmorphoic RBCs, modest proteinuria (1-2 g / 24 hours), and decreased GFR - Decreased GFR is seen as a rise in serum creatinine If the loss of GFR happens over days, acute nephritis is called rapidly progressive glomerulonephritis (RPGN), and will show cresentic glomerulonephritis on renal biopsy When people with RPGN have the disease extend to the lungs, it’s called pulmonary-renal syndrome In nehprotic syndrome, they excrete more than 3.5 g of protein / 24 hours, and show edema, hypoalbuminemia, and hypercholesterolemia - Long-standing nephrotic syndrome can cause decreased GFR and hypertension (ex: diabetic nephropathy) Nephrotic syndrome in a child suggests minimal change nephropathy o Shows that onset and timing can help distinguish between glomerular diseases Measuring 24 hour creatinine clearance and proteinuria helps distinguish whether there’s nephrotic syndrome or not, and assesses GFR Renal vasculature problems show hematuria and mild proteinuria Renal biopsy tells you if the disease is focal (involves less than half the glomeruli) or diffuse (involves more than half the glomeruli), or segmental (involving a part of a glomerulus) or global (involving the whole glomerulus) - Can also show crescents, which is the hallmark of rapidly progressive glomerulonephritis Immunofluorescence microscopy can ID types of Ig deposition and location Page 324 Treatments for glomerular diseases: - Hypertension – get it down to 130/80 Inhibit renin-angiotensin Volume overload from edema – treat by reducing salt and water intake, and use diuretics At all costs avoid exposure to nephrotoxins to avoid the risk for acute kidney injury Acute nephritic syndromes: - - Poststrep glomerulonephritis – happens after infection by nephritogenic M type of strep in the throat or skin o Glomerulonephritis from strep happens in less than 5% of throat infections, usually 1-3 weeks after the pharyngitis o Glomerulonephritis from strep impetigo is less common, but up to half of people with strep impetigo develop glomerulonephritis 2-6 weeks after the impetigo o In developed countries like the US, strep glomerulonephritis happens sporadically in the summer and fall o It can happen in adults, but is most common in kids 2-14 years old o Classic symptoms of poststrep glomerulonephritis are acute nephritis characterized by hematuria, pyuria, RBC casts, edema, hypertension, system stuff like headache and malaise, flank pain from renal capsule swelling, and oliguric renal failure Since the hematuria happens after the pharyngitis, it’s called metapharyngitic or postpharyngitic hematuria 5% of kids, and 1/5 of adults will have proteinuria in the nephrotic range Early in the disease, most patients will have decreased levels of C3 complement and CH50, with normal C4 Will see increased ASO antibodies, anti-DNAase, or antihyaluronidase antibodies The kidney will show diffuse proliferative glomerulonephritis with hypercellularity of the mesangial and endothelial cells, WBC infiltrate into the glomeruli, and granular “lumpy-bumpy” subendothelial and subepithelial deposits of IgG, IgM, and complement o Antibiotics and immunosuppressives don’t help PSGN o 90-95% of patients will completely recover Kids recover within 3-6 weeks of onset of nephritis, while adults can have symptoms like proteinuria and hematuria for 1-2 years o End-stage renal disease is uncommon in PSGN Subacute bacterial endocarditis – shows hematuria, pyuria, and mild proteinuria, and rarely it can go to rapidly progressive glomerulonephritis (RPGN) o - Labs show an increased erythrocyte sedimentation rate (ESR), low complement, positive rheumatoid factor, cryoglobulinemia, and anemia o Renal biopsy shows focal proliferative glomerulonephritis with lots of deposits of IgG, IgM, and complement Those with RPGN have crescents o Good prognosis and you treat for antibiotics for 4-6 weeks Lupus nephritis: o 60% of adults and 80% of kids with systemic lupus erythematosus (SLE) get renal problems o Symptoms are hematuria, proteinuria, RBC casts, hypertension, low complement,a nd anti-double-stranded DNA (anti-dsDNA) antibodies o Page 326 – classes of lupus nephritis WHO class 1 lupus lesions – show hematuria with normal histo Prognosis is excellent, and no treatment is needed WHO class 2 nephritis – shows mesangial immune complex deposition with mesangial proliferation, but few clinical renal manifestations, normal kidney function, and good prognosis Treatment is not necessary WHO class 3 lupus nephritis – shows focal lesions with proliferation and scarring, called focal proliferative lupus nephritis Symptoms include hypertension, hematuria, proteinuria, nephrotic syndrome in up to 1/3 of them, and increased serum creatinine Those with just mild focal proliferation that doesn’t involve much of the glomeruli have a good prognosis Those with more severe and diffuse proliferation have a worse prognosis, and need steroids or other immunosuppressive drugs WHO class 4 lupus nephritis – shows global, diffuse proliferative lesions that involves most of the glomeruli, called diffuse proliferative lupus nephritis Has more severe symptoms, including RPGN, hematuria, RBC casts, hypertension, proteinuria (half in nephrotic range), and decreasing renal function Needs steroids and immunosuppressives Prognosis is good if you can get the symptoms to remit WHO class 5 lupus nephritis – also shows proliferative lesions, and nephrotic syndrome, along with hypertension, renal dysfunction, and renal vein thrombosis Steroids and immunosuppressives help WHO class 6 lupus nephritis – show 90% scarred or sclerotic glomeruli, which implies end-stage renal disease (ESRD) About 1/5 of patients with lupus nephritis reach ESRD - - - Antiglomerular basement membrane disease – they have autoantibodies directed against the α3 NC1 domain of type 4 collagen in the GBM o Presents as isolated glomerulonephritis (anti-GBM disease) or involve type 4 collagen in the lung, causing a pulmonary-renal syndrome, called Goodpasture syndrome o Anti-GBM disease happens most often either in young men in their 20’s, or men and women in their 60’s-70’s o Anti-GBM disease can be triggered by exposure to infection, smoking, or solvents o Symptoms include hemoptysis, anemia, fever, dyspnea, hematuria, and RPGN About 1/10 of people with RPGN have anti-GBM disease o Renal biopsy shows a characteristic linear pattern of staining of the capillary loops with IgG and C3 Antinuclear cytoplasmic antibody (ANCA)-associated small vessel vasculitis o ANCA’s are found in the serum of most people with pauci-immune glomerulonephritis o ANCAs cause small vessel endothelial cell injury in Wegener grnaulomatosis, polyangiitis, and Churg-Strauss syndrome o 2 types of ANCA antibodies: Anti-proteinase 3 (anti-PR3) – more often found in the cytoplasm, and more common in Wegener granulomatosis Anti-myeloperoxidase (anti-MPO) – usually found around the nucleus (perinuclear), and more common in polyangiitis or Churg-Strauss syndrome o Wegener granulomatosis – shows fever, rhinorrhea, nasal ulcers, sinus symptoms, hemoptysis, arthritis, hematuria, and mild proteinuria It can present as a limited disease that involves both the lungs and kidneys, asymptomatic microscopic hematuria, or RPGN o Microscopic polyangiitis – shows same symptoms as Wegener’s, but lung symptoms are rare o Churg-Strauss syndrome – shows eosinophilia, purpura, mononeuritis multiplex, and respiratory stuff like asthma or allergic rhinitis o Renal biopsy of ANCA diseases shows pauci-immune glomerulonephritis, with only a few immune complexes int eh small vessels and either a crescentic glomerulonephritis, or focal necrotizing glomerulonephritis Cryoglobulinemia – shows purpura, fever, Raynaud phemonena, arthralgia, fatigue, and kidney involvement in half of cases o Raynaud’s phenomenon - cold temperatures or strong emotions cause blood vessel spasms, blocking blood flow to the fingers, toes, ears, and nose. o Seen in middle age, more often in women o Kidney symptoms include mild isolated hematuria or proteinuria, or severe symptoms with acute nephritic syndrome and RPGN o Can see positive rheumatoid factor and low C4 o Up to half of people with cryoglobulinemia have HCV o Renal biopsy shows membranoproliferative pattern of injury with hyaline thrombi o Often, treating the HCV infection will fix the cryoglobulinemia Nephrotic syndromes: - - - Nephrotic syndromes carry a risk for thrombotic conditions – since you lose clotting factors Minimal change disease (MCD) – most common cause of nephrotic syndrome in kids o 70-90% of cases of nephrotic syndrome in kids are from minimal-change disease 10-15% of cases in adults are from MCD o Minimal change disease is usually idiopathic, but can sometimes be associated with Hodgkin disease or NSAIDs o Minmal change disease presents with abrupt onset of proteinuria in the nephrotic range and edema In kids the proteinuria is mainly albumin, so it’s called selective proteinuria o Renal biopsy is the only definitive diagnostic test for MCD, but only done if they don’t respond to NSAID therapy Shows normal light microscopy, negative immunofluorescence, and effacement of foot processes o Up to 1/3 of kids will spontaneously get better, but you still treat them with steroids o 90-95% of kids will completely recover, and most adults do too, but it takes longer o Relapses are common, and frequent relapsers are those with 2 or more in 6 months Focal segmental glomerulosclerosis (FSGS) – page 328 o FSGS is up to 15% of nephrotic syndrome in kids, up to 1/3 in adults o More common in blacks, where it’s up to half of cases of nephrotic syndrome o Can either be primary and idiopathic, or secondary to a familial or systemic process o Symptoms of FSGS are proteinuria, microscopic hematuria, hypertension, edema, and impaired kidney function Adults with FSGS are more likely to develop hematuria, hypertension, and impaired renal function than with minimal change disease o Renal biopsy changes are most prominent in glomeruli near the corticomedullary junction, and include focal and segmental scarring o Heroin users, people with HIV, and blacks, can get a collapsing glomerulopathy with segmental or global glomerular collapse, massive proteinuria, and rapidly advancing renal failure o Recovery both with treatment or without is more rare in FSGS than in minimal change disease o Treat with inhibitors of renin-angiotensin and steroids o People with FSGS who are at high risk for progressive loss of renal function include those with nephrotic proteinuria, blacks, males, and those with renal insufficiency Membranous glomerulonephritis (MGN) – most common cause of nephrotic syndrome in elderly people o Most cases of MGN are idiopathic, but up to a 1/3 happen from cancers, infection, or rheumatologic disease o Most show nephrotic syndrome with nonselective proteinuria, and half have microscopic hematuria o - MGN carries the highest risk of nephrotic syndromes for renal vein thrombosis, pulmonary embolism, and deep vein thrombosis o Membranous glomerulonephritis is diagnosed by renal biopsy that shows uniform thickening and “spike” formation in the basement membrane along the capillary loops, and deposits of IgG and C3 (page 328) Diabetic nephropathy – most common cause of chronic kidney disease in the US o 45% of people with ESRD have diabetic nephropathy o About 40% of people with diabetes have diabetic nephropathy o Blacks, native americans, and SE Asian americans with type 2 diabetes are more likely to develop diabetic nephropathy than whites o In patients newly diagnosed with diabetes, you see renal hypertrophy and glomerular hyperfiltration o Within 1-3 years, you see glomerular basement thickening, mesangial expansion, hyaline arteriosclerosis, and sometimes nodular gloemruosclerosis o When it gets to diabetic nephropathy, the earliest sign is an increase in excretion of albumin in the urine Microalbuminuria – losing 30-300 mg of albumin / 24 hours Overt nephropathy or proteinuria – losing more than 300 mg of albumin / 24 hrs o Start testing people with type 1 diabetes after 5 years, for microalbuminuria o Test people with type 2 diabetes at diagnosis and then yearly after for microalbuminuria o Once microalbuminuria progresses to proteinuria, kidney function declines, with half reaching ESRD by 10 years o Many patients with microalbuminuria or proteinuria and type 2 diabetes die from cardiovascular events before they reach ESRD o Almost all of patients with type 1 diabetes and diabetic nephropathy also have diabetic retinopathy As opposed to type 2, which is about 2/3 o Unlike other glomerular diseases, patients with diabetic nephropathy often have normal sized to enlarged kidneys Glomerular diseases showing mainly hematuria: - IgA nephropathy o One of the most common causes of glomerulonephritis in the world o IgA nephropathy is more common in Asia and S. Europe, than in north America o IgA nephropathy peaks in yours 20’s-30’s, and prefers males o Classic IgA nephropathy shows recurrent episodes of hematuria during or immediately after an upper respiratory infection, called synpharngitic hematuria Proteinuria can happen late in the disease o Rarely, IgA nephropathy can present as RPGN o In most patients, IgA nephropathy is a benign disease, with only up to 1/3 progressing to ESRD over 20 years - - - Risk factors for progression include hypertension, absence of visible hematuria, proteinuria, and being male o Diagnosis requires a renal biopsy that shows characteristic IgA stains in the mesangium o Inhibiting renin-angiotensin can slow progression of many glomerular diseases associated with proteinuria, including IgA nephropathy Henoch-Schonlein purpura – very similar to IgA nephropathy, and only differs in that it affects kids more, and causes arthralgia and abdominal problems, and purpura on the hands Membranoproliferative glomerulonephritis (MPGN) – group of glomerular diseases o Can be idiopathic or secondary to something systemic o MPGN is rare in blacks o Idiopathic disease usually presents in childhood o MPGN is associated with HBV, HCV, cryoglobulinemia, SLE, sickle cell, antiphosphollipid antibody syndrome, and some cancers o MPGN is divided into types 1, 2, and 3 MPGN type 2 (dense-deposit disease) – usually have C3 nephritic factors, which are antibodies that stabilize the C3 convertase, & allow it to activate serum C3 Alos causes parital lipodystrophy and factor H deficiency MPGN type 3 causes complement receptor problems o MPGN shows hematuria, proteinuria, pyuria, low C3, and type 1 shows fatigue and malaise, and nephrotic proteinuria o Renal biopsy findings include capillary loop thickening with basement membrane duplication and mesangial hpyercellularity, often with lobular segmentation Type 1 MPGN causes mesangial interposition between the capillary basement membrane and endothelial cells to form a double contour “tram-tracking” appearance o Half of people with MPGN develop ESRD within 10 years, and 90% by 20 years Thin basement membrane disease (TBMD, aka benign familial hematuria) o Affects 1% of the population o Half of TBMD is autosomal dominant, and up to half have mutations to the COL4A3 or A4 gene, causing slight decreases in α3 α4α5 type 4 collagen in the GBM Unlike Alport syndrome, which causes the whole type 4 collagen to be lost or severely distorted o Patients show microscopic hematuria, with no proteinuria o Unlike Alport syndrome, thin basement membrane disease is benign Alport syndrome (aka hereditary nephritis) – name for a bunch of mutations to collagen 4 that cause hematuria, deafness, and sometimes eye problems o Most have an X-linked mutation to COL4A5, causing decreased or distorted α3 α4α5 type 4 collagen or α5 α5α6 type 4 collagen in the GBM o Symptoms include microscopic hematuria, mild proteinuria, and sensorineural deafness Some develop lens problems Rarely mental retardation and leiomyamatosis (small papule like growths) are seen o o Alport syndrome affects males more than females, and more often progresses to glomerulosclerosis and ESRD in men In the juvenile x linked one, they get alport syndrome before age 30 Glomerular deposition diseases: - - - In people with systemic amyloidosis, about 2/3 have AL amyloid with deposits of Ig light chains o The other 1/3 have AA amyloid, called secondary amyloidosis Serum amyloid A, an acute phase reactant, forms deposits in people with chronic inflammation, most often rheumatoid arthritis o In primary AL amyloidosis, excess light chains are made by messed up B cells, mostly lamba light chains o 1/10 of them have multiple myeloma o Amyloid fibrils can deposit in other organs too o When the kidneys are involved, it shows proteinuria in the nephrotic range, and sometimes renal vein thrombosis o Biopsy of the kidney shows diagnostic with positive Congo red staining positive stain for Ig light or heavy chains Hereditary amyloidosis is negative for that, and shows abnormal proteins being deposited Nonamyloid monoclonal Ig deposition diseases (MIDDs) – group of disorders that form Congo red negative depsoits o Light and heavy chain diseases with granular deposits that stain positive o Light chain nephropathy is most common and causes nephrotic syndrome, and most progress to ESRD The main light chain is k chains o Shows proteinuria, hematuria, and renal lesions Fabry disease – x linked globotriaosylceramide metabolism problem secondary to deficient lysosomal α-galactosidase A activity o It affects the vascular endothelium, nerve, heart, brain, and kidneys o Kidney symptoms include mild to moderate proteinuria, and sometimes microscopic hematuria or nephrotic syndrome o Renal biopsy is diagnostic with enlarged glomerular podocytes packed with vacuoles containing globotriaosylceramide, and focal and segmental sclerosis o Treat with recombinant α-galactosidase A Glomerular vascular syndromes: - Hypertensive nephrosclerosis o Only about 6% of people with systemic hypertension develop kidney disease o Up to 1/3 of people with ESRD have hypertensive nephrosclerosis as a primary cause Risk for hypertension and ESRD is higher in blacks o Patients present with hypertension, and sometimes microscopic hematuria o - - - - Episodes of malignant hypertension can be associated with acute kidney injury, nephrotic range proteinuria, or thrombi Cholesterol emboli – atherosclerosis can show cholesterol crystals in the kidney o Symptoms include hematuria, mild proteinuria, loss of renal function, eye problems, fever, eosinophilia, eosinophiluria, and low complement o Biopsy shows characteristic biconvex clefts in vessels Thrombotic thrombocytopenic purpura and hemolytic uremic syndrome o TTP and HUS share the same clinical features of thrombocytopenic purpura and microangiopathic hemolytic anemia, a combo called thrombotic microangiopathy, fever, acute renal failure, and neuro problems o HUS shows shiga toxin, which can cause diarrhea, which TTP doesn’t, but TTP does show neuro symptoms o Renal biopsy shows glomerular capillary endotheliosis with platelet thrombi and the formation of fibrin in and around the glomeruli Antiphospholipid antibody syndrome – systemic disease with antibodies to anionic phospholipids o Can be idiopathic or associated with systemic lupus, pregnancy, or other primary renal disease o Can have clots o Kidney injury happens in ¼ of cases, and shows acute renal failure, acute flank pain with renal vein thrombosis, or mild proteinuria and hematuria o Renal biopsy shows characteristic occluded vessels, ischemic mesangiolysis, and glomerulosclerosis Sickle cell disease – those homozygous with SS sickle cell anemia develop chronic occlusive disases that manifests in the kidney as hypostenuria early in disease o Over time you’ll see hematuria, hypertension, FSGS, interstitial nephritis, renal infarction, or MPGN Viruses involved in kidney disease are HIV, HCV, HBV, parvovirus, polyomavirus, cytomegalovirus, hantovrius, and coronavirus - HIV associated nephropathy presents after at least 2-3 years of HIV infection and is more common in blacks There is no hypertension, and kidney size is fine Most often, renal biopsy shows FSGS, usually the collapsing form HCV is strongly associated with MPGN type 1 or mixed IgG and IgM cryoglobulinemia