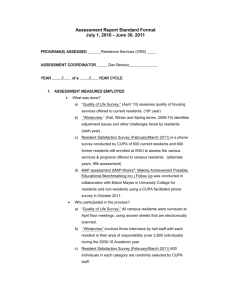
Internal Med
advertisement

Department of Psychiatry and Human Behavior Rhode Island Hospital Revised Date: 2/11/09 General Medicine Wards: B Overview of Rotation The General Internal Medicine Ward Rotation at RIH is a core inpatient experience during which interns and residents gain knowledge, skills and practice in the care of acutely ill hospitalized patients. The rotation requires a high degree of organization and efficiency, as well as a strong commitment to professionalism. This latter quality is a core competency, which will guide residents in decision-making on behalf their patients, as well as their own education. Description of Ward Rotation Teams: There are eight teams on per month at RIH. Teams are equally divided between Med A and Med B so that one of each is on every call day. Med A teams admit subspecialty patients who have a relationship with an attending of that subspecialty (renal, geriatrics, primary care, or hematology/oncology). Med B teams care for “unassigned” service patients, patients of the medical primary care clinic, and patients of the Women’s Health / Primary Care group. Med B patients are assigned to the General Internal Medicine Service attending for that team as the patient’s attending of record. The Med B attending conducts attending rounds, combined management and teaching rounds with their teams, provides feedback and is responsible for evaluations. Call Cycle: On each day there are two teams on call (one Med A and one Med B). Each team consists of one resident (2nd or 3rd year) and one or two interns. In addition there may be a 3 rd or 4th year medical student and/or a pharmacy student. This rotation is designed around the “go home at night” model with each team on call every 4th night (q4). During “on-call” days each team admits up to 5 patients per intern/10 patients per resident and leaves hospital in the evening, signing out to the night float team. There are generally no admissions on “post-call” days. The following day is “short-call” day during which each team admits 2 new patients per intern. These patients will have been admitted overnight by the second year night float. There are generally no admissions on the fourth day in the cycle, “pre-call” day. Per the admission algorithm, the cap is five admissions per on-call intern. On short call days, the cap is two per intern. ACGME guidelines permit interns to accept up to two additional patients as transfers from other medical services (i.e. MICU transfers, patients on a non-teaching service that become teaching); these patients are preferentially distributed to the on call team. Short call admissions will have been worked up and admitted by the night float resident. Sign out and cross-coverage: During the first half of the academic year, formal sign out rounds will take place every evening in the Residents lounge between 4:30 and 5pm. All teams are responsible for remaining in the hospital until this time. On-call teams will take sign out from teams going home and provide cross-coverage for their patients until 8pm. The interns on-call will carry the cross-cover beepers (Med A or B) during the entire day but will not provide cross-coverage until after sign-out. At 8pm the night float teams arrive and the on-call interns sign out all patients to the night float interns. The NF1’s will carry the cross-cover beepers. Though on-call teams sign-out at 8pm they will be continuing to work with their patients unit they leave the hospital. Good communication should exist between teams until the on-call team leaves the hospital. Use of the web sign-out system is required for all interns and sub-interns. Orientation to this system, as well as the goals and objectives of the rotation, will take place on the first day of the rotation for interns each month. Clinic Rule: PGY 2’s and PGY 3’s will attend a session of MPCU on the same day as their second site. This will be considered an "outpatient" day and there will be day float coverage for your patients in-house. When you are on call at RIH on your designated clinic day, clinic will be rescheduled to the day before the call day unless your clinic day falls on a Monday on which you are on call, in which case you will make up that clinic on the following pre-call day (Thursday). PGY 1’s come to clinic on their regular day at an afternoon session. When you are on call, the above rules apply regarding rescheduling of clinic days. Code Team: From 8a-8p, the On Call Teams will respond to all codes; from 8p-8a the Night Float Team will respond to all codes. Code pagers will be carried by the on-call residents, NF3, and NF2. I. GENERAL INFORMATION Name of Rotation Course Director Duration of Rotation Address/Institution Telephone/FAX Administrative/Secretarial Contact and Phone Chief Residents Location to report on First Day of Rotation Resident Study/Resource Area General Medicine Wards: Med B Dominick Tammaro, MD one month, no vacation Rhode Island Hospital 444-4083/444-3056 Terry Bomba, 444-4083 444-5990, 444-4980 Jane Brown (JB) Conference Room for orientation - see intranet schedule. JB Resident Conference Suite, Resident Library, Computer Resource Room 1 II. FACULTY The following is a list of the faculty in this Division or Department who attend on this rotation. Drs. Anvar, Babb, Bledsoe, Cyr, Duffy, Fagan, Gardner, Gupta, Jeremiah, Maher, Mathews, McGarry, McGillen, Moulton, Ofstead, Sapers, Schleinitz, Schwartzwald, Tammaro, Warrier, Wu Please note that fellows and/or chief medical residents may participate in this rotation in a teaching and supervisory role. Lines of Responsibility (in order): Interns are the primary care providers for all patients on their services. When they are unavailable (night, days off, continuity clinic), the intern will sign over responsibility to their resident, night float, or day float as appropriate. Interns are responsible for primary documentation of patient evaluation & management in the patient record. All interns are supervised by their resident or, in the case of a resident’s day in the ambulatory setting, a designated day float. The resident must approve all plans set forth by the intern and be contacted for any change in management plan or intervention. Residents and interns are supervised by the attending of record and/or teaching attending for the patient, who will collaborate and confirm/modify the team’s plans while providing patient-centered clinical teaching. DGIM faculty at RIH supervise housestaff on Med B and are available 24 hours/7 days/week by pager (on-call schedule with pager numbers on Residency Intranet Website). The attending of record has ultimate responsibility for the patient. Chief Residents are program director/chief of service designees who provide guidance and, where appropriate, back-up supervision of the intern or resident in the event that assistance is necessary. The resident or intern will contact the chief resident at the specific institution during the day (or the chief resident on-call at night - on-call schedule with pager numbers on Residency Website) when such assistance is required. Chief of Service (RIH Tammaro, TMH Schiffman, PVAMC Rounds/Charles) are available for assistance either directly to the resident or through the chief resident. III. TOPICS/TEACHING METHODS/MATERIALS USED DURING THIS ROTATION Topics to be covered are based upon: the patient population cared for by the team over the course of the month-long rotation and the noon conference schedule for the month. cases selected for presentation and Discussion at Morning Report and Attending Rounds Principal teaching methods: Attending Rounds Intern Conference Combined Management/Teaching Rounds Morning Report Post-Call Questions – each resident will research the answer to one question that came up on a previous call and present this at the resident’s morning report. Scheduled by the CMRs. Ethics Conference - one session per month per team in place of attending rounds; scheduled by CMRs Clinical Evaluation Exercise - Med B attending conducts for interns on short call day Noon Conference – see curriculum/topic list by subspecialty, as well as schedule, on residency home page intranet site. Monthly Mortality Review Sessions - review of all deaths on medical services Pathology Review Session - once monthly during noon conference; review of all pathology specimens from patients each month. MAR Conference – Medical Admitting Residents Conduct noon conference on topics relevant to triage decision-making Journal Club – review of current literature and critical appraisal skills – conducted 2x/month at RIH, TMH, PVAMC Educational materials provided/referred to residents: Reading and Reading Lists: Each attending and resident is expected to utilize current medical literature in the planning of therapeutic and diagnostic interventions. References are reviewed based upon the need for specific information as well as the need for general reviews. Attendings, chief residents, consultants, and residents will search for and obtain necessary literature and share such references with the rest of the physician team. Computer-assisted educational materials: All housestaff have access to full-text literature search and retrieval capacity through the hospital computer network. Terminals are located on all floors in all clinical areas. Other: Residents have access to radiology, pulmonary and hematology teaching files. 2 IV. SPECIFIC AREAS & EXPECTATIONS Residents are expected to regularly review relevant pathologic specimens (examples: bone marrow, biopsy, autopsy) laboratory specimens (blood smears, microbiologic specimens) biopsy and autopsy specimens on their patients. Diagnostic imaging studies – either online via PACS or in the radiology department with radiologists as the situation warrants On this rotation, residents do not act as consultants to other clinical services such as surgery or psychiatry. Such responsibility comes under the senior resident consultant and attending team. Among the attendings' responsibilities is the application of cost-effective care measures and principles to the actual care of the patients on the medical service. Residents are expected to communicate as needed with discharge planning specialists. V. EVALUATIONS Evaluation of the resident's successful completion of the goals outlined below will be carried out by the attending and intern. Evaluation of the intern's successful completion of the goals outlined below will be carried out by the attending and resident. Evaluation of the attending's successful completion of the goals outlined below will be carried out by the resident and intern Evaluation of the rotation will be carried out at the end of the month by the intern and resident. VI. RESPONSIBILITIES OF ATTENDING ON ROTATION The attending assigned to each Med B team serves as the attending of record for all patients on that team. The attending assigned to each Med B team will see all patients within 24 hours of admission and will supervise the care of the patient by the housestaff, offering guidance but allowing for autonomy. Such supervision will be in accordance with the Department of Medicine Policy on Resident Supervision. The attending will be available for or be present at all team activities where their involvement is needed. The attending assigned to each Med B team will document all initial patient visits, follow-up visits and all other patient interactions with documentation in the medical record in compliance with guidelines established by Medicare. The attending will conduct teaching rounds no less than 4½ hours per week. Each attending rounds must include either (a) bedside interaction with the patient under discussion as part of the educational session, or (b) the continuation of a discussion initiated at the bedside of the patient under discussion on a previous interaction. All attending rounds must be (a) based upon issues raised by patients being cared for by the team, (b) timely in relevance to the care of the patient being discussed, and (c) be attended by all members of the ward team, unless excused for clinic or urgent time-sensitive patient needs. Each Med B attending will conduct a Mini-CEX on each intern and resident who has not already had one performed during that year, unless instructed to do so by the program director (i.e., to track progress of a remediation program). CEX examination of interns or residents already examined is optional. Each Med B attending will make rounds with the entire team on the day following the admitting day for that team. The attending will hear case presentation by interns and students, see all new admissions (as well as any other patients requested by the housestaff), discuss diagnostic and therapeutic strategy with the team, and document their findings in the record. The attending will provide timely, specific, constructive and balanced feedback to all housestaff and student members of the team no less than twice monthly with the first feedback session no later than the mid-point of the month. The attending will, at the conclusion of the month-long assignment, complete an evaluation on each intern, resident and student. The evaluations should be discussed with the subject before submission to the program or clerkship director. The attending will be responsible for the educational content of the month-long experience. Attending writes no orders in the chart pertaining to patient care activities without proper communication or collaboration with team or covering housestaff, unless in emergency situations. 3 VII. RESPONSIBILITIES OF RESIDENT ON ROTATION PGY 1 Intern will pre-round on patients before and during AM Report in preparation for team rounds. Intern, together with resident, will receive report on short-call admissions prior to AM Report from Night Float Intern serves as primary provider for all patients assigned to him/her. Intern is responsible for initial evaluation of the newly hospitalized patient, documenting a full admission history and physical examination on the Department of Medicine standard admission form, and writing all admission orders utilizing the Physician Order Management System (POM). The intern is responsible for communicating with the patient’s primary care physician. This should involve a discussion at admission and at discharge with the outpatient physician. The intern will obtain consults as needed from subspecialists and should speak with them directly via page with specific clinical questions regarding their patients. Intern is responsible for examining and monitoring the progress of their patients on a daily basis, noting all laboratory and other data in a timely manner, discussing the management plans with the resident, and writing daily progress notes. Intern is responsible for collecting all relevant information on the patient, including reviewing old medical records. Intern is responsible for family and patient communication and should serve as liaison between the team and the patient. Intern presents all patient cases to the resident and attending on rounds, with exception if the patient is also cared for by a medical student in which case the student will present. Intern is responsible for performing all procedures (or observing those they have not yet performed under supervision) within the scope of the generalist on the patients for whom they are caring. Interns will keep a procedure log using the web-based procedure documentation system located on the Internal Medicine Residency Home Page. They will indicate their supervisor, level of proficiency, reason for procedure, outcome and complications, if any. Intern is responsible for the dictation of all discharge summaries on patients no more than 30 days following the discharge of each patient. Ideally, this will be done at the time of discharge. Intern is responsible for discharge paperwork and coordinating after-hospital care services (COC forms) on all patients. Interns will present cases at and attend intern conference on Fridays at Noon. Interns will attend noon conference, attending rounds and ethics conferences. Intern will admit no more than 5 new patients per admitting day and no more than 8 new patients in a 48-hour period. Intern will not be responsible for the on-going care of more than 12 patients at a given time. Intern will submit written evaluation of resident and attending and rotation upon completion of the rotation. Interns will comply with Duty Hours Policy. PGY 2 4 Resident will lead team rounds beginning after AM report. Team rounds should be conducted with both interns simultaneously. During morning rounds, the resident will guide the interns in setting the day's management agenda, including planning procedures, discharges and attending rounds presentations. Resident is responsible for supervising interns in the care of the patients assigned to that team. Resident will evaluate new patients by history, physical examination, and review of pertinent laboratory in a manner that does not compromise the intended autonomy of and independent evaluation by the intern. Resident will discuss the diagnostic and management strategy with intern on all new patients when the patient is admitted. Resident will document findings, impressions and plans for patient management in the patient record of all new patients admitted to them in a manner that complements, rather than duplicates the documentation of the intern. Resident is responsible for all initial and continuing dialogue with attending and consultants. This may increasingly be placed into the hands of the interns as the year progresses and the intern has greater presentation and analysis skills. Resident is required to attend and participate in AM report as scheduled. The resident is responsible for preparing cases for presentations, arranging with the Chief Residents when the presentation will occur, supplying pertinent literature to the Chief Residents in advance of the AM report, and participation in the discussion at AM report, including a discussion of follow-up information on previously presented patients. Residents must attend Noon Conference, Ethics Rounds, and Attending Rounds. Resident will incorporate the use of medical literature in management decisions. Resident will carry the code beeper as the code team's leader for the day. Resident will carry their intern's beeper when that intern is in clinic or at intern conference. Resident is the first line teacher of the interns. The residents' activities on the wards are expected to reflect this serious role. Residents should afford their interns sufficient autonomy so as to test their decision-making skills yet sufficient supervision to maintain quality of care. Remember that interns learn by the example taught by their resident. If you attend conferences, are an active participant in the educational aspects of residency, and consider your patients' needs above all other priorities in your work, you will teach your intern a great lesson. Resident will not be responsible for on-going care of more than 24 patients on a two-intern team, including sub-intern patients. Resident will not be responsible for admitting more than 10 new patients in an admitting day and no more than 16 new patients in a 48 hour period. Residents will sign out to the day float resident on the night or AM prior to their weekly ambulatory day. Residents will complete written evaluations of the interns and attending with whom they worked during the month. PGY 3 Identical to PGY 2. In addition, PGY-3 residents: Serve as resources to PGY2 residents new to this rotation during the first two quarters of the academic year Provide assistance to chief residents in selection of cases, literature and discussion process for AM report VIII. CONFERENCE AND CLINIC SCHEDULE DURING THIS ROTATION AM Report M, W, Th, F - required for all residents on ward teams, DF, NF 8-9AM Grand Rounds Tuesday at 8AM - required for all medical housestaff with the exception of those on critical care unit rotations Attending Rounds Daily. 10:30-11:45 - required for ward residents, interns and students. Noon Conference M, Tu, W, Th - required for all medical housestaff with the exception of those on critical care unit rotations Board Review Fridays at Noon Intern Conference Fridays at Noon - Residents hold intern pagers IX. OTHER IMPORTANT INFORMATION FOR RESIDENTS ON THIS ROTATION: Residents should be mindful of the unique opportunity with which they are presented during this rotation. In caring for sick, hospitalized patients in a supervised environment, you are being given the chance to study in a protected environment while caring for patients with the illnesses you are studying. We urge you to embrace your responsibilities and to study and teach based upon the needs of your patients. 5 X. GOALS AND EDUCATIONAL OBJECTIVES FOR THIS ROTATION Overall Goals To expose residents to a broad variety of patients and medical conditions in an acute care hospital setting. To promote independent learning skills among residents caring for acutely ill patients To provide an educational environment through Morning Report, Attending Rounds, Intern Conference, Ethics Conference and Noon Conferences that will permit resident to learn about conditions existing in their own patients, as well as those patients cared for by their peers. To promote independent decision-making behaviors consistent with the concept of supervised autonomy To promote professionalism among residents and interns, whereby residents will understand the importance of their roles as teachers. All housestaff will demonstrate an appreciation of the primacy of the patient's needs and autonomy. Competency-Based Goals: Patient Care Residents must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Common Goal: Gather essential and accurate information about their patients Objective: At the end of this rotation, the intern & resident should be able to obtain a complete history including a chief complaint, history of present illness, review of systems, past medical history, social history paying particular attention to cultural and religious beliefs, as well as a family history, developmental history, and list of medications, allergies, and vaccines. Objective: The intern & resident should access old medical records and obtain information pertaining to previous hospitalizations, clinic visits, laboratory work and studies from all available sources, including the patient, family and primary physician. Common Goal: Residents must be able to communicate effectively. Objective: The intern & resident should be able to present a history and physical exam in a clear and concise manner. Objective: The intern & resident should be able to explain to the patient & family the diagnosis, nature of the disease and the expected clinical course. Objective: The intern & resident should be able to effectively communicate medical information in a written format. Notes should be clear, legible, timely and provide content which accurately reflects the patient’s current status and planned management strategies. All notes should indicate time and date, and include a header indicating the role of the author. Common Goal: Demonstrate caring and respectful behaviors when interacting with patients and their families. Objective: The intern & resident will be observed interacting with patients and critiqued on this interaction. Common Goal: Counsel and educate patients and their families. Objective: The intern & resident will have experience explaining to the patient and their family the diagnosis, nature of the disease and the expected course. Med A&B Wards Specific Rotation Goals: Objective: Interns will provide comprehensive care for up to twelve hospitalized patients for which (s)he is the primary provider. Objective: Interns will assess severity of illness and develop prioritization skills necessary to make diagnostic and therapeutic interventions in a timely manner Objective: Interns will develop an appreciation for cost-efficient care, proper utilization of resources, the importance of after-hospital care planning, and patient autonomy Competency-Based Goals: Medical Knowledge Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care. Common Goal: Residents must know and apply the basic and clinical science pertinent to their patients. Objective: The resident will keep abreast of new scientific knowledge. This knowledge will be obtained via didactic sessions, Grand Rounds, critical review of scientific literature (e.g. journal clubs), computer and web-based resources. Objective: The resident will participate actively in assigned conferences and teaching rounds. These conferences will include medical, ethical, psychosocial issues, and culturally sensitive topics 6 Med A&B Wards Specific Rotation Goals: Objective: Interns will understand and apply basic principles of physiology and pathophysiology to common diseases; understand the diagnosis, prognosis and management options for these illnesses Objective: Interns will appreciate the importance of basic principles of bioethics in the care of their patients Objective: Interns and residents will appreciate and apply where necessary the basic legal principles by which society governs health care delivery – examples include responsibility to report child and elder abuse. Objective: Interns will develop/residents will refine skills necessary for the coordination of care among primary physicians and consultants Competency-Based Goals: Professionalism Residents must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. Common Goal: Residents must demonstrate respect, compassion, and integrity in their professional behavior Objective: Residents will ask patients/family members how they wish to be addressed; avoid addressing adults by first name unless specifically invited to do so. Objective: Residents will know and avoid breach of the boundaries of the physician/patient relationship, including but not limited to strict avoidance of sexual or romantic suggestiveness or involvement with patients/family members. Objective: Residents will operate with respect for patient confidentiality at all times. Common Goal: Residents must demonstrate responsiveness to the needs of patients and society that supercedes self interest. Objective: Residents will place patient safety and care above all competing considerations at all times. Objective: Residents will make reasonable efforts to act as advocates for their patients. Objective: Residents will place patient safety as their first priority without compromising their own safety or the safety of others that they are supervising. Common Goal: Residents must demonstrate a commitment to excellence and on-going professional development. Objective: Residents will participate regularly in required conferences, including Morning Report, intern conference, Grand Rounds, noon conference, journal club, board review, pathology conference, death review, MAR Conference. Common Goal: Residents must demonstrate sensitivity and responsiveness to patients’ culture, age, gender, disabilities, religion, sexual preference, and other parameters of human diversity. Objective: Residents will make every effort to elicit and to accommodate, to the fullest extent of their ability, differing religious and cultural needs and values in delivering medical care– but are under no obligation to accommodate requests based upon any form of identity-group prejudice. Objective: Residents will clearly and openly identify and repudiate statements of prejudice made by professional colleagues, and will not permit their actions as physicians to be influenced by such prejudice. Objective: Residents will cultivate the ability to identify and articulate their own cultural values and preferences, comforts and discomforts; and to be self aware in attempting to deliver fair and optimal medical care to all patients – including recognizing their obligation to transfer care to another physician should the occasion arise in which personal values or biases interfere with such care delivery to any patient or family. Objective: Residents will use language that is neutral as to assumptions of gender, sexual preference, religion, race/ethnicity, etc. when making general comments and explanations. Competency-Based Goals: Interpersonal and Communication Skills Residents must be able to demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, their patients’ families, and professional associates. Common Goal: Residents must create and sustain a therapeutic and ethically sound relationship with patients. 7 Objective: Residents will approach patients/families with a friendly, interested, and respectful demeanor. Objective: Residents will scrupulously maintain patient confidentiality, and specifically reassure patients/families of the confidentiality of their personal and medical information. Objective: Residents will know and be able to describe the proper boundaries of the physician/patient relationship, and will consistently and conscientiously avoid any breach of these boundaries. Common Goal: Residents must elicit and provide information using effective explanatory, questioning, and writing skills. (A) Explanatory Objective: Residents will make explanations in clear, common-parlance language, avoiding use of medical jargon, and using graphic aids (including informal sketches) where helpful to get points across. Objective: Residents will ask patient’s/family’s concerns and questions and address these specifically and directly to ensure that patient/family have received information in the desired degree of detail. Objective: Residents will clearly identify differences in patient/family and medical perspectives, bringing such differences into open discussion, and explaining the rationales for medical actions that differ from patient/family preferences and values. (B) Questioning Objective: Residents will demonstrate skill, clarity, and effectiveness in questioning patients/families, including: beginning each topical exploration with broad, open-ended questions and progressing to more directed questions and specific prompts; avoiding asking more than one question at a time; clarifying patients’/families’ unclear statements. (C) Writing Objective: Residents will write clearly and legibly when hand-writing instructions or other information for patients/families Objective: Residents will help to ensure that written or printed information for patients/families is language-congruent and literacy appropriate: using straightforward language and comprehensible and culturally appropriate illustration. Objective: Written communications in patient charts will effectively permit subsequent caregivers to understand the nature of the patient interaction and the goals and plans for the encounter as well as future encounters when applicable. Objective: Resident and Intern notes will be dated, timed and clearly indicate the role of the author. Common Goal: Residents must be able to work effectively with others as a member or leader of a health care team or other professional group Objective: Residents will complete timely and thorough oral and written documentation in patient records and communications to other members of patients’ care teams. Objective: Residents will act as teachers and educational mentors to medical students and interns, making optimal use of “teaching pearls” and “teachable moments;” instructing residents in the proper content and format for concise and organized patient presentation; helping students and interns to define patient care plans; and providing residents with timely and constructive evaluation and feedback. Objective: Residents will, as continuing residents themselves, actively seek the advice and knowledge of senior physicians and other parties with knowledge relevant to the care of patients (both in general and in specific individual instances). Objective: Residents will master the logistics and appropriate use of sub-specialty and specialty consults and their follow-up, including such non-medical resources as Social Work, Case Management, Ethics Committee, Risk Management, etc. Objective: Interns will be able to prepare and present case presentations and lead discussions at intern conference among peers Objective: Resident will prepare & present case presentations and lead in-depth discussions at AM report among peers and faculty. Objective: Resident will complete end-of-rotation evaluations and provide timely feedback for interns in order to direct their professional growth and development Competency-Based Goals: Practice Based Learning and Improvement Residents must be able to investigate and evaluate their patient care practices, appraise and assimilate scientific evidence, 8 and improve their patient care practices. Common Goal: Residents must be able to analyze, evaluate and improve their own practice performance, skill, and style. Objective: At the end of this rotation, the resident should be able to identify gaps in knowledge based upon experience, introspective awareness, and feedback for the month. The resident is expected to regularly review both textbook and primary source literature to maintain up to date understanding of specific topics that have arisen in practice. Objective: The resident should actively seek feedback and advice on practice from peers, mentors, staff, and patients alike to gain greater objective insight into their strengths and weaknesses. Common Goal: The resident will effectively use information technology to access and manage on-line medical information to support their education, expertise and certification. Objective: The resident will gain basic skills in literature search methodologies using standard web-based medical literature search engines such as Ovid, MD Consult, Pubmed. Objective: The resident will have familiarity with a variety of computer and hand-held computer based resources for looking up medications, dosing, and other topics of use to the general internist. Objective: The resident will utilize the resident based web page to document procedures, and changes in educational plans. Objective: The resident will actively participate in lectures and discussions with peers and experts on the topics related to the care of their patients. Objective: The resident is expected to take a proactive approach to enhancing their knowledge. The resident is expected to “think out loud”, ask for guidance, and actively seek input on their practice and knowledge base from their mentors. Competency-Based Goals: Systems-Based Practice Residents must demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value. By the end of their training, residents are expected to have attained competence in the following goals. Common Goal: The resident will understand how their patient care and other professional practices affect other health care professionals and the health care system, and how these elements of the system affect their own practice. Objective: The resident will learn how to work within a multidisciplinary team to develop a care plan for their patients. Objective: The resident will become familiar with hospital and community based health care professionals and their roles in groups such as social work, mental health professionals, PT, OT, dietitians, and VNA etc. Objective: The resident will evaluate how interacting with the above groups and health professionals affects their own practice. Common Goal: The Resident will advocate for quality patient care and assist patients in dealing with system based complexities. Objective: The resident will learn about a variety of insurances and how they affect patient referrals and prescriptions. They will learn the legal rights of the uninsured and will work with the appropriate services to assist patients who are under- or un-insured. Objective: The resident will learn how to interact and advocate effectively with other physicians, ancillary caregivers, community agencies, insurance companies, etc. when it affects the health of their patients. Objective: The resident will learn about the various community resources available for patients and will work with case managers and social workers to enable patients to access these resources. Objective: The resident will learn to work with translator services for optimal and appropriate patient care. Common Goal: The Resident will know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities affect system performance. Objective: The resident will maintain responsible communications by phone and letter with their patient’s primary care physician. Objective: The resident will learn how and when to appropriately refer patients to subspecialists and how to communicate effectively with the subspecialist. 9