Additional Supporting Information may be found in the online
advertisement

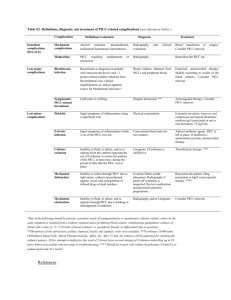
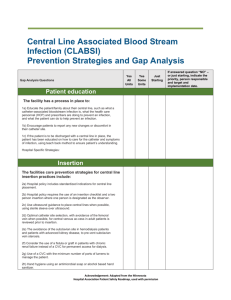
Additional Supporting Information may be found in the online version of this article: Table S I. Evidence-based better practices developed by a multidisciplinary task force for PICCs care at our centre (see references below) Category Specific PICCs care procedures Hand hygiene Hand washing with an alcohol-based “waterless” product before manipulation of catheter. Sterile barrier Usage of sterile material (sterile gloves, drapes, cap and mask) and chlorhexidine solutions or chlorhexidine sponges for catheter dressings (except patient’s contraindication). Skin preparation Skin and PICC exit site are aseptically cleaned with 2% chlorhexidine and allow dry for 2 minutes before manipulating PICCs insertion Trained nurses inserted the catheter under cardiac and respiratory monitoring and applying the maximum sterile conditions. Position was confirmed by chest radiography. We considered optimal if the tip was located at cavoatrial junction and acceptable anywhere in superior vena cava. Patients were referred to intensive care unit (ICU) team when was unsuccessful placing (two insertion attempts are allowed), or when had inadequate veins access. PICCs maintenance Catheters were secured to the skin with use of fixation transparent dressing and were covered with an occlusive gauze dressing. The dressings were replaced every 48h in hospitalized patients and every one to two weeks in outpatients or health centre; and always when dressings became damp, loose, etc. After each use and once weekly when not in use; were flushed using 6 ml of heparin solution (20 UI/ml). No antibiotic prophylaxis specifically was administered because no studies have demonstrated any reduction in CRBSI rates. There was no routine use of thromboprophylaxis while de PICC line was in situ. Removing the PICC as soon as the therapeutic goal has been reached or in cases of death or catheter related complication (see text for details). PICCs removal Catheters were removal under aseptically conditions according to these criteria: electively (end of therapy or completion of intensive phase of chemotherapy), death of patient, or due to related complications. PICCs were routinely cultured at removal. Patients and family education General and detailed information about PICC hygiene and care were given (emphasized hand hygiene). Specific information about PICC complications and rules of procedures in case of any sign/symptoms of complications were given. Staff education Educational workshops, including theoretical and practical aspects, addressed to every nurse and physician taking care of patients were performed every year since the beginning of program. Team PICC meetings Discussion about PICC-related complications rates ( CRBSI, CRT, etc); possible doubts or problems detected during the implementation of the program; as well as meetings of the group of infection control were performed on a 3-month basis to evaluate PICC-related complication rates, adherence to the intervention program and to discuss possible changes. PICCs registration All patients were examined daily or every one to two weeks in the outpatient clinic for symptoms or signs suggestive of any complications while PICC was still in place. Incidences happened were registered by nursery and leaders physicians’ team. PICC- peripheral inserted central catheter, CRBSI- catheter related bloodstream infection, CRT- catheter related thrombosis. References 1. 2. O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad II, Randolph AG, Rupp ME, Saint S, Healthcare Infection Control Practices Advisory Committee (HICPAC). (2011) Guidelines for the prevention of intravascular catheter-related infections. Clinical Infectious Diseases, 52, e162-93. Alexander M. (2011). The new gold standard in infusion nursing. Journal of Infusion Nursing, 34(1), 11. 3. Maki DG, Weise CE, Sarafin HW. (1977) A semiquantitative culture method for identifying intravenous- catheter-related infection. New England Journal of Medicine, 296(23), 1305-9. 4. Ljungman P, Hägglund H, Björkstrand B, Lönnqvist B, Ringdén O. (1997) Peroperative teicoplanin for prevention of gram-positive infections in neutropenic patients with indwelling central venous catheters: a randomized, controlled study. Support Care Cancer, (6), 485-8. 5. Jeffries HE, Mason W, Brewer M, Oakes KL, Muñoz EI, Gornick W, Flowers LD, Mullen JE, Gilliam CH, Fustar S, Thurm CW, Logsdon T, Jarvis WR.(2009) Prevention of central venous catheter-associated bloodstream infections in pediatric intensive care units: a performance improvement collaborative. Infection Control and Hospital Epidemiology, (7), 645-51. 6. Møller T, Borregaard N, Tvede M, Adamsen L. (2005). Patient education-a strategy for prevention of infections caused by permanent central venous catheters in patients with haematological malignancies: a randomized clinical trial. Journal of Hospital Infection, (4), 330-41. 7. Pascual A., Bouza E., Liñares J. (2004) Procedimientos en Microbiología Clínica. Recomendaciones de la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica.