Vascular Access Devices: PICC & Central Catheter Management
advertisement

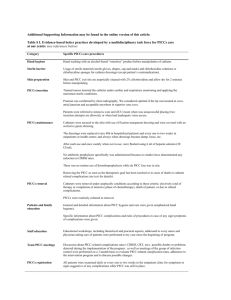
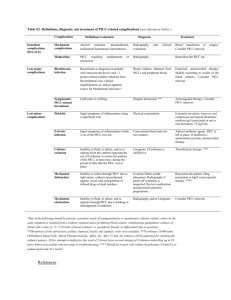
Vascular Access at MUSC Lynn Williams, RN Vascular Access Resource Nurse Specialty Nursing Department Vascular Access Devices 2013 Objectives: •Intro to Infusion Nursing Society (INS) •Identify common types of venous access devices, inc general characteristics •Discuss device selection & placement departments •Review assessment, care and management of central venous access devices – C75 Central Venous Catheter Policy •Identify potential complications and related interventions regarding a central venous access device Infusion Nursing Society (INS) Recognized as the global authority in infusion nursing, dedicated to exceeding the public’s expectations of excellence by setting the standard for infusion care. The Standards of Practice are written to be applicable in all patient settings & address all patient populations. Be advised – the “Standards” is a legally recognized document. General Characteristics of CVAD Catheter Materials Polyurethane, Silicone, Impregnated, FDA approved for Power injection of IV contrast during radiological imaging French Sizes 1.2 fr – 15 fr Lumens Single, double, triple, & quad available *Golden rule – Less is more! Cuffed vs non-cuffed Valves Internal (tip) – Groshong External (hub) – PASV, Solo Power PICC 4 Choosing the Best VAD for Each Patient • • • • • • Diagnosis Prescribed therapy Duration of therapy Physical assessment Patient health history Support system/resources – Case Managers • Patient preference 5 List of drugs that d/t pH, osmolality or chemical structure, cause frequent IV restarts • Amphotericin-irritant • • Bactrim - pH 10.0 • • Calcium Gluconate – Hypertonic • • Chemo Vesicants- pH • Ciprofloxacin – pH 3.3 • • • Dilantin – pH 12.0 • Dobutamine – pH 2.5 • • Erthromycin – irritant • • Morphine(PCA) – pH 2.5 All Penicillins – pH 10/hypertonic Phenergan – pH 4.0 Potassium >20 KCL – Hypertonic PPN/TPN – Hypertonic Rocephin – Irritant/hypertonic Tobramycin – pH 3.0 Vancomycin – pH 2.4 Selection of Catheters and Sites CDC Recommendations Catheters & Site selection PIV vs PICC: Use a peripherally inserted central catheter (PICC) when the duration of IV Therapy will likely exceed six days Weigh the risks/benefits of placing a central venous device (CVD) at a recommended site to reduce infectious vs mechanical complications (IJ vs Subcl vs femoral) Catheter & Site Selection cont’d Choose a device with the minimum # of lumens/chambers essential for treatment Promptly remove catheters that are no longer essential Central Venous Access Devices • Peripherally Inserted Central Catheters (PICC) – Regular & cuffed/tunneled • Non-tunneled/Non-cuffed Central Catheters • Tunneled/Cuffed Central Catheters • Implanted Ports – regular vs power 10 Departments that Place &/or Manage CVAD’s • VAIN Team – Bedside PICC & difficult PIV insertion – Screen all Adult IP PICC orders – Adults • Interventional Radiology Dept. – Place all types of venous access devices – All ages • Infectious Disease PICC Service – Place both cuffed & regular PICCs – Bronch Lab, EP, Cath Lab – Adults • OR/Surgeons – All ages – All devices EXCEPT PICCs • Pediatric Services – Procedural area on 5th floor of CH – PICCs – Bedside PICCs by specialized RNs in ICUs Peripherally Inserted Central Catheters PICCs • Usually inserted using a vein in upper arm • Can be used for most IV therapies and to obtain blood draws • Select for pt’s requiring IV abx’s, TPN, poor IV access needing frequent blood draws • Easily removed either at bedside while an IP or by a Home Health Nurse after discharge • FYI – if pt has no insurance, they are unable to have device cared for at home Adult PICC White Board • All Adult PICC orders go to the VAIN team for evaluation and dept assignment for device insertion • White Board provides info r/t which dept is assigned to insert PICC w/ comments • Certain criteria dictate which dept is best suited to place the PICC: occlusion history, sedation, complicated diagnosis • Found on the Intranet PICCs Placed at MUSC BARD Power PICC (polyurethane) Cook Silastic PICCs Cook Spectrum (polyurethane, Abx impregnated) Centrally Inserted Catheter • Non-Tunneled CVC (no cuff) – Short term, Acute care, percutaneous catheters – Typically used for days – weeks for all types of IV therapy, blood draws, monitor central venous pressure in ICUs – Example: PICCs, Acute single/dual/triple/Quad CVCs, Dialysis/aPheresis catheters • Tunneled CVC (cuffed) – Long term therapies – TPN, chemo • Oncology, Cardiac, GI patients – Dacron cuff provides catheter stability and serves as a barrier to prevent infection – Examples: Cuffed PICCs, Chronic Dialysis/aPheresis catheters, Hickman, Broviac, 18 Tunneled IJ entry site Subcutaneous Tunnel w/ cuff Non-tunneled IJ entry site No subcutaneous Tunnel or cuff Implantable Ports Implantable Ports Implanted Ports - Plastic, stainless steel or titanium housing attached to a catheter implanted under the skin - Chest, Arm, Thigh, Abdomen - Completely under skin – swimming permitted when not accessed once the incision has totally healed - Requires special non-coring needles to access - Available as power injectable - Can remain in place for years - Sickle cell, Oncology, Rheumatoid Arthritis, intermittent long term tx’s 21 Identifying Power Ports • Prior to a fluoroscopic exam requiring power injection of contrast: – Clinical staff (radiology techs, RNs) will positively ID device • Manufacturers ID card, arm bracelet, key tag • Manufacturers sticker found on IR/OR document • Image – view “CT” marker on port chamber – Radiologist to review prior image before being used – If no prior image, an image of the appropriate anatomic area will be done & reviewed by Radiologist • Radiology Dept. has a process they follow to confirm if a device is power injectable. Port Needle Sets Before Meds can be administered via CVAD: • Verify tip location using fluoroscopy – For newly placed devices – Transferred patients with an indwelling central venous catheter – If there is a known or questionable change in catheter position • Migration or dislodgement suspected • Securement device has become dislodged • S/S: No blood return &/or unable to flush If no blood return, device is not to be used until evaluated/treated for clot/thrombus or mechanical issues! IV Flush Orders • Practitioner must write order for heparin flushes • Standard Adult and Pediatric flush orders • Each device has a standard flushing protocol including 0.9% sodium chloride and heparin • If heparin is contraindicated, consider alternative, such as argatroban or tPA • When patient is admitted with a device, initiate the order for RN to get heparin Dialysis/aPheresis catheters • Locked with high-dose heparin – Refer to IV Flush Orders – Adults: Use 1000u/ml heparin – Pediatrics: Use 100u/ml heparin • May only be accessed by nurses trained to do so (ICU, aPheresis & Dialysis RNs) • Renal service must be consulted before using catheter. If no longer being used for aPheresis &/or dialysis, the Renal MD MUST transfer care to RNs on unit. Post-Insertion Complications • • • • Catheter Dislodgement Catheter Migration Air Embolism Catheter-related Bloodstream Infection • Venous Thrombosis • Catheter Occlusion 28 Catheter Dislodgement • Stabilization devices (Statlock, sutures, securement dressings) are used to prevent catheter from falling out, catheter tip malposition, and migration of bacteria • If displacement is suspected, CXR is required to verify tip placement • S/S of dislodgement – catheter malfunctioning, securement device lose, device is semi-pulled out • Do not try to re-insert the device 29 Catheter Migration • Tip can spontaneously migrate into right atrium or internal jugular • May result from coughing, ventilator, forceful flushing, heavy lifting, hypertension • S/S = Inability to flush, infuse or aspirate • “Ear gurgling” or “running stream” while catheter is being flushed • Get a chest x-ray 30 Catheter Tip Malposition Catheter tip right jugular Catheter Related Bloodstream Infections (CRBSI) During CVC insertion – use maximal sterile barrier precautions: Cap, mask, sterile gown, sterile gloves, sterile full body drape Put mask on if removing a dressing to inspect a site Prep skin using Chlorhexidine gluconate w/ alcohol – allow to dry!! Assess catheter necessity daily! Venous Thrombosis • Diagnosed via Vascular Ultrasound • What do you do?? – Before removal, consider this: • • • • Is the catheter functioning normally? Are symptoms manageable? Can patient receive anticoagulant treatment? Does patient have known occluded vessels that will compromise a new device plcmt in the future? • Consider patients condition, long term treatment and the need for the existing device Occlusion Management • Partial Occlusion: device flushes, no blood return • Total Occlusion: No flush or aspiration via device • Both types of occlusions can safely be treated with Cathflo Activase (alteplase) – If mechanical malfunction has been ruled out, order Cathflo for catheter occlusion – Follow Occlusion Management guidelines (Appendix B in C75 Policy) Device Removal • RNs have to demonstrate competency to remove a non-tunneled catheter. – RN competency is based on skill & frequency of performance • ONLY dialysis or ICU RNs w/ demonstrated competency may remove large bore catheters (dialysis/aphersis) • ONLY MDs and non-surgical specialist that are credentialed may remove cuffed devices, including PICCs. Air embolism = entry of a bolus of air into the vascular system; can occur during placement or after device removal Reduce the risk of embolism: • Place the patient in Trendelenberg position to increase intrathoracic pressure, unless not tolerated or contraindicated • Have patient hold breath and gently bear down (Valsalva). • Sx’s & Sx’s include: palpitations, resp distress, hypotension, arrhythmias, Non healing site over port! Post port plcmt – bruising! Extravasation CDC Recommendations Educate/training clinicians who insert/maintain cath’s – *SIM Lab program being developed Use maximal sterile barrier precautions Use >0.5% chlorhexidine skin prep w/ alcohol (ChloraPrep = 2% = isopropyl alcohol) Avoid routine replcmt of CVCs as strategy to prevent infection Periodically assess knowledge of & adherence to guidelines Central Venous Catheter Policy • Owner: Central Venous Access Committee – Multidisciplinary team • Purpose: Provide guidelines for the insertion & care of all VADs • For all staff that handle or insert a Central VAD • Includes: – 8 Appendix Included: References, VAD Occlusion Mgmt, IV Flush Orders (Peds/Adults), CVL Guideline, Ethanol Lock Info Sheet, VAIN Team Guidelines Questions??? Lynn Williams, RN Vascular Access Resource Nurse 792-1143 11109