Line Infections - Clinical Departments
advertisement

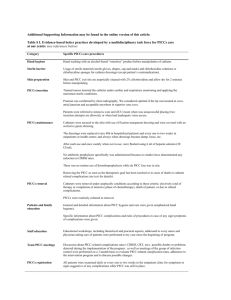
LEARNING OBJECTIVES 1. Differentiate types of infection associated with vascular access 2. Formulate appropriate empiric therapy based on patient specific risk factors 3. Recite indications for antibiotic lock therapy 4. Prescribe appropriate antibiotic therapy based on culture results KEY MESSAGES 1. Catheter related bloodstream infection (CRBSI) is defined as growth of the same microorganism in blood drawn from a percutaneous stick and from an intravenous catheter. 2. The treatment of line infections depends on type of catheter and microorganism. 3. Antibiotic lock therapy is used to salvage long term catheters infected in certain circumstances. INTRODUCTION >150,000 devices purchased annually by US hospitals >100,000 deaths $6.5 billion cost Result in average LOS of 12 days longer in hospital PATHOPHYSIOLOGY How do these infections happen? 1. Migration of skin flora from insertion site 2. Direct contamination of catheter 3. Hematogenous seeding 4. Contaminated infusate RISK FACTORS Risk varies based on: Type of device Midline catheters 0.2% PIV 0.5% PICC 1.1% Tunneled cvc 1.6% Noncuffed cvc 1.7/2.7% PA catheters 3.7% Use of device Insertion site (femoral>IJ>SC) RISK FACTORS Risk varies based on: Duration of catheter PIV 3-5 days CVC >6 days PA catheter >3-4 days Frequency of accesses Use of prevention strategies Experience and skill of individual Patient factors ASK 3 MAIN QUESTIONS 1. What is the nature of the infection? 2. What type of catheter is infected? 3. What is the organism? DEFINITIONS WHAT IS A CATHETER RELATED BLOODSTREAM INFECTION (CRBSI)? What is a CRBSI? Growth of same organism from percutaneous blood culture and catheter What is not a CRBSI? Catheter colonization Phlebitis Exit site infection Tunnel Infection Pocket infection MORE DEFINITIONS Catheter colonization-growth of organism from tip, hub or sq segment of catheter Phlebitis-redness, warmth, tenderness along tract of catheterized vein Exit site infection-redness, tenderness or exudate with growth at exit site Pocket infection-infected fluid in pocket of totally implanted device Tunnel infection-pain, redness, >2cm from catheter exit site along sq tract of tunneled catheter Complicated Infection-metastatic foci of bloodstream infection ASK 3 MAIN QUESTIONS 1. What is the nature of the infection? 2. What type of catheter is infected? 3. What is the organism? TYPES OF CATHETERS PERIPHERAL IV M ID LIN E C AT HE T E R TYPES OF CATHETERS SHORT TERM CVC PA C AT HE T E R TYPES OF CATHETERS PICC TYPES OF CATHETERS TOTA L LY I M P L A N TA B L E DEVICE LONG TERM CVC ASK 3 MAIN QUESTIONS 1. What is the nature of the infection? 2. What type of catheter is infected? 3. What is the organism? EMPIRIC TREATMENT COVERAGE FOR BACTERIA Empiric treatment with vanc or dapto depending on hospitals mrsa mic data Do not use linezolid empirically Empiric GNR coverage should be based on severity of disease and presence of femoral line Use cefepime, carbapenem, or zosyn if warranted Only empirically double cover MDR GNR if pt is one of the following neutropenic severely septic colonized/recently infected with mdr gnr Add aminoglycoside if warranted EMPIRIC TREATMENT COVERAGE FOR CANDIDA Only empirically cover candida if pt is septic AND one of the following TPN prolonged broad spectrum abx hematologic malignancy transplant pt femoral site pt colonized with candida at multiple sites Use echinocandin OR fluconazole if pt has had no azole exposure in past 3 months MICROBE SPECIFIC TREATMENT COAG NEGATIVE STAPH Nafcillin/oxacillin for msse Vancomycin for mrse Treat for 5-7 days with antibiotics if catheter removed Treat 10-14 days with abx lock if catheter is salvaged Some say ok to not treat if catheter is removed, pt has no hardware, and blood cx negative after catheter removal MICROBE SPECIFIC TREATMENT STAPH AUREUS Always remove catheter Nafcillin/oxacillin for mssa Vanco/dapto for mrsa Default duration of therapy is 4-6 weeks Treat 14 days if all following apply pt not immunosuppressed catheter is removed no intravascular devices or grafts tee negative no evidence of metastatic infx bacteremia resolves after 72 hours on abx Treat 5-7 days for tip cx positive/perc blood cx negative situations MICROBE SPECIFIC TREATMENT ENTEROCOCCUS Ampicillin is drug of choice if susceptible Vanco if resistant to amp Double coverage with aminoglycoside is controversial 7-14 course of therapy recommended Only tee if other signs and symptoms of endocarditis MICROBE SPECIFIC TREATMENT GRAM NEGATIVE BACILLI Carbapenem ok for all following ESBL + ecoli/klebsiella enterobacter serratia acinetobacter ESBL – e. coli/klebsiella-use 3rd gen cephalosporin Psuedomonas-4th gen cephalosporin, carbapenem, zosyn, +/- aminoglycoside Stenotrophomonas- bactrim 3-5mg/kg q8hr De-escalate asap Duration of therapy 7-14 days MICROBE SPECIFIC TREATMENT CANDIDA Always remove catheter (tunneled hd catheter can be exchanged over wire) C. Glabrata and C. krusei use echinocandins C. Albicans use fluconazole 400mg qd ANTIBIOTIC LOCK THERAPY WHAT IS IT AND WHO CAN GET IT? ANTIBIOTIC LOCK THERAPY WHAT IS IT AND WHO CAN GET IT? For pts with long term cvc’s and uncomplicated crbsi Always use with systemic abx If abx lock not available, give systemic abx through the lumen of the infected catheter Not for candida or staph aureus crbsi Not for complicated crbsi, exit site or tunnel infx, or infx with persistent + blood cx after >72 hours of appropriate abx therapy PEARLS AND PITFALLS PEARLS AND PITFALLS Only culture if infection is suspected Culture before starting abx The first day cultures are negative is day one of abx If unable to obtain percutaneous blood cultures, drawn cultures from 2 lumens of line Arterial lines follow the same rules as temporary cvc’s PEARLS AND PITFALLS Do not remove catheters based on fever alone Do not change over guidewire routinely to prevent infection If you exchange a catheter over a guide wire and the tip and perc blood cx come back +, you must remove catheter and do fresh stick When removing the line for suspected crbsi, culture the tip, not the sq segment For PA catheters culture the introducer tip PREVENTION Only place line if necessary, use least risky line in the least risky place that will accomplish your goals Use full body drape and aseptic technique Prophylactic systemic abx are not indicated For pts with hx of crbsi abx lock may be indicated for prevention Education, education, education Checklists TREATMENT ALGORITHM SUSPECTED CRBSI TREATMENT ALGORITHM DOCUMENTED CRBSI IN SHORT-TERM CVC TREATMENT ALGORITHM DOCUMENTED CRBSI IN LONG TERM CVC TREATMENT ALOGRITHM SUSPECTED TUNNELED HD CATHETER INFX REFERENCE Mermel LA, Allon M, et al. Clinical Practice Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infection: 2009 Update by the Infectious Diseases Society of America. Accessed on line at: http://www.idsociety.org/uploadedFiles/IDSA/GuidelinesPatient_Care/PDF_Library/Management%20IV%20Cath.pdf