H-13 INTRAVENOUS N-ACETYLCYSTEINE ADMINISTRATION IN
advertisement
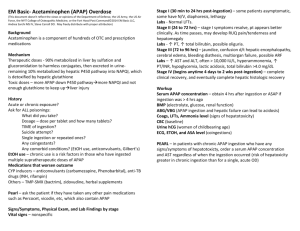
H-13 INTRAVENOUS N-ACETYLCYSTEINE ADMINISTRATION IN ACUTE LIVER INJURY Huynh Q*, Chen J, Marfo K Montefiore Medical Center the University Hospital for Albert Einstein College of Medicine 111 East 210th Street, Bronx, New York 10467 Purpose Acute liver failure (ALF) secondary to acute liver injury (ALI) is associated with high mortality rate and frequent need for transplantation. N-acetylcysteine (NAC) can prevent liver damage caused by acetaminophen (APAP) when given within 24 hours. In non-APAP ALI, NAC may improve hemodynamics, tissue oxygen delivery, and modify disease progression. We sought to evaluate a clinical protocol of NAC administration and its therapeutic benefits in ALI. Clinical outcomes of these patients with APAP induced ALI compared to patients with non-APAP induced ALI will be evaluated. Methods Medical records of adult patients who received continuous NAC infusion between August 1, 2010 and July 31, 2012 for ALI were retrospectively reviewed for baseline demographic characteristics including etiology of ALI, MELD scores on days 1 and 7, duration of therapy, total dose administered, and concomitant medications. Clinical outcomes after 7 days of therapy including changes in liver function tests, INR, serum creatinine, survival at discharge and 30days, and transplant-free survival were collected. Cost utilization analysis of treatment with NAC was determined based on patients’ length of hospital stay and drug acquisition cost. Due to the retrospective nature and design of the study, institutional review board and informed consent was not necessary to obtain. Summary of Results 46 patients in the APAP and 100 in the non-APAP groups received continuous IV NAC infusion for ALI for a mean duration of 25.9 and 29.9 hours, respectively with 48 (32.9%) of patients receiving >24 hours of therapy and 9 (6.2%) receiving >72 hours. Patients with ALI secondary to non-APAP etiologies were older, had more renal impairment, higher MELD scores, and longer LOS. IV NAC was well tolerated with no interruption of therapy due to adverse events and APAP and non-APAP ALI proved comparable in regards to reduction in AST and ALT. there was no difference in INR, serum creatinine, and MELD score observed in both groups. Survival was 97.8% and 82.0% at discharge, 96.2% and 70.0% at 7 days, and 92.9% and 65.4% at 30 days in the APAP and non-APAP groups, respectively with transplant-free survival valuing at 97.8% and 77.0% in the APAP and non-APAP groups, respectively. Only 1 in the APAP and 23 in the nonAPAP groups required liver transplants. Conclusions IV NAC is indicated to prevent APAP-induced ALI with some data supporting its use in nonAPAP etiologies. Although similar trends in measurable clinical values were seen with the use of IV NAC in both groups of our study, the lack of rigorous clinical methodology prevents us from drawing substantial conclusions. Further research must be done to describe the role of IV NAC in non-APAP ALI.